Bacteria in the blood - how dangerous is it?
introduction
The appearance of bacteria in the blood (bacteremia) is a common phenomenon and can occur as a result of harmless activities such as brushing your teeth. Their sole proof is primarily not an indication for treatment.
A physical reaction of the immune system with simultaneous detection of bacteria or their toxins in the blood must be treated immediately. It is a potentially life threatening disease. If septic shock occurs, any delay before the start of antibiotic therapy means a worsening of the chances of survival by around eight percent per hour.
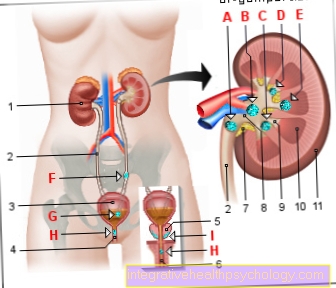
Severe sepsis occurs when the pathogens or their toxins spread in the body and spread to organs. In such a case there is an acute failure of at least one, sometimes vital, organ. In addition to circulatory failure (generally "shock"), failure of the respiratory system and renal insufficiency are in the foreground.
One speaks of septic shock when not just one organ but several can no longer fulfill their function. The underlying cause is a greatly reduced blood flow to the tissue. This particularly affects the kidneys, lungs and liver.

What symptoms do I have if I have bacteria in my blood?
Bacteria in the blood can cause a wide range of symptoms. This mainly depends on how many bacteria get into the blood and how long they stay there. Even after vigorously brushing your teeth, a small amount of bacteria can get into the bloodstream. However, this usually does not cause any noticeable symptoms.
In addition, the bacteria are usually eliminated quickly by the body. If large amounts of bacteria get into the bloodstream, this can become noticeable as fatigue or a feeling of illness. However, the body can react to large numbers of bacteria in the blood with severe symptoms such as fever or severe circulatory problems. This is usually referred to as sepsis.
It should be noted that it is difficult for bacteria to get into the bloodstream in a healthy body. Therefore, a local infection, such as gum inflammation, must usually take precedence. This original infection will of course also cause symptoms.
Read more about this: Symptoms of blood poisoning
Bacteria in the blood if you have a high fever
Sepsis with bacteria in the blood cannot always be clearly identified in its early stages. The symptoms, such as high fever, are initially unspecific. This means that the symptoms of the illness can also be associated with many other illnesses. A high fever also occurs, for example, with a flu-like infection or the flu.
Typically there is a rapid deterioration in the general condition. Body temperature can rise to well over 38 ° C within a short period of time. Usually those affected suffer from chills at the same time.
In addition to the rise in fever, other unspecific symptoms can include a high pulse and breathing rate, altered consciousness, uncertain pain in various parts of the body and signs of inflammation at the site of the original infection. However, sepsis is not always associated with a high fever. In some people, the body temperature drops below normal.
Read more on the subject below Causes of fever
Bacteria in the blood and joint pain
Bacteria in the blood can be linked to joint pain for several reasons. Bacteria can first infect a joint and then get into the bloodstream from this local inflammation. An infected joint is very painful; it can be red and swollen. On the other hand, it is also conceivable that bacteria in the blood could infect a joint. In this case, bacteria first develop in the blood and then the joints are affected. Borrelia can also affect joints. This is known as Lyme arthritis.
Borrelia usually get into the affected joints via the blood. Bacteria do not always have to be in the joint to cause damage. In so-called reactive arthritis, the joints become inflamed after a bacterial disease has been overcome. Typically this happens after infections with gonococci, also called gonorrhea, chlamydia or after a gastrointestinal infection. In this case, it is not the pathogens that attack the joints, but the immune system. It is unclear why this happens. The pathogens can, but need not, be detectable in the blood.
Read more on this topic at: Joint pain
Are bacteria in the blood contagious?
In order to be able to clarify this question unambiguously, it is first important to realize that an infection is understood as the active or passive transmission of a pathogen into another organism, such as the human body. If the pathogen remains in this and can then multiply, what is known as an infection occurs, which can be followed by the manifestation of the correspondingly associated clinical picture. The presence of a risk of infection when dealing with sick people is not equally pronounced for every disease and in every stage of the disease, but primarily depends on the excretion of active pathogens by the patient. In principle, every sick person who "viable“Pathogen is potentially contagious, regardless of its clinical picture.
The transmission of infectious pathogens is usually possible through contact with body fluids and the excretions of the sick person, an example of this is the spread of cold viruses via the secretions of the nasal and throat mucous membranes formed in connection with the cold, which are expelled by sneezing and coughing.
The transmission and subsequent infection is possible through direct contact with the sick person on the one hand, but also through indirect contact with the body secretions of the person concerned, for example via door handles. Other examples of diseases in which the patient's excretions are particularly infectious are most gastric orBowel disease associated with vomiting or diarrhea.
Diseases such as HIV are particularly associated with the detection of the pathogen in the blood. In these cases, contact with the patient's blood is to be regarded as contagious, and transmission via uninjured skin is very unlikely. The situation is similar with most of the pathogens that can be detected in the blood. Accordingly, a person in whom the detection of active bacteria in the blood is positive is in principle infectious and there is a risk for others to become infected with them. It should be noted, however, that the transmission of these pathogens is normally only possible through contact with body fluids, especially the blood of the person concerned.
However, patients in whom the bacteria entered the blood indirectly via colonization and infection of a tissue with a subsequent transition into the blood usually have a greater risk of infection, as in these cases the infection with the pathogens can originate from the blood and the primarily colonized tissue. Let us return to the example of pneumonia already mentioned above: in this case, infection with the pathogens in this patient would come from not only the blood but also the bronchial and throat secretions formed as part of his lung disease, which he usually expels through strong coughing.
Duration
The length of time that bacteria are in the blood can vary widely. If a small amount of bacteria is washed into the blood, these are usually eliminated immediately by the body. This can happen, for example, during a visit to the dentist. Bacteria often enter the bloodstream from a local source of infection. This can be, for example, inflammation of the gums or tonsils. If this focus of inflammation persists over a longer period of time, bacteria can repeatedly get into the blood. In this case, bacteria can remain detectable in the blood until the original focus of infection has been successfully treated.
root cause
The presence of bacteria in the blood is not necessarily associated with symptoms, let alone a serious clinical picture. If bacteria are present in the blood, this can range from a symptom-free picture to a life-threatening condition of blood poisoning (sepsis) with multiple organ failure are sufficient.
In principle, bacteria can enter the bloodstream in various ways. Above all, it should be noted whether the bacteria get directly into the blood of the person affected or first settle in a tissue. In general, bacteria can get into the blood of a person through a direct opening of a blood vessel, for example in the event of an open injury or as part of a deliberate vascular puncture during a medical procedure. A typical example of the direct penetration of bacterial pathogens into the bloodstream is the ingestion of Clostridium tetani as a result of an accident. This infection occurs when the open wound comes into contact with contaminated soil.
Bacteria can also colonize tissue, but also primarily ingested via other routes (food, breathing) and trigger a disease such as pneumonia, in the course of which the pathogen can also pass into the bloodstream. This complication usually occurs when the patient is very weakened by the previous illness and his immune system with the causative pathogens "Overwhelmed“Is so that this process is feared.
The transfer of bacteria in the oral flora after or during tooth brushing is usually harmless, but as a result can also lead to heart valve inflammation. This usually harmless example illustrates how differentiated the detection of bacteria in the patient's blood is to be interpreted.
E. coli bacteria
E. Coli is a bacterium that is part of the natural intestinal flora even in healthy people. In some studies, E. Coli was the most common bacterium found in the blood. E. Coli is a common cause of urinary tract infections and diarrhea. There are a number of different E. coli strains. While many are relatively harmless to humans and do not leave the intestines, others can cause serious illnesses. If E. Coli get into the blood, they can cause life-threatening sepsis. But the bacterium does not always have to reach the bloodstream. Often only toxins produced by E. Coli get into the blood, not the bacterium itself.
Read more on this topic at: Escherichia coli
Bacteria in the blood after an operation
After an operation, the risk of infections with bacteria in the blood is increased. Every surgical procedure involves the risk of foreign material being brought in and damage to certain body structures nosocomial infection (Hospital infection).
It is therefore a so-called postoperative complication. For example, bacteria that actually occur in the intestine, such as E. coli, can pass into the blood after an operation in the abdomen. One then speaks of an endogenous infection, in which the bacteria in your own body reach another location.
Every postoperative wound has an increased potential for infection, from where the pathogens can spread into the blood. Such an infection can also be triggered by endogenous, but also by exogenous (from outside) germs. In addition to enterococci, the most common pathogens include Staphylococcus aureus (especially MRSA) and enterobacteria.
In particular, inserted implants, for example knee joint prostheses, as well as interventions in the abdominal cavity or on the heart are associated with an increased risk of sepsis. Surgical sepsis usually occurs within 24 hours. In the best case scenario, the symptoms that occur are recognized a short time later and treated with an antibiotic that covers the broadest possible spectrum. Each additional hour that passes by worsens the chances of survival.
If the focus of infection is identified, further surgical intervention may be necessary to remove the focus.
Bacteria in the blood after chemotherapy
The likelihood of bacteria appearing in the blood is increased after chemotherapy. The majority of chemotherapy drugs (Cytostatics), which are supposed to fight the cell growth of malignant cells, is not only directed against tumor cells, but unfortunately also against the body's own cells. Other rapidly dividing cells of the immune system and blood formation in the bone marrow are also affected.
The blood count must be checked regularly during chemotherapy treatment. A special focus is on the leukocytes, the white blood cells that are responsible for the proper functioning of our immune system. As the number of white blood cells decreases, the risk of infection increases. This often first announces itself with a fever. A bacterial infection can turn into sepsis more quickly due to the weakened immune system. If the white blood cells are likely to be affected, antibiotics can be used as a precaution against the most common pathogens.
Patients with acute leukemia or receiving high-dose chemotherapy are usually hospitalized during treatment. There is a particularly high risk of infection here. In this way, the onset of sepsis is recognized as early as possible.
Please also read our topic on this Chemotherapy side effects
Diseases occurring in connection
There are many different clinical pictures that are inextricably linked with the detection of bacteria in the blood.
- The first example is bacterial endocarditis (Heart valve inflammation), which occurs more frequently in patients with previously ill, usually also operated, heart valves. The inflammation of the affected heart is preceded by a deposition of bacterial pathogens in the blood on the heart valves, which is more likely to occur with changed / scarred valves. These bacteria find good growth conditions on the heart valves, as they are constantly bathed in nutrient-rich blood. Endocarditis very often occurs as a result of an invasive dental procedure, since large amounts of bacteria from the oral cavity can get into the bloodstream through the injury and opening of the gums that are well supplied with blood. For this reason, preventive antibiotic therapy when there are risk factors, such as an artificial heart valve, is of great importance and should be carried out after dental procedures. Typical symptoms are general signs of an infection, such as fever, but also the appearance of new, previously unknown heart murmurs, as well as signs of increasing cardiac insufficiency are part of the clinical picture. Normally, if a bacterial heart valve inflammation occurs, therapy is carried out with the aid of an antibiotic.
Learn more about: Endocarditis prophylaxis
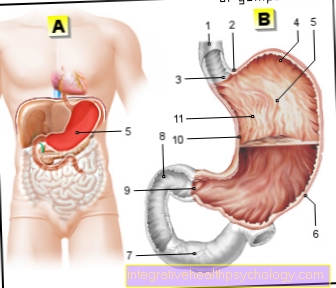
- The presence of tetanus disease, also known as tetanus, has already been mentioned, which is related to the detection of the bacterium in open wounds and the release of its nerve-damaging poison. This initially leads to unspecific symptoms such as headaches, dizziness or sweating. Only in the further course do the typical, spastic symptoms of paralysis appear, in which the muscles cramp in an uncontrolled manner and the patient no longer has the opportunity to relax his muscles. An acute danger to life arises, for example, when the respiratory muscles are also affected. The clinical picture is triggered by the poison in the blood, so that in addition to relaxing substances, an antidote is also used therapeutically. In contrast to Clostridium tetani, which gets directly into the bloodstream through open wounds, the bacterium Tropheryma whipleii initially releases a "local“Disease of the stomach and upper small intestine as it is mostly absorbed through the mouth. The pathogens are caused by cells of the body's own defense system, the Macrophages, ingested, remain in the mucous membrane and cause problems with the absorption of nutrients from food. As a result, there are structural changes in the intestinal mucosa and, secondarily, the bacteria penetrate the bloodstream. The bacteria can spread throughout the body via the bloodstream and affect many other organs. This can trigger further, organ-specific symptoms, such as joint problems or increasing shortness of breath during exercise. The clinical picture of Whipple's disease is treated with antibiotics, whereby symptomatic therapy is also carried out by giving, for example, vitamins that could no longer be absorbed through the changed intestinal mucosa at times.
- The last but particularly feared example of a disease associated with the detection of bacteria in the blood is so-called sepsis, Colloquially also blood poisoning called, which in the course of an overreaction of the body's own defense system is accompanied by the failure of several organs and can thus be life-threatening. It usually begins with a "harmless“, Localized disease that does not heal due to a weak immune system, but gets out of control so that the pathogens can get into the bloodstream. The strong reaction of the immune system ultimately triggers the life-threatening complications that shouldn't actually occur. The main problem with blood poisoning is that it usually occurs as a result of its initially very unspecific symptoms (fever, Feeling sick) is recognized very late. In the meantime, the immune system's response is well advanced, so that the patient is already showing signs of shock, such as a drop in blood pressure and an increased pulse. The affected person must receive intensive care as soon as possible in order to stabilize the patient's circulation, fight the bacteria with antibiotics and reduce the risk of failure of important organs such as the lungs, kidneys or liver.
Periodontal disease
Periodontitis is an inflammation of the periodontium. This is usually triggered by bacteria. These bacteria can also get into the bloodstream. Since periodontitis can persist for a long time, bacteria can repeatedly get into the blood. As a result, the body is exposed to a kind of constant stress, which can have many harmful consequences. The inflammatory reaction increases the risk of cancer or heart attack, among other things. Therefore periodontitis should be treated if possible.
Read more on this topic at: Periodontal disease
Which antibiotics help?
Antibiotics are typically used against bacteria. Therefore, they are well suited for therapy against bacteria in the blood. However, not every antibiotic is effective against every bacterium. The widespread use of antibiotics has also led to an increasing spread of antibiotic-resistant bacterial strains. It is therefore not clear which antibiotic should be used against bacteria in the blood. To solve this problem, blood is first drawn from which the bacteria can be isolated and grown. Then you can test the resistance of the bacteria in a laboratory. In this way, the doctor can safely decide which antibiotic is effective in a specific case. If there is not enough time for such a procedure, calculated or empirical antibiotic therapy can also be carried out. Here you choose an antibiotic that is effective against most typical pathogens of a disease. It is also important to know through which port of entry the bacteria were likely to get into the blood.
More information on this topic: Blood poisoning therapy
diagnosis
The presence of bacterial pathogens in a patient's blood is only possible through a special laboratory examination, a so-called Blood culture, possible after removal from a venous vessel. The blood culture is used to grow bacteria that may be in the blood. Ideally, the blood is drawn at the beginning of a rise in fever, as this is usually accompanied by an increase in the concentration of bacteria in the blood, so that the probability of a positive and specific detection is greater. In addition, it should be taken several times with a minimum interval of 30 minutes. Here, special and sterile bottles are used, which on the one hand contain suitable nutrient media and on the other hand the aerobic (with oxygen) or anaerobic (with the exclusion of oxygen) Contain the gas mixtures required by bacteria. Since there is usually no knowledge of the pathogen, at least one aerobic and one anaerobic culture bottle are always filled with the patient's blood. After they have been taken and transported to a microbiological laboratory, the samples are placed in an incubator at body temperature (approx. 37 ° C) kept to allow possible bacteria to grow in the culture bottle.
The occurrence of bacterial growth is detected with the help of special devices which generate an alarm even if the gas mixture contained in the bottles changes minimally as a result of bacterial growth. If the pathogen was successfully cultivated, it can be identified and tested for possible resistance to antibiotics.
Read more on this topic at: Resistance to antibiotics
When examining the blood using a blood culture, incorrect diagnoses can occur, for example if the blood was contaminated by skin germs. Furthermore, it is possible that bacteria will not be detected because they are particularly sensitive and therefore cannot survive transport to the laboratory in the culture bottle. In addition, the result can be negative if the patient has already been treated with antibiotics or if the pathogens causing the disease are not bacterial.
Bacteria in the blood in children
Bacteria in the blood of children occur most frequently in infancy up to three years of age, although they can manifest themselves in a wide spectrum, as in adults, from a condition without symptoms to severe clinical pictures in the context of pneumonia or meningitis to the onset of blood poisoning.
Depending on the age, the function of the immune system and the vaccination status of the child, threatening clinical pictures are triggered by different types of bacteria in children; It is particularly noticeable that the decrease in the so-called network protection (Presence of antibodies against many pathogens that were transmitted from the mother to her unborn child during pregnancy) after the third month of life the spectrum of pathogens such as Echerichia coli (Intestinal germ) or salmonella to bacteria that, for example, have a lung (Streptococcus pneumoniae) or meningitis (Neisseria meninigtidis) can trigger moves.
If an infection with the bacterium Streptococcus pyogenes is suspected, a rapid test can easily be carried out at home. Read more about this under our article: Streptococcus rapid test
The response of the immune system to the bacteria that has entered the blood differs in children from that of adults only in a few ways: among other things, infants can develop hypothermia with body temperatures below 36 ° C instead of fever. If meningitis occurs Neisseria meningitidiswhich occurs much more frequently in children than in adults, includes not only fever but also the development of petechiae (small, pinhead-sized bleeding into the skin) by the transfer of the bacteria into the blood to the clinical picture.
Please also read our topic:
- Fever in the toddler
- Blood poisoning in the child
Bacteria in the baby's blood
Infection with bacteria in the blood in a baby is also called neonatal sepsis. Children who are born prematurely as well as those with a low birth weight have an increased risk of newborn sepsis. The child's immature immune system is particularly susceptible to external infections.
A "Early sepsis"is triggered before or during childbirth. Usually it is the intestinal bacteria E.coli or B-streptococci. A"Late sepsis"on the other hand occurs a few days to a week after birth. In the majority of cases it is also bacteria from the mother's birth canal.
During pregnancy and in the period after the birth, the newborn child receives a so-called loan immunity from the mother ("nest protection"). Antibodies from the mother are passed on to the baby via the placenta during pregnancy and via the breast milk during breastfeeding.
If bacteria or other pathogens are not adequately fought, they can spread in the blood. The immune system reacts with a strong inflammatory reaction. Without timely treatment with antibiotics, the loss of function of vital organs can lead to death within a few hours. As soon as bacteria are suspected in the baby's blood, an "empirical" antibiotic therapy is started. This means that it has not yet been possible to precisely identify the underlying bacterium and that the therapy is therefore directed against the statistically most common bacteria in newborns.





















-buschmcke.jpg)