Hip dysplasia in the child
definition
Synonyms: Hip dysplasia, hip dysplasia
Hip dysplasia describes an incorrect or incomplete development of the Hip joint. Here is the Socket, the so-called Acetabulum not deep and wide enough to accommodate and cover the femoral head sufficiently.

Epidemiology
The hip dysplasia is that most common congenital deformity (malformation), it comes at about 3-4% of newborns and affects mostly girl (in the ratio girls: boys = 6:1). It occurs more frequently with a positive family history, i.e. when other family members have already had such an illness, and it is more common Births from Breech position observed and in combination with other anomalies (undesirable developments) such as the Clubfoot. It also occurs more frequently in the context of neurological diseases such as the Spina bifida or the Cerebral palsy on.
Symptoms
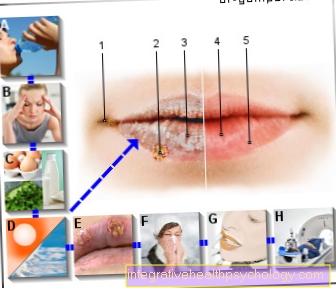
In the case of newborns, a diagnosis cannot be made clinically (i.e. only on the basis of a physical examination); the only indication of the presence of hip dysplasia is the so-called Ortolani sign, a click can be heard here when the examiner spreads the thigh on and off. After a few weeks, additional symptoms appear, such as one Anti-splay inhibitionThis means that when the child is lying on their back, the legs, which are bent by 90 ° in the hips and knees, cannot be spread sideways to the surface by the examiner.
Sometimes there is also one Fold asymmetry (So wrinkles can be seen on one side, not on the other side or in a different place) in the area of the buttocks and thighs. Also can Barlow sign Be positive, the femoral head jumping out and in from the socket can be felt when the legs are spread apart and apart and the hips are pressed forwards and backwards with the thumb and index finger at the same time.
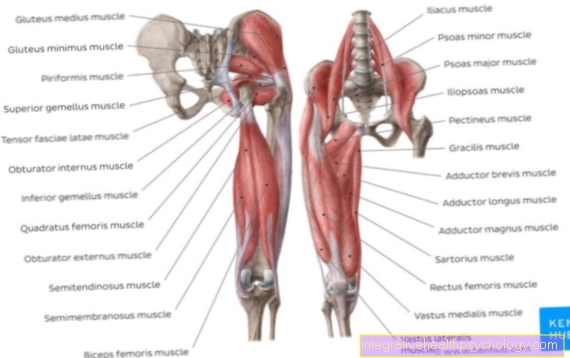
Does the dysplasia cause a Hip dislocationwhich is not infrequently the case, a Leg shortening stand out on the affected side. Also a sedentary lifestyle and - if the child is already of walking age - a limping gait can be indicative of hip dysplasia. Here is the so-called Trendelenburg sign to mention. This causes the pelvis to tilt when standing on one leg and thus also when running.
In the case of bilateral hip dislocation, the "Waddling gait“Noticeable. Often with hip dysplasia there is also a misalignment of the legs in the sense of a Internal rotation (Antetorsion) and Knock knees (Coxa valga).
Appointment with a hip expert?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The hip joint is one of the joints that are exposed to the greatest stress.
The treatment of the hip (e.g. hip arthrosis, hip impingement, etc.) therefore requires a lot of experience.
I treat all hip diseases with a focus on conservative methods.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
diagnosis
The infant can be diagnosed using a Ultrasound examination (Sonography) the hip. On the one hand this method is very reliable, on the other hand it is in contrast to the roentgen or CT (Computed tomography) completely free of radiation exposure, which should be avoided especially in children. The sonography is prescribed as a screening (early detection examination) for the Preventive medical check-up U2 or U3. In this way, the affected children are discovered very early on, which is essential for effective therapy and minimizing subsequent damage.
Different stages of the disease (after Graf) differentiated.
- Grade I. describes a normally shaped acetabulum
- Grade II describes a pathological dysplasia
- from Grade III there is also a dislocation of the femoral head (the femoral head is no longer properly seated in the socket)
- Grade IV describes a dysplastic hip with complete dislocation.
therapy
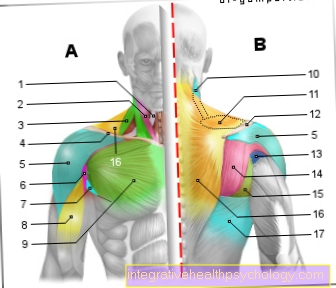
Hip dysplasia must always be treated. Which procedure is indicated depends on the stage of the disease. A Graf II hip is created using a so-called Tübingen flexion orthosis or one Splaying plaster treated. The principle here is that the femoral head is centered (i.e. pressed into the socket) by a certain fixed position of the affected leg (flexion and splaying), which leads to a stimulation of the socket growth in small children. So the goal is for the acetabulum to grow so that it better accommodates the femoral head.
From stage III, such a treatment is no longer sufficient, here the femoral head must be repositioned (centered again in the pan). Such a reduction can usually "closed“(Ie without open surgery), but can drag on for several weeks. The child then has to wear a cast (usually the so-called Fat white plaster) and regularly for sonographic controls. Here, too, comes a rail such as the Tübingen hip flexion splint is used, which must be worn until healing.
Does it give under the measures described above 2-5 years no improvement, must be operated surgically. There are several methods to choose from, all of them so-called Osteotomies (i.e. cutting through bone parts of the hip or the femoral head with subsequent rotation and reattachment), such as the Salter osteotomy or the Acetabuloplasty.
forecast
An occasional complication of therapy is the development of one Femoral head necrosisthat have gradients similar to the Perthes disease can take.
If the therapy does not fully restore the normal hip anatomy, there is a risk that a Dysplasia coxarthrosis (Osteoarthritis of the hip joint), some symptoms of this kind begin as early as around 30 years of age.