disc prolapse
Synonyms in a broader sense
- Disc prolapse
- Nucleus pulposus prolapse (NPP)
- Disc prolapse
- Protrusio
Related terms
- Sciatic pain
- Intervertebral disc bulge
- Disc protrusion
- Lumbago
- Low back pain / lumbago
- Lumboischialgia
- Back pain
- Intervertebral disc
English
- prolapsed intervertebral disc
- herniated disc

Definition of a herniated disc
Under a disc prolapse one understands the sudden or slowly increasing displacement or the emergence of tissue of the Nucleus pulposus (Gelatinous nucleus of the intervertebral disc) one Intervertebral disc backwards into the spinal canal (Spinal canal) or back-side (Nerve root). Here it can go through Irritation of the Nerve roots pain, paralysis and / or sensory disturbances occur. This can then become a Nerve root compression to lead. Herniated discs in the area of the Lumbar spine (Lumbar spine) occur much more frequently than herniated discs in the area of the Cervical spine (Cervical spine).
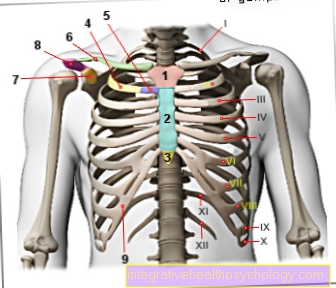
Illustration of a herniated disc

Disc prolapse -
Nucleus pulposus prolapse
A - herniated disc from the left
B - herniated disc from above
C - Healthy disc
a - neck and chest area
b - lumbar region
- Fiber ring -
Annulus fibrosus - Gelatinous core -
Nucleus pulposus
1st + 2nd intervertebral disc
(Intervertebral disc) -
Discus inter vertebralis - Spinal nerve -
Spinal nerve - Spinal cord -
Medula spinalis - Vertebral bodies -
Corpus vertebrae - Spinous process -
Spinous process
You can find an overview of all Dr-Gumpert images at: medical illustrations
What are the symptoms of a herniated disc?
Reference was already made above to the study, which showed that not every herniated disc inevitably causes discomfort in the form of back pain. If, however, complaints / symptoms occur in the context of a herniated disc, they are primarily due to the displacement of the gelatinous nucleus, which presses on individual nerve roots, on nerve fiber bundles (in the area of the lumbar spine) and / or the spinal cord.
In the following, the symptoms of the herniated disc will be discussed, which can turn out very differently due to pressure on the areas mentioned above.
Read more on the topic: pain in the back
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Symptoms of pressure against a nerve root
Pressure on nerve roots always triggers intense pain that can radiate into the arms and / or legs.
Learn more about the Disc herniation pain.
With this severe pain, sensory disorders and their consequences can also occur, one speaks of:
- Ant running
- Tingling sensation
- deafness
Depending on the stage and extent of the herniated disc, symptoms can also result in reduced muscle strength or even paralysis of individual muscle areas
Read more on this topic at:
- Consequences of a herniated disc
- Numbness from a herniated disc
- Herniated disc with nerve damage
Symptoms of pressure against the spinal cord
The symptoms vary depending on the location of the herniated disc. Herniated discs in the thoracic spine can cause sensory disturbances, cramps (Spasms) or even cause paralysis, whereas a herniated disc in the lumbar spine can cause bladder paralysis, for example. Paralysis of the leg muscles is also possible.
Symptoms of pressure against nerve fiber bundles, the horse's tail (cauda equina)
Lack of control of the bladder and rectum function, sensory disorders (e.g. numbness) in the anal and / or genital area inside the thighs, possibly associated with paralysis of the legs.
Read more on the topic
- Symptoms of a herniated disc
and even more special - Symptoms of a herniated disc of the lumbar spine
- Symptoms of a herniated disc of the cervical spine
- Symptoms of a herniated disc of the thoracic spine
causes
The intervertebral disc consists of a fiber ring with a gel-like core. If the fiber ring is weakened or cracked due to incorrect or overloading of the spine, the jelly-like core can escape from the intervertebral disc = disc prolapse. This usually happens due to wear and tear, so as risk factors for a herniated disc among other things obesity and pregnancy get ranked.
- in genetics
- the profession
- the statics of the spine (scoliosis, hollow back)
- Sports injuries
- Muscle weakness (muscular imbalance)
and - many more
to see.
Also read our page Herniated disc cause.
Prognosis of a herniated disc
One cannot make an exact prediction as to which Prognosis and course of a disc disease / herniated disc create.
Likewise, the duration of a herniated disc cannot be precisely named, as the course varies considerably from person to person.
The course and duration of the herniated disk also depends considerably on the location (cervical, thoracic, lumbar spine).
Older patients, however, tend to have more chronic pain, whereas younger patients with acute pain can assume long, pain-free intervals.
Modern treatment methods can also make a chronic disease tolerable for patients. The degree of improvement depends to a large extent on personal initiative. Physiotherapy applications provide effective support in the acute phase.
In most cases, conservative measures ensure complete freedom from symptoms after a herniated disc.
- Course of a herniated disc
- Duration of a herniated disc
How long does a herniated disc last?
Both the duration and the chances of recovery from a herniated disc are depending on the severity. The greater the expression of the leaked tissue the Intervertebral disc the longer it takes for this material to be broken down by the body, i.e. the more severe the herniated disc, the longer the healing process can take.
Usually the complaints should be within 6-8 weeks have passed. If it doesn't, the chances of successful conservative treatment decrease and it can lead to one Chronification of pain and discomfortcaused by the herniated disc. Especially with elderly patients chronic pain can often occur.
Prophylaxis / prevention
There is no specific preventive measure that fundamentally protects against a herniated disc. By changing and adapting the way of life, for example in the form of Strengthening of the back muscles and abdominal muscles by training on an adequate Power station, however, the risk can be reduced. From our and our experience, such a training is the best and most important prophylaxis.
Of course, change and adaptation also include a correct work posture for activities in professional life and in the household. For example, you should crouch heavy objects with you stretched back (ins Hollow back walk) to be lifted. When vacuuming, for example, an upright, relaxed working position can be achieved by adjusting the suction tube.
If you are mainly seated, it makes sense to get up and walk around at shorter intervals. There are also programs with relaxation and loosening exercises especially for this professional group. Ergonomic adjustment of the seating by means of height-adjustable seats and backrests can help to protect the spine. This is especially true for professional drivers.
A herniated disc cannot be completely prevented, but the risk can be through targeted training Core muscles targeted lower.
Read more complete information on this topic: How to prevent a herniated disc
Diagnosing a herniated disc
The Diagnosing a herniated disc includes various forms of physical and technical examination. In addition, diseases that have symptoms similar to the herniated disc must also be included in a Differential diagnostics be excluded.
Neurological examination
To diagnose or rule out a Herniated disc a detailed neurological examination is necessary. You can use differential diagnosis, for example, a Circulatory disorder of the legs, the so-called Intermittent claudication (= Claudicatio intermittens) exclude.
In addition, conclusions can be drawn about the location, severity and involvement of the nerves.
A neurological exam will check that Reflexes, the mobility, as well as the sensitivity, can also be a measurement of the Nerve conduction velocity include. This is particularly important when the severity of the herniated disc is to be assessed and it is to be checked which nerve roots are affected or whether there is a circulatory disorder.
Conventional X-ray diagnostics (X-ray image)
Recordings in two planes:
By means of a X-raythat are in at least two levels (from the front, from the side) should be carried out, one can see the bony structure of the Spine judge.
It is also possible to X-ray the patient as part of a functional recording. These special recordings, which are carried out in an inclined position, allow conclusions to be drawn about the mobility of the spine.
The problem of diagnosing a herniated disc through an X-ray is based on the fact that only bony structures are shown here, the remaining soft tissue and the Intervertebral disc can only be mapped indirectly. This means that you can assess the spinal column from its bony structure, but not - and this seems particularly important in the case of a herniated disc - the situation of the intervertebral disc and its individual problems.
Myelography

As part of a Myelography in the case of a herniated disc, an X-ray contrast medium is injected into the Nerve sac (Dural sac). The contrast medium in the nerve sac makes the spinal cord, including the nerve root, indirectly visible in the form of a contrast medium recess. However, since very good cross-sectional imaging methods can now be used, myelography is now only used very rarely.
Especially through the use of MRI (Myelo-MRI) and CT l (Myelo-CT) it is currently possible to make the most precise statements about the size and location of a herniated disc. With a computed tomography, however, a radiation exposure occurs on the organ system.
MRI / CT
The MRI of the respective affected region represents the most important and valuable diagnosis in a herniated disc. Depending on the affected region, a MRI of the cervical spine, ESPE or Lumbar spine hazards.
If inflammatory processes or if healing processes are to be assessed (so-called granulation tissue), a MRI with contrast agent hazards.
The size and position of the herniated disc can be recognized via the MRI, and the age can also be assessed in some cases.
If two MRIs are run during the course, statements can also be made about the course and duration of the symptoms.
The CT Nowadays it only plays a subordinate role in the diagnosis of a herniated disc because it is inferior to MRI in terms of detail. Sometimes you cannot see small herniated discs.
Furthermore, there is radiation exposure during a CT. An MRI, on the other hand, is radiation-free and works via magnetism.
Treatment of a herniated disc

A herniated disc can be treated both conservatively and surgically. It is decided individually which of these treatments is more suitable for the patient.
As a rule - except in the case of acute herniated discs with motor and / or sensory deficits - the therapy of a herniated disc initially consists of conservative treatment, which can be made up of a large number of different treatment measures. In the first stage, it is important to immobilize and relieve the spine. In order to achieve this in the best possible way, one depends on the height at which the spine is affected: In the case of a herniated disc of the cervical spine, a neck cuff is recommended for stabilization.
In the case of a herniated disc in the lumbar spine, the step bed helps to relieve the nerve. Here, the patient positions their lower legs on a support in the supine position so that the upper and lower legs are at a 90 ° angle to each other. However, it is not necessary to immobilize the spine in the sense of a longer bed rest.
The focus of further treatment is pain therapy. Only when the person concerned is free from pain can the following measures such as Physiotherapy shows success. Pain relievers, anti-inflammatory drugs, and muscle relaxants may be used to relieve the pain. In the case of severe pain, the use of local anesthetic medication or cortisone is also helpful. Here especially in the form of a cortisone injection. Physical therapy, i.e. heat or cold treatments, is also pain-relieving. The heat applications include e.g. Warmth patches (e.g. ThermaCare®), mud and mud packs, hot baths or infrared radiation. The circulation is stimulated by warmth and the tense muscles in the back are loosened. Cold applications such as gel pillows or cold compresses are more beneficial for nerve irritation. Ultrasound therapy also has a great effect in the treatment of herniated discs: sound waves generate heat in the tissue through vibrations and thus also loosen the back muscles. Massages and acupuncture can also contribute to a desired reduction in pain. For a long-term elimination of the pain, the back muscles must be strengthened in any case. Accompanying physiotherapeutic measures are therefore an essential part of pain therapy, as strengthening the back muscles creates a guide rail for the spine, which consequently also reduces the load on the intervertebral disc.
Surgical treatment is only rarely indicated when the symptoms of the herniated disc cannot be brought under control by conservative measures. This is often the case when nerves have been damaged in the herniated disc and as a result symptoms of paralysis (motor and sensory) occur. An example of this is a herniated disc in the lumbar spine, which disrupts bowel and bladder emptying by damaging a nerve. During an intervertebral disc operation, the herniated part of the disc material is removed in order to relieve the constricted nerve.
There are various ways of treating a herniated disc surgically. In an open operation on the spine, the surgeon can either remove the intervertebral disc or the "prolapsed" tissue that affects the nerve. Or a minimally invasive procedure ("keyhole surgery") is chosen. Similar to the open procedure, the intervertebral disc is removed, but this time the surgeon works endoscopically, i.e. it reaches the spine through a small incision. After a disc operation, another herniated disc can occur. It can also happen that scars form from the removed tissue, which again irritates the spinal cord nerve and the original symptoms remain.
Read more on the subject below:
- Treatment of a herniated disc
- Herniated Disc Surgery - What Are the Pros and Cons?
Medication for a herniated disc

Painkillers that inhibit pain and inflammation at the same time are suitable for drug therapy of a herniated disc. Non-steroidal anti-inflammatory drugs, or NSAIDs for short, are ideal for this. These include active ingredients such as diclofenac or ibuprofen. By inhibiting an enzyme, cyclooxygenase (COX), NSAIDs prevent the production of prostaglandins, which play a key role in the development of pain and inflammatory reactions.
The pain reliever paracetamol can be taken as an alternative to NSAIDs, mainly because of its better tolerability. It is also pain reliever, but not as anti-inflammatory as the NSAIDs.
Corticosteroids (cortisone) have an anti-inflammatory effect and are therefore well suited to anti-inflammatory measures. Especially when there is a threat of nerve damage, cortisone is a very effective drug against swelling caused by the herniated disc.
Read more about the topic here: Cortisone therapy for a herniated disc
Not every herniated disc needs to be treated with cortisone.
Muscle relaxants, i.e. muscle relaxing drugs, can also help with a herniated disc. They loosen up the muscles and so relieve tension.
Read more about the various muscle relaxants below: Muscle relaxants
Opioids (morphine, tramadol) are recommended for severe and long-lasting pain. Opioids are strong pain relievers, which can cause severe side effects and are therefore only used under control in medical treatment.
If the pain is chronic and the effect of other pain medication was insufficient, there is still the option of using anticonvulsants and antidepressants. These drugs raise the pain threshold so that the patient develops better pain tolerance.
Read more on the subject at: Medication for a herniated disc
PRT
If previous therapeutic measures such as medication, physiotherapy and physical measures are not sufficient for a noticeable improvement in an existing disc symptoms, then PRT can be used as an additional pain reliever.
The abbreviation PRT means the periradicular therapy, a relatively new and non-operative measurewhich can basically be carried out on all sections of the spine.
Here will be under local anesthesia medication directly to the affected or pinched nerve on the spine using a PRT needle injected. It is also possible to work with a small dose of medication, as the precise placement has a soothing effect on the painful nerve root.
One is often injected Combination of a corticosteroid (cortisone) and a long-acting local anesthetic: The corticosteroid (cortisone) does this Decongestion the irritated nerve root and the herniated disc, thus giving the nerve more space at its exit point from the spine so that it is no longer pinched.
The local anesthetic leads to a Reduction in inflammation and localized pain radiation. If the medication is used as a depot, this effect should last for a longer period of time. As a control, the PRT is performed using imaging techniques (roentgen, CT or MRI) to ensure accurate placement of the injection needle.
With the help of periradicular therapy (PRT), a significant pain relief or even that Freedom from pain can be achieved. Usually this is usually enough 2-4 treatments which should take place at weekly intervals.
Read more extensive information on: PRT
You can find a lot more information about what you can do with an existing herniated disc under our topic: Herniated disc - what to do?
Operation of a herniated disc
If conservative therapy does not lead to a reduction in pain in the case of a herniated disc or if the herniated disc has led to neurological disorders and impairments, then an operation can be performed.
The indication for an operation for a herniated disc is now more than ever carefully considered. The operation is performed under general or local anesthesia and can be offered in different variants depending on the surgeon and clinic.
The minimally invasive technique enables the operation of the herniated disc without large incisions. However, it is not possible with every type of herniated disc and the surgeon must decide whether minimally invasive work can be carried out.
There are several minimally invasive methods available. In the microsurgical variant, the patient usually lies on his stomach - in the case of herniated discs on the cervical spine, on his back - and an approx. 2 cm skin incision is made through which the surgeon can operate on the affected disc with the smallest of instruments.
With the endoscopic variant, a small tube is pushed through a skin incision of approx. 1 cm to the intervertebral disc. The tube (endoscope) can be inserted from the side or from the back. Very small instruments and a camera are introduced through the endoscope through which the surgeon can remove the herniated intervertebral disc. With both variants mentioned, a laser can also be used instead of scalpels. In this case, herniated discs are not cut away, but evaporated. In addition, even the smallest portions of intervertebral discs that otherwise cannot be reached can be removed in this way.
There is also electrotherapy. Here the intervertebral disc is operated on at temperatures of over 90 degrees Celsius.
More complicated herniated discs often have to be operated on in the conventional open surgical variant. A longer skin incision is made from the back and the surgeon cuts through the posterior ligaments of the spine to reveal the spinal canal. It may also be necessary to remove parts of the vertebral arch.
Read more on the topic: When does a herniated disc need to be operated on?
Surgery Risks
The Operation of a herniated disc is not risk free and should therefore not be performed without an appropriate indication. Basically, every general anesthetic is a risk.
However, due to the development of minimally invasive procedures, which can also be performed under local anesthesia, this is an avoidable risk. After the operation can at the surgical site Secondary bleeding, Bruising and Swelling arise and the wound can become infected.
It is also relevant that Pain, tingle, Numbness and others too neurological failures may persist or even reappear after the operation, as they emerge during the operation Nerves irritated or injured can be. The technical term for these symptoms after the operation of the herniated disc is called Post nucleotomy syndrome.
In addition to the nerves, there is a risk that vessels or other organs (intestines, urinary bladder, etc.) will be injured during the operation. since Use of the minimally invasive operation variants can a large proportion of complications can be prevented, as the smaller surgical access leads to significantly fewer injuries to other tissues.
Duration of the operation
Most used nowadays minimally invasive procedure to operate a herniated disc take about in most cases 30 - 60 minutes. However, this time depends on which variant the surgeon uses, how the herniated disc is and which access route is selected.
Furthermore, for example, too very overweight or old age the patient's factors that influence the duration of the operation.
At Interventions at them multiple intervertebral discs may be affected by surgery up to 120 minutes take time, since several access routes have to be created here and the operating time is added up accordingly.
In which conventionally open surgery is the operating time a herniated disc, depending on the location (cervical spine, thoracic spine, lumbar spine) and access route, between 60 and 120 Minutes.
Should in addition to the removal of the incident additional stiffener (Spinal fusion) of the spine or a Intervertebral disc prosthesis are introduced, then the procedure can be up to take several hours.
In addition to the pure operation time in addition, the time for anesthesia before and after the operation to be included. Appropriate anesthesia or anesthesia must be performed prior to the operation. After the operation need it Time to wake up in the recovery room or to remove the local anesthetic.
Herniated disc during pregnancy

Pregnant women are one increased riskto suffer a herniated disc. Most commonly, a herniated disc occurs during pregnancy in the field of Lumbar vertebrae on.
The reason for the emergence is mainly due to the Weight of the growing baby. In many cases it is Back muscles not sufficiently designed to withstand this counterweight. This is how the mother-to-be develops one Bad posturewhich can lead to a herniated disc.
Also favors the hormonal change of the woman during pregnancy such an event. The Band washers absorb more water and thus become more unstable and more prone to an incident.
If there is a herniated disc during pregnancy, the conservative treatment first and foremost. Before pain reliever medication is used, attempts are made to help the expectant mother with other measures. Move, Massages, physical therapy or acupuncture can help alleviate the symptoms. Even reducing stress and relaxing the pregnant woman can release tension and improve symptoms.
If that doesn't work, come pain reliever drugs for use. It is essential to use the Protection of the unborn child be respected. The doctor only prescribes pain medication that does not pass through the placenta into the child's bloodstream during pregnancy and thereby harm the child.
Paracetamol is the first choice pain medication during pregnancy. (Please refer Paracetamol in pregnancy)
Sport and the herniated disc

The best remedy, a herniated disc to prevent, is Move. This allows the Prevents wear and tear on the spine by providing the intervertebral disc with better nutrients and thereby strengthening it. However, caution is advised when choosing the sport - because not every movement is beneficial for the back.
For people with back problems, however, there is a wide choice that is safe.They are particularly suitable for back-friendly training of the abdominal and back muscles swim, Walking and To go biking. In these sports, the muscles of the abdomen and the back are equally stressed, so that a strong backbone is formed.
Even Jogging is after a herniated disc is allowed after one. It is advisable to pay attention to an oncoming surface when jogging. Best should be on one soft flooring such as. be jogged on forest floor and not on hard surfaces such as asphalt in order to protect the spine from compression. Sports that put a lot of strain on the spine (e.g. lifting weight) or involving rotating movements (e.g. tennis) will use the Spine discouraged for the sake of experts.
- Herniated disc and exercise
- Jogging after a herniated disc
Localization of the herniated disc
Lumbar disc herniation
A disc prolapse of the Lumbar spine (lumbar spine) - also called lumbar disc herniation - occurs significantly in comparison to the herniated disc of the cervical or thoracic spine more often on. About 90% of all herniated discs are found in the lower portion of the spine. The reason for this is the weight on the lumbar spine, which is particularly noticeable when moving. The lumbar spine is the most stressed during physical work or sport.
There is also a frequency distribution within the lumbar spine. 80% are distributed over the lumbar spine segments L4 / 5 and most frequently L5 / S1
- Herniated disc of the lumbar spine
- Herniated disc L4 / 5
- Herniated disc L5 / S1
If there is an incident in the lumbar spine, so that gelatinous mass from the Intervertebral disc exits, can annoy irritated or even pinched. Local pain over the affected lumbar section of the Spine can indicate a herniated disc. In addition, there is a local Inflammatory responsewhich sometimes aggravates the pain. Since in the lumbar spine the nerves that supply the legs come from the Spinal canal can emerge Pain also radiate segment-like over the leg to the foot - depending on which vertebral segment is affected by the incident. It can also be in the legs Sensory disturbances - how unpleasant Tingle, deafness- or even to Paralysis of the muscles come.
In the worst case, a herniated disc of the upper lumbar spine affects those nerves that are responsible for regulating the Bladder muscles are responsible. In this case, the patient may experience a Voiding disorder come, i.e. that he no longer has control over the evacuation of urine in the bladder and incontinent and other symptoms will show up.
With additional symptoms such as Fecal incontinence and Numbness in the genital and anal area (Breeches anesthesia) one speaks of "Cauda Equina Syndrome". A doctor should be contacted quickly here. With the help of a Emergency surgery an attempt is then made to relieve the constricted nerve root. In this way, chronic stool and urinary incontinence can be prevented in the best case.
Figure lumbar spine with herniated disc (NPP)

- Vertebral bodies
- Intervertebral disc
- Herniated disc / protruding disc
- Spinous process
Herniated disc cervical spine

A disc prolapse of the Cervical spine is also medically called cervical disc herniation designated. Since this area of the spine is not as heavy as the thoracic and lumbar spine, herniated discs are in the cervical spine less common to observe. The lower section of the cervical spine is often affected, as this is where the individual vertebral segments have the greatest mobility. In the cervical spine, a herniated disc can press on the nerves emerging from the spinal canal. This is especially noticeable Pain in the neck areathat extend up to the Shoulders or that head can spread. Since the nerves that supply the arms are located in the cervical spine, a cervical disc herniation is often also manifest pain radiating to the arm. It can also affect the person concerned Sensory disturbances show in the skin area supplied by the affected nerve: uncomfortable tingling sensation or deafness up to the hands occur. In the worst case it comes in addition to motor failures of the arm, so to paralysis of the arm muscles. Many sufferers also suffer from other symptoms, such as dizziness or Balance disorders.
Because of the symptoms, many patients experience a Relieving posture taken, which also contributes to the stiffening of the neck and thus further aggravates the symptoms.
The causes of a herniated disc of the cervical spine are too large and false loads, such as unfavorable movements of the cervical spine. This also includes long-term incorrect loads, such as working in front of the computer with the head stiff. Cervical disc herniations can also be provoked by injuries. This can for example be with a Rear-end collision, in which the head is thrown forward unprotected and not stabilized. Slipped discs in the neck area are more likely to occur older people because of the wear and tear of the Cervical spinethat show up in the form of loosened joints can more easily lead to an incident.
MRI of a herniated disc of the cervical spine

MRI cervical spine:
- Intervertebral disc
- Vertebral bodies
- Spinal cord
- disc prolapse
Further information on this topic can also be found at: MRI of the cervical spine
Herniated disc of the thoracic spine

A herniated disc on the Thoracic spine is a lot less common as a herniated disc of the cervical or lumbar spine. Often these herniated discs present themselves symptomless and are sometimes only called by the doctor Incidental finding in a CT or one MRI of the thoracic spine discovered. But not every patient is spared. The main symptom of a herniated disc is the thoracic spine Pain. And if the person concerned complains of pain, then it usually is very strong pronounced. The pain is there local over the affected vertebral segment, in many cases go with a local one inflammation or Muscle tension in the thoracic spine area.
Also the pain from the spine can be along the way Ribs forward to the middle of the Rib cage radiate. This special radiation of pain is called "Intercostal neuralgia“And is described by patients as very uncomfortable. Typical of the pain caused by a herniated disc of the thoracic spine is that it is caused by to cough, Sneeze or Laugh be reinforced.
Those affected also complain of other complaints from time to time, such as Racing heart or Palpitations and tightness in the chest. Even dizziness and Shortness of breath reported by some affected patients.
If there is a herniated disc in the thoracic spine, pain often also radiates into the spine poor off, but the legs are less often affected. On arms and Legs the herniated disc can in turn result sensitive disorders (Tingling, numbness) and motor failures (Paralysis) express. It can also cause an impairment of the thoracic spine Bladder and bowel disorders come. If you experience these symptoms, you should see a doctor immediately, as there is damage to the spinal cord and surgical treatment is necessary.
The main cause of a slipped disc of the thoracic spine is the Wear and tear due to old age to call. Also physical exertion and burden, such as Bad posture or improper loading can provoke such a herniated disc.
Epidemiology
Back pain alone are not an indication of the presence of a herniated disc. Generally it is very difficult to find that Causes of back pain to detect. Even X-ray images cannot always provide the desired clarity.
To show that back pain and the actual presence of one pathological (= pathological) disc findings are not always mandatory, Jensen's study should be cited here as an example. This randomized controlled study cooperated MRI scans of the lumbar spine and examined it symptom-free people. The results astonish:
At 52 % the patient could see a protrusion of the intervertebral disc (= Protrusioalso known as intervertebral disc protrusion or disc protrusion).
At 27 % A herniated disc was diagnosed and, in addition, 1% of the patients had a herniated disc that was already pressing on the surrounding tissue.
At 38 % of all patients, the changes were not limited to just one disc.
It is alarming that only about 33% of all those examined stated that they suffered from back pain. This makes it clear that diagnostic accuracy can only be achieved if the diagnostic measures are taken as completely as possible. Different symptoms must always be differentiated from each other in order to make a reliable diagnosis "disc prolapse"to be able to provide.
Age and frequency
The herniated discs occur most often in the area of the Lumbar spine followed by slipped discs in the area of the Cervical spine, Incidents in the field of Thoracic spine are relatively rare as a further possibility.
During lumbar spine incidents, most common between the 30th and 50th The cervical spine is between the years of life 40th and 60th Year of life affected later. A disc protrusion (disc protrusion see below) can occur much earlier.
In the further course of life, herniated discs are then found less frequently, as the disc water loss then occurs more intensely. With regard to the herniated disc, this has the "advantage" that the gelatinous core becomes thicker and can therefore only occur more difficultly.
Differentiation of a herniated disc
In the context of a herniated disc one differentiates between:
- one Disc protrusion (Picture below), which leads to a bulging of the Annulus fibrosus comes
- one Disc prolapse (= Herniated disc; Picture below) into the intervertebral holes or - which is much less common - into the spinal canal.
- one Sequestration, as a result, the prolapsed parts no longer have any connection with the original disc.
Think of it like this:
- At a Disc protrusion the intervertebral disc as such initially remains intact. The inner gelatinous nucleus bulges forward and presses on the cartilaginous outer ring made of connective tissue.
- At one Nucleus pulposus prolapse (NPP) on the other hand, the gelatinous core partially exits through the outer ring. The part that emerges remains connected to the rest of the inner gelatinous nucleus and does not encapsulate itself.
- An encapsulation of the trodden area, however, takes place in one Sequestration Instead of: The prolapsed part of the gelatinous nucleus is no longer connected to the inner area.
Prolonged areas of the intervertebral disc can be more or less pronounced Nerve roots that are directly adjacent to the intervertebral disc. This also includes the in the lower lumbar region Sciatic nerve, which under certain circumstances can trigger very violent, severe pain when pressure is exerted (sciatic pain = Sciatica).

Healthy intervertebral disc
- Nucleus pulposus (Gelatinous core)
- Annulus fibrosus (Fiber ring)

Intervertebral disc bulge (protrusion)
- Nucleus pulposus (gelatinous nucleus)
- Anulus fibrosus (fibrous ring)
- Bulging

Figure slipped disc (prolapse)
- Nucleus pulposus (gelatinous nucleus)
- Anulus fibrosus (fibrous ring)
- incident
Disc herniation anatomy
Disc anatomy
Before discussing the herniated disc, the concept of Intervertebral disc be sufficiently clarified. Only when the functions and properties of the intervertebral discs have been clarified can the extent of the herniated disc and its therapeutic measures be understood.
Position - Where are the "intervertebral discs"?
Between two vertebral bodies of the Spine there is a cartilaginous connection called an intervertebral disc. Since it lies between two vertebral bodies, it is often referred to as Intervertebral disc. The vertebral body and intervertebral disc are firmly fused together.
Properties of an intervertebral disc
An intervertebral disc consists of the so-called annulus fibrosus, the connective tissue, cartilaginous outer ring and the nucleus pulposus, the inner gelatinous nucleus. In total, humans have 23 intervertebral discs, so that in their totality they represent approximately ¼ of the total length of the spine.

Function of the intervertebral disc
The mobility of the spine:
Shown are 2 vertebral bodies and the nucleus pulposus, on which the vertebral bodies can move freely against each other like on an elastic ball.
The one described above Nucleus pulposus, the gelatinous core of the intervertebral disc is under pressure. The consistency of this core is always dependent on the water balance of the intervertebral disc. The following rule of thumb applies:
The more water it soaks up in a similar way to a sponge, the plumper, more elastic and stronger it is.
The "soaking process" should be shown in an understandable way. The presence of the Water balance and its decrease can be illustrated in the context of a person's aging process: In the course of life, the water content of the intervertebral disc automatically reduces. This becomes visible to the outside, for example, as part of the aging process, in the course of which people become smaller.
Furthermore, you can see in yourself every day that the same person is about 1 to 3 cm (approx. 1%) is larger than in the evening, which is related to the fact that the intervertebral discs recover from the nightly relief and were able to suck fully again. You can imagine a wrung-out sponge that is placed in water and soaked up as much as possible. Just like a sponge, it wins Intervertebral disc thereby in height.
However, an intervertebral disc not only needs water, but also so-called vital substances. Since intervertebral discs do not feed on the blood supply, these vital substances can only be absorbed if they are present and through varied human movements (bending backwards, circling the hip, Go, to jog, Stooping, ...) were expelled beforehand.
The following principle applies:
The more varied a person's movement, the more intensely the vital substance supply and water supply of this highly sensitive cartilage tissue work.

burden
Through the Band washers Only then does the mobility of the spine arise. Without it, the spine would be stiff, comparable to a broomstick, for example. The intervertebral discs thus enable the elasticity and flexibility of the vertebral segments.
A shift in weight forwards, backwards or to the side causes a shift of the core in the corresponding direction. Through this relocation of the nuclei, the cartilaginous ring, called the cartilaginous fiber disc one-sided and depending on the movement differently compressed, so that the load that one Intervertebral disc has to endure, can be quite different.
The diagram below is intended to show the different loads that are placed on the intervertebral discs during everyday movements. It is noticeable that when lying down (Supine position) the pressure on the intervertebral disc is lowest. Incorrect postures or incorrect movements (middle right, bottom) increase the load on the intervertebral disc. If there is already cartilage wear, a disc prolapse occur. Cartilage wear, in turn, is strongly promoted by advanced age and / or water loss.
- Vertebral bodies
- Protrusion (bulging of the intervertebral disc)
- Spinal cord
- disc prolapse