Degenerative spinal disease
Synonyms in a broader sense
- Spinal disease caused by wear and tear
- Spinal wear
- Spinal degeneration,
- Degeneration of the spine
- Wear and tear on the spine
- Lumbar spine syndrome
- Cervical spine syndrome,

definition
Among the degenerative (wear-related) Spinal column diseases (back problems) belong to several clinical pictures, which can occur in isolation or together and whose common characteristic is the age-dependent occurrence. The lumbar spine is most commonly affected.
The main degenerative diseases of the spine (back pain) include:
- Spinal canal stenosis (narrowing of the spinal canal)
- Spondylarthrosis (osteoarthritis of the small vertebral joints = facet syndrome)
- Spondylosis / osteochondrosis (wear and tear on the intervertebral discs and vertebral bodies)
- Degenerative spondylolisthesis (pseudospondylolisthesis = sliding of the vertebral body)
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
anatomy
The spine consists of the vertebrae, the intervertebral discs (= intervertebral vertebrae) and the associated ligaments, the task of which is to connect and stabilize the structures of the spine. The human spine is made up of 33 - 34 vertebral bodies, which are differentiated based on their different areas of responsibility.
A distinction is made between seven cervical vertebrae of the so-called cervical spine, twelve thoracic vertebrae of the so-called thoracic spine, five lumbar vertebrae of the lumbar spine, five sacrum and tail vertebrae.
The last two vertebrae mentioned merge into the sacrum and coccyx between the ages of 20 and 25.
The spine forms the so-called vertebral canal in which the spinal cord is located.

- First cervical vertebra (carrier) -
Atlas - Second cervical vertebra (turner) -
Axis - Seventh cervical vertebra -
Vertebra prominent - First thoracic vertebra -
Vertebra thoracica I - Twelfth thoracic vertebra -
Vertebra thoracica XII - First lumbar vertebra -
Vertebra lumbalis I - Fifth lumbar vertebra -
Vertebra lumbalis V - Lumbar cruciate ligament kink -
Promontory - Sacrum - Sacrum
- Tailbone - Os coccygis
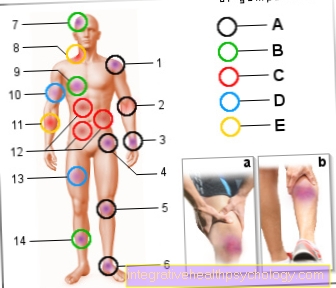
I - cervical spine (red)
II - thoracic spine (green)
III - lumbar spine (blue)
You can find an overview of all Dr-Gumpert images at: medical illustrations
pathology
The wear and tear of the intervertebral disc begins in a person's 20s. Disc protrusion or herniated disc (med. Nucleus pulposus prolaps or NPP) can occur. The increasing loss of water from the intervertebral discs leads to a decrease in height of the intervertebral body section (osteochondrosis). The consequences are an overload of the small vertebral joints, a malfunction of the spinal ligaments and a creeping instability of the spinal column movement segment, each consisting of two vertebral bodies and the intervertebral disc in between.
The base and cover plates of the vertebral bodies are more stressed by the lowered intervertebral disc. The body reacts to this with bone compression in the area of these structures (sclerotherapy), which can be seen radiologically.
The body tries to counter the creeping instability of the spine by producing bony additions to the vertebral bodies (osteophytes / exophytes) that look for support in the environment.
If the instability is very advanced, the spine can become warped due to wear and tear, which further weakens the statics of the spine (degenerative scoliosis).
The changed spine statics also changes the origin and attachment points of the muscles and the ligamentous apparatus of the spine, whereby some muscles and ligaments come too close and shorten and others are stretched too much. Both of these lead to the weakening of these structures through the loss of function. Painful muscle hardening (muscle tension / myogelosis) can develop.
Read more on the topic: pain in the back
An incongruent position of the vertebral body joints to one another leads to premature cartilage wear of the joint partners. The same processes then take place that are well known for knee or hip arthrosis. There is inflammation of the joints, swelling and thickening of the capsules, and joint deformity even more quickly than in the large joints. The overall picture of a vertebral joint arthrosis (spondylarthrosis = facet syndrome) has emerged.
Instability-related displacements of the vertebral bodies (spondylolisthesis / pseudospondylolisthesis), thickening of the vertebral joint structures, bony vertebral canal attachments, intervertebral disc protrusions and thickening of the vertebral ligaments (ligamentum flavum) can ultimately lead to a considerable narrowing of the spinal canal itself (spinal canal stenosis) and the spinal canal itself.
Spondylosis
Strictly speaking, the term spondylosis is a collective term that summarizes a number of bony changes in the spine. These are irregularities such as bony attachments, bulges, or spikes, which can be seen particularly well in an X-ray image or in a computer tomography of the spine.
A wide variety of diseases can lead to the diagnosis of spondylosis. For example, osteoarthritis of the spine, degenerative changes in the intervertebral discs or chronic inflammatory systemic diseases such as ankylosing spondylitis are common (Ankylosing spondylitis).
Read more on the topic: Lumbar spine syndrome, facet syndrome
Spondylosis is often associated with discomfort, especially back pain. It is not uncommon for pain to radiate into the arms or legs. In particular, the cervical spine and the lumbar spine are affected by the changes. The focus of therapy for spondylosis is pain therapy based on drugs such as ibuprofen or diclofenac. Intensive physiotherapy can often help to alleviate the symptoms in the long term.
Read more on the topic:
- Herniated Disc: Symptoms in the Leg
- Back school
- Cervical Spine Syndrome - How We Can Help You!
Facet arthrosis
One speaks of facet arthrosis when certain joints in the spine are affected by a degenerative disease. Both Facet joints, also called intervertebral joints, it is the connection of the articular processes between two neighboring vertebrae. Among other things, the facet joints ensure free and smooth mobility of the spine.
Read more on the topic: Facet syndrome
If these joints degenerate in the course of life, back pain is the focus of the complaints. Osteoarthritis can be recognized and diagnosed with the help of an X-ray or computed tomography. It is a common disease that mainly affects the elderly. Risk factors can be bad posture, long-term excessive strain and obesity.
Facet osteoarthritis therapy is based primarily on taking pain-relieving medication and intensive physiotherapy. Physiotherapy can build up the muscles of the back and thus relieve the spine.
Read more on the topic:
- Build back muscles
- Exercise the lower back muscles
- Spine training
Spinal diseases in childhood
Scoliosis
Scoliosis is a disease of the spine that develops over the course of growth. There is both a lateral bending of the spine and a rotation of the individual vertebral bodies. Scoliosis can be recognized by looking at the person's spine from behind and running your finger along the back tips of the spine. If these tips deviate significantly to one side, scoliosis may be present.
The exact causes that are responsible for the occurrence of scoliosis have not been conclusively clarified. It is believed that the different growth of the anterior and posterior parts of a vertebral body is the cause of the occurrence. Children from the age of 11 are often affected, although there are also forms in which children between the ages of 0 and 10 are affected. Girls are affected more than average.
As a rule, there are no symptoms at the beginning of the disease, but in the course there may be breathing difficulties and pain due to the bending of the trunk. With the help of a corset treatment, the progression of the disease can be stopped, but it is not possible to improve the existing malposition. Different operations on the spine are also possible.
Read more about the topics:
- Pain associated with scoliosis
- Brace treatment for scoliosis
- Surgery for scoliosis- what options are there?
Scheuermann's disease
In Scheuermann's disease (Adolescent kyphosis) is a disease of the spine that mainly affects adolescents aged 10-13 years. Boys are more often affected by the disease. In Scheuermann's disease there is excessive flexion of the thoracic spine. While the healthy spine arches only slightly backwards in the area of the upper thoracic vertebrae, this becomes very apparent in a person with Scheuermann's disease.
Read more on the topic: Hunchback
The exact cause that is responsible for the occurrence of Scheuermann's disease is not yet known. In addition to genetic factors, rapid growth and the performance of certain competitive sports are also discussed as causes. Affected people usually do not complain of pain, although painful secondary diseases can occur in adulthood.
Read more on the topic: Long-term consequences of Scheuermann's disease
Scheuermann's disease is diagnosed in addition to a physical examination using an X-ray examination of the spine.
The therapy consists of physiotherapy, which aims to strengthen the muscles in the back. Particularly pronounced clinical pictures can be treated with a corset.
Read more on the topic: Back training - tips for a strong, healthy back
Diagnosis of spinal diseases
In addition to collecting the medical history (anamnese) and a careful physical examination, imaging procedures are of particular importance in the diagnosis of spinal disease.
Due to the different diagnostic methods, one can and wants to obtain extensive information with regard to therapeutic measures to be taken.
roentgen
In principle, the X-ray of the Spine refer to as basic imaging diagnostics. The attending physician receives an insight into the posture of the spine via the X-ray images. In addition, bony changes (calcium salt reduction, spinal curvature, a Vertebral fracture, Vertebral joint arthroses, vertebral body attachments) and disc degradation can be detected.
CT and MRI of the spine
A cross-sectional image diagnosis (CT and MRI, either with or without Contrast media) also enables the pain to be assigned to a specific nerve or a specific section of the spine.
With the help of a CT (computed tomography) examination, in particular further questions regarding the bony structure can be answered (e.g. spinal canal stenosis, vertebral body fracture).
MRI (magnetic resonance imaging), on the other hand, is even more valuable in spinal column diagnostics, as it shows not only the bony structures, but also the soft tissue structures (intervertebral discs, nerve roots, ligaments) much better than CT. All of the above Diseases can be detected with the MRI and assigned to a specific section of the spine.
At Vertebral body fractures as Spinal disease is it with the help of the MRI of the respective region (e.g. MRI of the lumbar spine) possible to differentiate between fresh and old fractures, which can have immediate therapeutic consequences (see Kyphoplasty).
Read a lot more information at: Diagnosis of a spinal disease
Myelography
The Myelography describes an examination in which the patient is injected with contrast medium into the dural sac. The dural sac envelops that Spinal cord and is in the area of the lower Lumbar spine the area that surrounds the beginning of a nerve before it leaves the spinal canal. By mixing Nerve water and contrast media, specific issues relating to the spinal cord can be clarified. After the contrast agent has been injected, functional recordings of the spine are usually made (in flexion and extension) in order to identify nerve congestion in the functional position. At the same time, a CT examination is often added in the case of spinal diseases, which is more informative for certain questions due to the contrast agent applied.
Further information is available under our topic: Myelography
In order to rule out nerve damage or to be able to determine the degree of possible nerve damage, extended examinations must be carried out in the case of a spinal disease. This can be done through a specialist neurological examination and recording of neurophysiological parameters (e.g. nerve conduction velocity).
MRI of the cervical spine

2. Cervical vertebrae
3. Cervical vertebrae
4. Cervical vertebrae
5. Cervical vertebrae
6. Cervical vertebrae
7. Cervical vertebrae
8. Herniated disc of the cervical spine
9. Spinal cord
You can find a lot more information about this MRI image on our website: MRI of the cervical spine
Symptoms
Characteristic of degenerative spinal diseases are persistent, difficult to influence back pain and a functional restriction of the spine.
The symptoms can be limited to the spine or spread to the legs (lumbar spine) or arms (cervical spine).
They can only occur during exercise or exertion, or at rest.
It is often difficult to name a specific disease because the above Diseases often occur together and it cannot be precisely clarified which complaints can be attributed to which morphological change. That is why one often speaks of a degenerative one Cervical spine syndrome or degenerative lumbar spine syndrome, which is supposed to describe the symptom complex of degenerative spinal diseases.
The characteristics of the above Individual illnesses are listed separately. Follow the appropriate links.
Read a lot more information on this topic at: Symptoms of spinal disease
therapy
The treatment of degenerative spinal diseases is largely conservative. Mostly elderly people are affected, some of whom have severe internal pre-existing illnesses, to whom extensive surgical measures are no longer required and usually do not have to. In the case of severe nerve damage, uncontrollable, debilitating pain and circumscribed disease findings, surgical therapy measures can help.
Since there is no causal therapy for an advanced degenerative spinal disease, pain therapy and physiotherapy are the focus of treatment.
These include:
- Medicinal Pain therapy (NSAIDs, Opiates etc.)
- Pain patches
- Physical pain therapy (electricity therapy, ultrasound, heat, etc.)
- Infiltration therapy (nerve blocks, Periradicular therapy, trigger point infiltration)
- Mobilizing, stabilizing physiotherapy
- Back school
- Naturopathy: Osteoarthritis and Homeopathy (please refer: Homeopathics for cervical spine syndrome)
To the operative therapy options belong:
- Spinal canal decompression (removal of ossifications and disruptive soft tissue)
- Intervertebral disc surgery (Microdiscectomy, IDET)
- Stiffening operations (Spinal fusion)
- Intervertebral disc prosthesis
- Sclerotherapy e.g. of small vertebral joints (sclerotherapy / proliferation / denervation therapy)
- Racz catheter
The operative therapy options are dealt with under the individual clinical pictures. Follow the links.