Radiotherapy for breast cancer
introduction
There are various therapy options for patients with breast cancer. In principle, chemotherapy, radiation, hormone therapy and / or an operation are available. Which therapy the gynecologist will choose depends on various factors, including the age of the woman and whether or not she had her last menstrual period, the tumor size, certain tissue properties of the tumor, the extent of metastasis (spread) of the tumor and the hormone receptor status . Radiation therapy enormously reduces the risk of relapse and has therefore proven itself as a solid therapy pillar.
Here you will find more information:
- Therapy for breast cancer
- Chances of a cure for breast cancer

Purpose of radiation therapy
The purpose of radiation is to kill isolated tumor cells that are still in the body after an operation. This is to prevent the likelihood of local neoplasm (relapse). If there is no subsequent radiation therapy, the risk of relapse is up to 50%, with radiation it is only 5 to 10%. Therefore, radiation has now proven to be an integral part of breast cancer therapy.
Several studies are currently investigating whether, under certain circumstances, it may be indicated to dispense with radiotherapy (radiation). However, this has not yet been confirmed.
For more information, see: Treatment with radiation therapy
When does breast cancer have to be irradiated?
Radiation therapy for breast cancer can be used for inoperable tumor types, i.e. primarily, in addition to an operation or palliative, i.e. accompanying, relieving pain and improving quality of life. In the case of breast-conserving therapy or surgery, in which not the entire breast but part of the glandular tissue is removed, radiation therapy is always relevant because it lowers the risk of tumor recurrence in the mammary gland tissue.
After a complete surgical removal of the breast, irradiation is recommended if there are more than 3 affected lymph nodes, if the patient is under 40 years of age, if the tumor has spread to lymph or blood vessels, or if it has not been possible to achieve complete freedom from tumors at the cellular level.
In palliative terms, radiation is used to relieve pain or reduce the size of tumors.
In addition, it is possible to irradiate the breast affected by the tumor during the operation with the mammary gland or wound open. With a few exceptions - such as older patients, very small tumors, no affected axillary lymph nodes - it is a supplement to external radiation and shortens the duration of radiation therapy after an operation.But it does not replace them.
Further irradiation
Depending on a patient's individual diagnosis, it may also be necessary to irradiate areas of the body other than just the chest.
In addition, radiation therapy of the lymphatic drainage is often carried out, which usually affects either the armpit or the area just below the collarbone. This is because a breast tumor is the first to spread to these areas.
Distant metastases (daughter tumors) from breast cancer can also be addressed with radiotherapy (radiation), which in this case mostly only serves to relieve pain or avoid secondary diseases (such as broken bones in the case of bone metastases).
Post-irradiation after mastectomy
Radiation therapy does not necessarily have to be carried out after the breast has been completely removed; the assessment of the attending physician is required here. After such an operation, radiation is usually only connected if the tumor was very large or had already affected the chest muscles and / or skin.
Sole irradiation
Treating breast cancer with radiation alone is rather the exception. This route is usually only taken if an operation proves to be unsuitable for certain reasons.
This can happen, for example, with patients who refuse an operation on principle or with those who would be exposed to an above-average risk during an operation because of their advanced age or other diseases. The radiation dose used for this primary therapy is higher than that used in addition to surgery. For this reason, changes and scarring of the skin or a reduction in the size of the breast are more common here.
All about irradiation
What are gray?
Gray is a unit that occurs in physics. This unit is derived from a formula for determining the absorbed dose. The unit is defined as one joule per kilogram. This corresponds to a gray. The absorbed dose is created by ionizing radiation.
This is used in medicine as part of radiation therapy, for example, for various types of tumors or as a nuclear medicine therapy. To understand the absorbed dose, it is important to know that radiation therapy uses doses of 20,000-80,000 milligray (mGy). Approximately 5000 DNA damage occurs in a cell for each Gray radiation dose.
Read more on the subject at: Effect of radiation therapy
Will you be on sick leave during the irradiation?
It is up to each patient whether they want to or can go to work. Because every body copes with this phase in a different way. Some patients do not mind the radiation. You don't want to get too fixated on therapy and still be busy with other things. Others feel very tired after a few sessions and need longer periods of rest.
In addition, some patients are bothered by the fact that they are not allowed to wash. This is handled differently for each irradiation. Instead, you can powder yourself. Getting sick leave is therefore not a problem if the patient is not feeling well. It is often several months. Since the statutory health insurance pays money after 6 weeks, this is not an obstacle to getting sick leave.
Duration of exposure
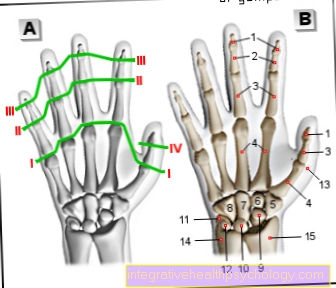
Radiation therapy must be well planned in order to precisely localize the area affected by the tumor and to spare neighboring tissue as much as possible. For this purpose, the patient is positioned accordingly by medical-technical X-ray assistants. Before the start of an irradiation cycle, the exact position of the tumor is determined and marked in test images so that the patient is positioned in the same way with each irradiation. This enables the maximum radiation dose to reach the tumor tissue while at the same time protecting the surrounding tissue as best as possible.
All other people leave the room during the treatment. However, the patient is monitored using a camera and microphone system. In total, the irradiation itself only takes a few seconds, but storing and adjusting the device takes 10 to 15 minutes.
For more information, see: Radiation therapy planning
How often is irradiation?
The number of irradiations is determined individually according to the size and type of the tumor in a radiation plan.
Radiation treatment after surgery usually starts with 28 sessions that are carried out once a day, five days a week. The number of sessions can, however, be adjusted to the patient and the response of the tumor and result in more than 30. For patients for whom the daily drive to the clinic is a relevant problem, higher doses can be used in some sessions, thus reducing the total number of sessions.
What are the chances of recovery from the radiation?
The prospect of a cure for tumor diseases cannot only be attributed to radiation therapy, but also depends on many different factors. These include the size of the tumor, the number of affected lymph nodes and any metastases that may be present. Based on this, a statement can be made about the intention with which breast cancer is treated, i.e. curative (healing) or palliative (soothing).
In breast cancer, the chances of recovery also depend on the type of tumor, which is determined using a microscope, and on whether there are docking points (hormone receptors) that can be treated with other drugs. Radiotherapy is often recommended in view of a local recurrence, i.e. a recurrence of cancer cells at the operated site, or after chemotherapy. Without radiation, local recurrence occurs in up to 50% of the cases, after radiation therapy only in up to 5 - 10% of the cases.
Read more on the subject at:
- Chances of recovery in breast cancer
- Breast cancer prognosis
Can I smoke during radiation therapy?
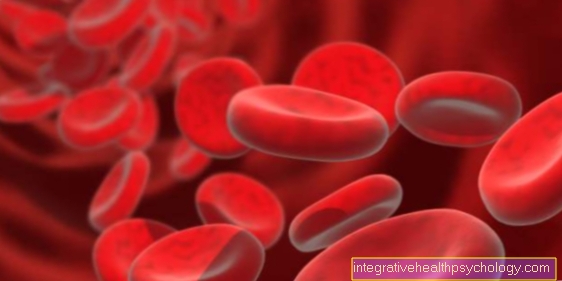
Radiation therapy is most effective in healthy blood and tissue saturated with oxygen. Smoking greatly reduces the amount of oxygen in the blood and reduces the effectiveness of the therapy.
Smoking is known to be a cause of many malignant and benign diseases. It is one of the most important reasons for the development of carcinomas in particular. For this reason, it is always advisable to refrain from smoking, especially with regard to radiation therapy. If this is not possible, at least one should try to reduce the number of cigarettes as much as possible.
Can you drink alcohol during radiation therapy?
There is no absolute ban on alcohol during radiation therapy. Consumption is possible in moderation in the form of 1-2 glasses of wine occasionally. Because alcohol is highly damaging to healthy tissue in addition to radiation therapy, it should not be consumed in esophageal cancer.
Side effect of radiation
The majority of patients tolerated the dose of 50 Gy. Symptoms that can often occur after radiation therapy are reddening and hypersensitivity of the skin on the treated area.
Reddening of the skin is an acute complication of radiation therapy. This can manifest itself symptomatically as a burning sensation in patients. Inflammation or reddening of the skin or mucous membranes are often reversible. It is important that you inform your doctor about the consequential damage of radiation therapy.
It is recommended not to wash the affected skin frequently. Furthermore, massive drying of the skin irritates it, which is why it is important to just dab it off. Further mechanical irritation in the form of sunlight, perfume, deodorants or hair removal should be avoided. Instead, it is helpful to wear loose clothing, powder the skin at higher temperatures and use pH-neutral, unscented cream.
When the treatment is finished, however, these disappear completely. In addition, some people suffer from tiredness, exhaustion and malaise after exposure to radiation - the so-called "radiation hangover". Women are much more likely to miss menstruation (70%).
In one percent of cases, pneumonia can occur several weeks after irradiation with shortness of breath, dry cough, coughing up blood and possibly a fever. Like breast inflammation, this is rarely the case. With a very high absorbed dose, broken ribs or disorders of the nerves supplying the arm are described in 1-2% of cases. This would only occur at energy doses of over 50 gray.
Permanent changes can very rarely occur, such as E.g.:
- Scarring
- Tanning (hyperpigmentation) of the skin
- dilated skin vessels
or - a reduction in the size of the breast
Read more on the subject at: Side effects of radiation
Hair loss
The radioactive rays during radiation therapy not only hit the region to be treated or the tumor, but also healthy cells and tissues. Since the head of breast cancer patients is not in the radiation field, hair loss on the head is not an expected side effect.
In contrast, the armpit hair is affected here. It takes several months or years for the hair cells to regenerate and emerge.
While this is less of a problem in the armpits, the attending physician should inform or pass on the possibilities of hair loss to the patient in the event of skull irradiation, for example if brain metastases occur.
What pain can be expected during the radiation treatment?
In radiation therapy, a distinction is made between acute radiation reactions and chronic radiation damage. Depending on their severity, both can cause pain.
The consequences of the irradiation depend very much on the irradiation field. Skin reddening can result from long-term exposure. These do not necessarily have to lead to pain. Arm or chest edema, which is caused less by the radiation itself and more by the operation, is more uncomfortable. Furthermore, some patients also report pain in the chest and around the chest, which are caused by the radiation and which sometimes last for a long time.
Does taking selenium make sense during irradiation?
Selenium is one of the trace elements. It has an important function in many organs. Among other things, it plays an important role in the formation of thyroid hormones, in the maturation of sperm and in the interception of free radicals in the event of oxidative stress. Selenium can protect healthy cells during radiation therapy. During treatment with radioactive rays, not only tumor cells but also neighboring tissue are damaged and free radicals are created in this process. These can additionally damage healthy tissue that is distant via the bloodstream. Selenium is able to catch these free radicals and reduces the side effects of radiation therapy without weakening the effect.
What are the possible long-term effects of chest radiation therapy?
Radiation therapy may require several sessions, for example up to 36 or more sessions, depending on the size and location of the tumor. Depending on the absorbed dose, the adjacent skin of the affected region is also damaged.
This can also influence the mucous membrane or organs. Occasionally there are permanent pigment disorders of the skin and disorders of the sweat glands. In addition to harmless reddening of the skin, so-called fibrosis of the breast can occur in ten percent of cases. This appears as a connective tissue remodeling of the mammary gland tissue.
In earlier years, inaccurate radiation fields caused more frequent damage to the heart and thus increased cardiac mortality. In the last 15 years this has hardly played a role anymore due to better, tissue-saving radiation methods.
In addition to breast-specific radiation, there can generally be inflammation of the mucous membranes in the mouth, esophagus or intestine, which can be expressed, for example, by diarrhea. Irradiation of the bone or the blood-forming bone marrow results in anemia, reduced numbers of platelets and white blood cells. Since the breastbone is a relatively small bone when it is in the radiation field, there are usually no serious effects.
In rare cases it can happen that the radiation causes a second tumor in the breast or a tumor on the opposite side.
- Find out more about the Long-term effects after radiation treatment.