Chest pressure - what to do?
definition
Feeling pressure in the chest can have many causes, including both harmless and serious conditions.
These are differentiated according to their location in the chest cavity and can consequently be caused by the various organs in the chest such as the lungs, the heart or the esophagus.
In addition, a feeling of pressure in the chest cavity occurs during a panic attack.

Causes of a pressure in the chest
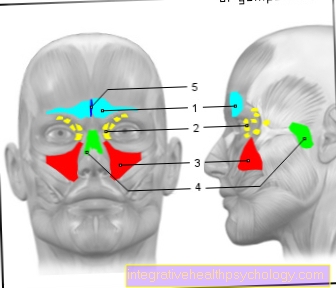
There are several organs in the chest and numerous blood vessels run through this area. A feeling of pressure in the chest can have various causes. A heart attack is traditionally accompanied by pain and a feeling of pressure in the chest area. As a result, many people worry quickly when they experience chest pressure. If thoracic pressure occurs due to constricted coronary arteries, it is called angina pectoris. However, if the heart is affected and there is pressure in the chest, it is not always a heart attack. Many people who suffer from calcified coronary arteries (coronary artery disease) regularly feel a feeling of pressure in the chest when they exercise. This is an indication that the coronary arteries are narrowed. Often times, nitro spray can help. It expands the blood vessels and thus ensures better blood flow to the heart. However, it is extremely difficult for patients to tell whether it is a seizure or a heart attack. In addition to a disturbance in the area of the heart vessels, cardiac arrhythmias can also lead to a feeling of thoracic pressure. These include, for example, the mostly harmless heart stumbling in supraventricular extrasystoles or atrial fibrillation.
Read more on the topic: Symptoms of a heart attack
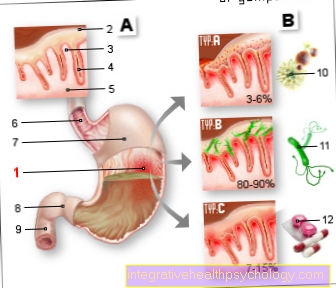
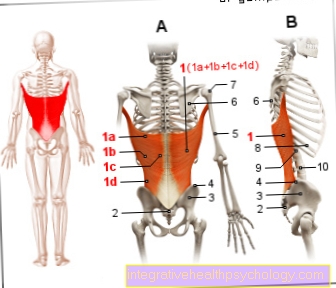
The esophagus is also an organ that can often trigger a feeling of pressure in the chest. Many people suffer from what is known as reflux oesophagitis, or heartburn. The backflow of stomach acid from the stomach into the esophagus can cause uncomfortable pressure in the chest area. The two lungs are also located in the thorax. Diseases of the lungs can lead to a feeling of pressure or pain in the chest area. Possible diseases are pneumonia, pulmonary embolism, i.e. an occlusion of a large pulmonary vessel, or a pneumothorax. The aorta, i.e. the main artery, also runs through the back of the chest. If the aorta is damaged, this usually leads to severe pain, and a feeling of pressure is rather unusual. Another possible cause of chest pulling or squeezing can be a pinched rib nerve. It is true that stabbing, suddenly shooting pains are more likely to occur here, but more rarely a feeling of pressure can occur. Sore muscles after unusual physical exertion can also lead to a feeling of thoracic pressure. Herpes zoster (shingles) is also one of the nerve diseases in a broader sense. The pathogens stay in the body for decades and then attack at some point if the immune system does not offer enough protection. Shingles can cause severe pain in the affected area, and a feeling of pressure can also occur. Degenerative changes or diseases in the spinal column can also cause a feeling of pressure in the chest area. Physical causes are not always responsible for a feeling of pressure on the chest. One of the most common causes is anxiety during a panic attack.
Causes by location
left in the chest
If there is pressure on the left side of the chest, the heart on the left side of the chest should be considered as the trigger. In addition to myocardial infarction, subtotal occlusions of the coronary arteries or cardiac arrhythmias such as extrasystoles or atrial fibrillation can lead to a feeling of pressure in the left thoracic region. If left thoracic pressure appears for the first time, which is not due to previous sporting activity with subsequent muscle soreness, a doctor should be consulted - depending on the overall situation of the person concerned - to clarify the symptoms further.
Read more on the subject at: Extrasystole
in the middle of the chest
A feeling of pressure that is located in the center of the chest is relatively typical for heartburn in the context of reflux esophagitis. But nerve disorders, sore muscles and damage to the spine can also be the cause. The central artery (aorta) seldom leads to a feeling of pressure in the chest. In a panic attack, the pressure in the chest is usually also located in the middle.
right in the chest
Pneumonia or pneumothorax can cause unilateral chest pain on the affected side (both left and right). Lung cancer (bronchial carcinoma) only causes symptoms at a very advanced stage; thoracic pressure is a rather atypical symptom. Of course, nerve affections and problems in the spine can also lead to unilateral chest pressure.
diagnosis
When a patient comes to the doctor with the symptom of chest pressure, various diagnostic steps are taken. First of all, the anamnesis is crucial. The doctor asks about the age of the patient, previous illnesses, illnesses in the family, type of complaints, time of occurrence and duration of complaints and regular use of medication. You will also be asked about other accompanying symptoms. Next up is the physical exam. Particular attention is paid to palpating the chest, listening to the lungs and examining the spine and ribs. If a lung disease is suspected, an X-ray may be necessary. Depending on what the conversation turns out to be, an EKG can be written to rule out a heart attack or cardiac arrhythmia. A safe exclusion of myocardial infarction is only possible with an EKG and two-stage blood sampling. Cardiac arrhythmias do not have to show up in an EKG that only records a few seconds of the heart's action. If a cardiac arrhythmia is suspected, it would be advisable to carry out a long-term ECG examination. The attending physician can also decide whether a blood sample is useful. Here, among other things, the heart enzymes and inflammation values can be checked. If heartburn is suspected, a gastroscopy can be performed in case of doubt. However, this is not absolutely necessary for the diagnosis. If a panic attack is suspected, only a sensitive conversation can reveal more details.
These are the accompanying symptoms
Which accompanying symptoms occur in addition to the pressure in the chest depends largely on the underlying disease. If it is a heart attack, there is also pain in the chest, usually radiating to the left arm, upper abdomen or neck. In addition, shortness of breath is common. Cold sweats and nausea can also occur. Cardiac arrhythmias such as atrial fibrillation can also lead to shortness of breath, a feeling of oppression, reduced performance and dizziness. If it is reflux esophagitis, in addition to chest pressure, there is a burning sensation in the chest, heartburn, and increased cough. With pneumonia, the cough can be painful, there is often a fever and the general condition is reduced. A pneumothorax can cause shortness of breath, as can a pulmonary embolism. If a pinched nerve is responsible for the discomfort, the discomfort is often movement-dependent, resulting in suddenly shooting unpleasant pain. If there is a panic attack with pressure on the chest, this is often accompanied by a racing heart, profuse sweating and feelings of fear.
with cough
If the symptoms of chest pressure and coughing occur at the same time, this can be an indication of the presence of reflux disease. The stomach acid runs back through the insufficiently sealed sphincter of the esophagus and leads to a significant irritation of the mucous membrane. Other symptoms include heartburn, increased belching, and the need to sleep with your upper body elevated.
with nausea
If pressure on the chest and nausea occur at the same time, this could be an indication of a heart attack. In addition, chest pain occurs, usually with radiation and shortness of breath. However, the combination of thoracic pressure and nausea is not a compelling indicator of a heart attack.
with burning
Pressure and a burning sensation in the central pressure area are relatively typical signs of reflux disease. The burning sensation is caused by irritation of the esophageal lining from the gastric acid flowing back.
with shortness of breath
The combination of thoracic pressure and shortness of breath should make one sit up and take notice. Either it is a heart disease or a disease of the lungs. Heart attacks are very often accompanied by chest pressure, chest pain and shortness of breath. But cardiac arrhythmias such as atrial fibrillation can also lead to pressure in the chest and shortness of breath. However, the same symptoms can also occur in the context of pneumonia, pulmonary embolism or pneumothorax, for example.
with back pain
Degenerative changes or diseases in the spinal column such as Bechterew's disease can lead to back pain on the one hand and pressure in the chest on the other. In rare cases, an acute rupture of the main artery (aortic dissection) can also cause pain in the back (between the shoulder blades) and thoracic pressure.
with racing heart
Palpitations and pressure on the chest can occur together, for example in cardiac arrhythmias. Examples include atrial fibrillation (absolute tachyarrhythmia) or tachycardiac arrhythmias such as Wolf-Parkinson-White syndrome (WPW syndrome). One of the most common causes for the combined occurrence of thoracic pressure with a feeling of oppression and a racing heart is the panic attack. In addition, there are strong feelings of fear, restlessness and profuse sweating.
difficulties swallowing
Difficulty swallowing and pressure on the chest can occur as part of reflux disease.
having panic attack
The panic attack is probably one of the most common causes of thoracic pressure. The panic attack starts suddenly and is hardly controllable. Those affected suddenly feel severe fear and suffer from a racing heart, a feeling of pressure on the chest, feelings of oppression and sweating.
How do you treat pressure in the chest?
The type of treatment depends largely on the underlying disease. Immediate inpatient treatment is necessary in the event of a heart attack. Immediate drug therapy with blood thinners such as aspirin, heparin, and clopidogrel / prasugrel is initiated. Depending on the type of infarction (STEMI = ST elevation myocardial infarction, NSTEMI = non-ST elevation myocardial infarction), an immediate or prompt cardiac catheter examination is necessary. Arrhythmias are treated differently. For example, if there is atrial fibrillation, permanent blood thinning is usually necessary. Rhythm stabilizing therapy is also often used. If pneumonia is present, it must be treated with antibiotics. Depending on the general condition of the patient, this treatment can be inpatient or outpatient. A pulmonary embolism usually also has to be treated as an inpatient; blood thinners are used here. In some cases, a pneumothorax has to be treated surgically, but in some cases waiting and waiting is sufficient. Reflux esophagitis is best treated by changing your lifestyle and eating habits and using drugs that reduce the acidity of the stomach, such as pantozol. If nerves are pinched, waiting, applying heat and physiotherapy usually helps. Physiotherapy and the application of heat also help with degenerative changes in the spine as the cause of the symptoms. Patients with recurrent panic attacks often require psychotherapeutic treatment.
The duration / prognosis of chest pressures
The duration or prognosis also depends primarily on the underlying disease. In the case of a heart attack, there is a significantly increased risk of life-threatening complications, especially in the first few hours and days.Once the patients have survived this phase, the prognosis depends, among other things, on the lifestyle change. Long-term medication intake is also helpful. Cardiac arrhythmias such as atrial fibrillation are chronic in many cases. Optimal therapy reduces the complication rate. Pneumonia usually heals - depending on the general condition and additional illnesses of the patient - with adequate antibiotic therapy without consequences. The symptoms usually last for several weeks until they completely disappear. Pulmonary embolism can be potentially fatal if not properly treated. The symptoms of reflux disease are often relieved very quickly by taking acid-inhibiting medication. Diseases of the spine are almost always of a chronic nature, so they last a lifetime. Pinched nerves are very painful, but the symptoms usually disappear completely after a few days. Panic attacks are usually a chronic mental illness. They occur again and again and are very stressful for the patient because they occur unpredictably. Psychotherapy can significantly reduce the disease.
Further information
You can find more information about chest complaints at:
- Emphysema
- Barrel chest
- Chest contusion
- bronchitis
- Inflammation of the bronchi