Symptoms of a herniated disc
introduction
Symptoms and ailments that a disc prolapse are different and manifold. The most common cause is pain. Mostly these are indicated as pressing and pulling in the back.
You can also find many alternative causes for which a pulling in the back can trigger under our topic: Pulling in the back

Most pain symptoms associated with a herniated disc can only be localized inaccurately.
Patients usually point to areas of the spine that span 4-5 vertebrae (med. as L4 / 5 designated) cover. This helps to delimit the approximate area of the spine, but the exact vertebra can only be determined by means of imaging.
The pain indicated is often described as pulling towards the foot. Sometimes it is stated that they pull up to the tip of one half of the body. Almost always, however, patients complain that the pain is moving towards the buttocks.
Read more on the topic: pain in the back
Symptoms of a herniated disc
The symptoms of a herniated disc include:
- Symptoms of pressure against the nerve root:
A Compression of the nerve roots triggers intense pain that can radiate into arms and legs. With this pain, sensory disturbances can also occur. Depending on the stage and extent of the herniated disc, symptoms can also result in reduced muscle strength or paralysis in individuals.
Read more about the topic here: Nerve root irritation - Symptoms of pressure against the spinal cord:
Depending on the location of the herniated disc, the symptoms of the disc vary. Herniated discs in the thoracic spine can cause sensory disturbances, cramps or cause paralysis, whereas a herniated disc in the lumbar spine can cause bladder paralysis. - Symptoms of pressure against nerve fiber bundles, the horse's tail (Cauda equina):
Lack of function of the bladder and rectum function, sensitivity disorders in the anal and / or genital area.
For more information, see: Herniated disc with nerve damage
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
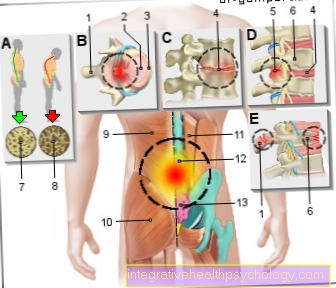
Illustration of the symptoms of a herniated disc

Disc prolapse -
Symptoms
- Fifth cervical vertebra
- Sixth cervical vertebra
- Seventh cervical vertebra -
Vertebra prominenta - Twelfth thoracic vertebra -
Vertebra thoracica XII - First lumbar vertebra -
Vertebra lumbalis I - Fourth lumbar vertebra -
Vertebra lumbalis IV - Fifth lumbar vertebra -
Vertebra lumbalis V - Five sacral vertebrae
(merged) - Pear-shaped muscle -
Piriformis muscle - Sciatic nerve -
Sciatic nerve
Sections of the spine:
C - neck area (cervical)
T - chest area (thoracic)
L - lumbar region (lumbar)
S - sacrum area (sacral)
You can find an overview of all Dr-Gumpert images at: medical illustrations
Symptoms of a herniated disc of the cervical spine

The Cervical spine (Cervical spine) consists of 7 cervical vertebrae, which can lead to a herniated disc. The term is a synonym for the herniated disc of the cervical spine cervical disc prolapse or NPP of the cervical spine called.
At the cervical spine it comes in comparison to Lumbar spine less often to one Prolapse. In the case of a herniated disc, the lower cervical spine is affected more often than the upper.
Most of the herniated discs are found in the segments C5 / 6 and C6 / 7.
This is partly because the lower part is moved much more and more complexly.
The symptoms vary depending on the severity of the herniated disc. If he is just very small, it can be neither annoy and that Spinal cord be compressed, causing a herniated disc completely symptomless runs and remains undetected for years.
Otherwise typical symptoms such as pain and paresthesia in the neck, shoulder and arm area occur. The pain is sharp and can affect both Neck area be centered than about that Shoulders and poor Radiate to the fingertips.
A herniated disc in the cervical spine that is severely pinching a nerve root can cause extremely severe pain.
Sometimes it is described by patients as dull, pulling or pressing. Under Paraesthesia one understands a painful discomfort, which is a collective term for body sensations such as tingling, numbness and temperature perception disorders.
Furthermore, there is a knocking pain on the corresponding cervical vertebrae.
The stage of the cervical disc herniation is reflected in the type of Symptoms again. The pain described is the first sign of a herniated disc. First, it occurs in the immediate vicinity of the cervical vertebrae, i.e. in the neck / neck area.
With time the Pain in shoulder and arms up to the hands to broadcast.
The more nerve fibers are compressed by the incident, the stronger the symptoms become, so that the first feelings of numbness and a slight tingling sensation occur. The herniated disc is serious when it actually comes to muscle weakness and restricted mobility; then a doctor should definitely be consulted.
Ultimately, a herniated disc of the cervical spine can be so serious that it leads to complete failure symptoms or Paralysis comes. This is seldom the case, but in principle possible. You can then also from one Paraplegic syndrome speak. Not only are nerves compressed, but the entire diameter of the spinal cord running centrally in the spinal canal is damaged, resulting in paralysis of the muscles and a loss of sensitivity below the lesion.
In general, a worsening of the pain symptoms in the case of a herniated disc of the cervical spine can be provoked and intensified by tilting the head to the side and / or tilting back.
The lying position is also perceived by patients as very uncomfortable due to the increased pain intensity, so the patients suffer from greater pain at night. Often an unconscious posture is adopted, such as holding the head at an angle, depending on which side is affected by a herniated disc, as this may make the symptoms somewhat more bearable.
Read a lot more information on this topic under: Symptoms of a herniated disc of the cervical spine
Neck pain with a herniated disc in the cervical spine
The neck pain is a typical symptom of a herniated disc in the cervical spine. The intensity of the neck pain depends on how severe the herniated disc is. The painful perception without the appearance of other symptoms such as Sensory disturbances, for example tingle and Numbness, and Reduced strength in the neck-, shoulder -and Arm area tend to speak more for you lighter disc herniation.
The development of neck pain due to a herniated disc in the cervical spine comes about as follows: By a increased pressure load the outer fiber ring of the intervertebral disc can be damaged more and more until it is ultimately so unstable that the gelatinous core emerges through the fracture site. This works with a Compression of the spinal nerves along, whereupon a pain stimulus is triggered. If such a herniated disc occurs in the area of the cervical spine, the symptoms can primarily take the form of neck pain, but also a headache, Visual disturbances or Ringing in the ears express. The nature of the pain in the neck can vary individually. Some sufferers report stabbing and suddenly shooting pain. In contrast to this, however, diffuse and rather dull pain are described again and again.
The exact localization of pain in neck pain due to a herniated disc is not always possible. The neck pain also often radiates to the head and shoulders. Not infrequently the pain even extends into the arms. An increase in pain intensity is provoked by further strain and movement in the area of the cervical spine, so that those affected often have a Relieving posture take in. This, however, begins a vicious circle, since the gentle posture is a Tension which can result in neck pain. It is therefore very important to treat neck pain adequately in order to get rid of symptoms as quickly as possible.
Read more information on the topic Neck pain
Symptoms of a herniated disc in the C5 / C6 area
A herniated disc in the C5 / 6 cervical area may be due to a increased pressure load on the Band washers by Bad posture or traumatic events arise. As a result, the symptoms are typical Paresthesia, such as numbness, "tingling" and pain in the corresponding skin area (=Dermatome; Skin area that is supplied by sensitive fibers of a specific spinal nerve). If the spinal nerve C5 is compressed by the herniated disc at the C5 / 6 level, one can also use a C5 syndrome speak which with Tingling sensations in the shoulder -and Upper arm area goes hand in hand, as the C5 dermatome is located here. Another symptom is an extinct one or only once attenuated „Biceps tendon reflex“.
However, if the spinal nerve C6 is compressed by the herniated disc, it is a C6 syndrome. Typical for this are on the one hand Sensitivity Disordersthat differ from Elbow Outside along the outer forearm side until thumb extend and partly also on index finger can be felt. On the other hand, as with the C5 syndrome, a reflex can fail here, in this case the so-called "radius periosteal reflex". Since the spinal nerve also gives off motor parts, it is possible that those affected with a herniated disc at the C5 / 6 level of a Weakness in lifting the arms to report.
Symptoms of a herniated disc in the C6 / C7 area
A herniated disc in the cervical area at the level of C6 / 7 manifests itself with symptoms similar to a herniated disc at the level of C5 / 6. In addition to the characteristic sensitivity disturbances in the area of the dermatome C6, namely from the outer elbow along the forearm to the thumb and parts of the index finger, the "radius periosteal reflex" disappears.
If, on the other hand, the spinal nerves C7 are compressed by the herniated disc, this leads to abnormal sensations in the corresponding dermatome C7. This extends over both the front and back of the forearm and hand. More precisely, over the entire middle finger and the adjacent skin areas of the ring and index finger. The reflex that fails in the context of a herniated disc in C7 syndrome is the "triceps tendon reflex".
Read more about this at: Herniated disc of C6 / 7
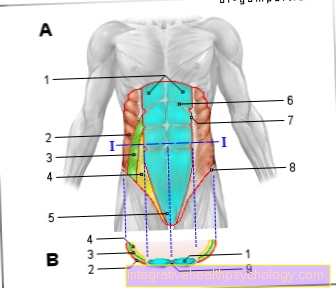
The symptoms in the lumbar spine and leg

The most common localization of a herniated disc is in the lumbar spine. The lumbar spine has a significantly higher risk of prolapse than the cervical and thoracic spine.
In principle, a herniated disc can occur in all 5 lumbar vertebrae, but it preferably occurs between the 4th and 5th LWK (herniated disc L4 / 5) or between the 5th LWK and the 1st sacrum (Sacrum) (Herniated disc L5 / S1).
The main symptom is the classic, severe lower back pain with a radiating component to the buttocks, along the thigh, over the knee and to the tips of the feet. The pain radiates particularly when the sciatic nerve, the most powerful nerve in our body from the L4 to S3 nerve roots, is compressed.
The character of pain can be stabbing, pulling, but also dull and pressing. Most often the pain is sudden, e.g. when lifting something heavy. In general, the pain symptoms can be aggravated by certain movements, so that patients adopt a relieving posture. Sneezing, coughing, and straining are also very uncomfortable and make the sharp pain in the back region worse.
In addition to the pain, neurological failures such as tingling and numbness can also occur. A special form of paresthesia (tingling) is called breeches anesthesia due to its location. This means the loss of sensitivity in the buttocks and genital area and on the inside of the thigh. The reason for this is nerve root damage to the sacral segments S1-3.
Depending on how severe the herniated disc of the lumbar spine and the compression of the surrounding structures is, it can lead to paralysis in the leg region (herniated disc with symptoms in the leg). As a rule, patients notice these serious symptoms by stumbling more often or by having no stability in their knees when climbing stairs. The patient can be asked to stand on their heels and then on their toes to check.
If there are any difficulties, a herniated disc of the lumbar spine should definitely be clarified using an MRI of the lumbar spine.
The most common herniated discs of the lumbar spine occur in the L4 / 5 and L5 / S1 segments.
But not only the leg muscles with symptoms of paralysis worry the patient, the nerves that regulate the urinary bladder and bowel function can also be affected, resulting in incontinence (= urination and bowel movements can no longer be controlled). The incontinence mostly occurs in connection with the already mentioned breeches anesthesia. In addition, it can lead to a disruption of the sexual function.
Read more on the subject here Breeches anesthesia.
Read more on the topic:
- Symptoms of a herniated disc in the lumbar spine
and - Herniated disc L4 / L5
The herniated disc in the lumbar spine can also trigger a so-called cauda equina syndrome, which should be recognized urgently and, if left untreated, can lead to permanent paraplegia. We therefore recommend our website for further information: Cauda equina syndrome - do I have paraplegia?
Symptoms of a herniated disc at the L3 / L4 level
Everyone feels pain and therefore it is part of every herniated disc. Usually the pain has a stabbing quality.
In addition to the pain, abnormal sensations can be noticed. These include feelings of tingling or numbness. In serious incidents, muscle paralysis - primarily in the thighs - can occur.
You can find out more about this at: Disc herniation of L3 / L4
Symptoms of a herniated disc in the L4 / 5 area
A herniated disc L4 / 5 is the second most common in the human body. Only a herniated disc L5 / S1 is more common.
In the case of a herniated disc L4 / 5, the L4 or L5 nerve root can generally be affected. In most cases the 5 root is affected.
Depending on where the patient states the symptoms of the restricted mobility, it can be concluded which area of the spine is affected by the herniated disc.
An example is the disturbed foot lift. If the patient is no longer able to do this, a herniated disc of the lumbar spine between L4 / 5 can be assumed. The intervertebral disc is pushed between the two vertebral bodies 4 and 5 and presses the nerves L5 running there, which leads to the dorsiflexor weakness described.
Pain that ends in the big toe also suggests a herniated disc L4 / 5.
Please also read our topics:
- Herniated disc L4 / 5
and - Symptoms in the legs of a herniated disc
The herniated disc in the lumbar spine can also trigger a so-called cauda equina syndrome, which should be recognized urgently and, if left untreated, can lead to permanent paraplegia. We therefore recommend our website for further information: Cauda equina syndrome - do I have paraplegia?
Symptoms of a herniated disc L5 / S1
A herniated disc L5 / S1 is the most common in the human body. Basically, the L5 or S1 nerve root can be affected.
If the lowering of the foot is disturbed, an affected area between S1 is to be assumed. Here the intervertebral disc pushes through between L5 and S1 (L5 / S1). If there is a herniated disc L5 / S1, which is attached over several segments, it can also happen that autonomic nerve tracts that affect the sympathetic or parasympathetic nervous system are damaged.
One also speaks of the so-called cauda syndrome.
This syndrome becomes symptomatic when the patient can no longer control their bladder or bowel function (see also: Bladder rectal disorder). In the case of sudden urinary or fecal incontinence, a herniated disc must always be considered as the cause. This is an absolute emergency because the symptoms indicate that the herniated disc is affecting vital nerve tracts.
Even in the worst case, a possible permanent dysfunction of the bladder and stool function must be assumed if there is no immediate therapy of the herniated disc or surgery of a herniated disc of the lumbar spine.
In this extreme case, this consists exclusively of an operative decompression of the affected area on the spine. In this operation, the herniated disc is surgically removed. Conservative therapy is by no means possible here.
Almost all L5 / S1 herniated discs can be treated conservatively.
The herniated disc in the lumbar spine can also trigger a so-called cauda equina syndrome, which should be recognized urgently and, if left untreated, can lead to permanent paraplegia. We therefore recommend our website for further information: Cauda equina syndrome - do I have paraplegia?
Learn more about the .
Symptoms of a herniated disc on the sciatica
Of the Sciatic nerve is the most powerful nerve in our body and is formed from parts of the nerve roots L4 to S3.
Due to its position and course, the nerve itself has good soft tissue coverage, which guarantees it relatively good protection against injuries.
Nevertheless, problems can arise if, for example, a Thigh fracture or a compression when passing through the Piriformis muscle in the pool present. In addition, an intramuscular syringe can injure the sciatic nerve if administered incorrectly.
A herniated disc in the lumbar spine can also trigger nerve irritation and typical symptoms. Nerve irritation even has its own name in medicine Sciatica.
Sciatica describes the nerve root irritation of the sciatic nerve and is therefore one of the Radiculopathies (lat. radix= Root; Root irritation). This leads to pain, paralysis and sensory disturbances. A classic for sciatica is the tearing, pulling pain from the buttocks to the leg. In addition, symptoms of sciatica due to a herniated disc include paresthesia and limitations in exercise capacity. This pain can be aggravated by coughing and sneezing as well as pressing the abdomen. If there is a serious lesion of the sciatic nerve, it can even lead to incontinence and Erectile dysfunction come.
Since the sciatic nerve is formed from the L4-S3 nerve roots, the symptoms correspond to those of the general herniated discs of the lumbar spine.
A Sciatica irritation can occur in both a herniated disc L4 / 5 and a herniated disc L5 / S1.
The symptoms usually get better when lying down!
Lying in bed on a softer surface causes moderate to severe discomfort in many cases, while lying on flat and firm surfaces is considered to be pain-relieving.
So-called step positioning often helps to alleviate the symptoms. A step position can be achieved by placing the lower legs on a raised cube so that a 90 ° angle is achieved in the hip and knee joint.
What else you can do against the symptoms of a herniated disc can be found at: Treatment of a herniated disc
Symptoms of a herniated disc of the thoracic spine
A herniated disc the Thoracic spine occurs the least in comparison to the cervical and lumbar spine. One of the reasons for this is that the spine is less mobile in the area of 12 thoracic vertebrae. A herniated thoracic disc is also called "thoracic disc prolapse" designated.
In principle, the same symptoms can occur as with a cervical disc herniation:
- Pain
- Paresthesia (tingling and numbness)
and in the worst case - Paralysis.
A herniated disc of the thoracic spine is often completely symptom-free and is only an incidental finding on CT or MRI examination of the thoracic spine if lumbago is suspected. In some cases, the thoracic spinal disc herniation remains undetected and symptom-free because the patient has good back muscles that have a compensatory influence. Otherwise, the classic leading symptom is pain, which is oppressive or dull.
You can usually feel it in the middle of your back, but it can also radiate. This is a peculiarity of the thoracic vertebrae, because they are articulated with the head of the ribs (lat. Capita costae).
The pain may therefore be belt-shaped along the Rib courses radiate to the front of the abdomen, for example if the Vertebral joints are blocked by a herniated disc of the thoracic spine. In the deep inhalation phase, when the ribs straighten horizontally, some patients describe the feeling of not being able to breathe deeply. Understandably, such pain can often be movement and breathing dependent. In addition, there is pressure pain in the corresponding segment and individual muscle groups can harden with accompanying muscle pain.
The pain can radiate in a belt-shaped manner, but the characteristic of the radiation in a herniated disc of the thoracic spine is less common than in the cervical and lumbar spine. The pain can be to cough or sneezing because it causes a slight jarring and increases the irritation of the broken disc to a nerve. In addition to pain, patients complain of restricted mobility, muscle tension and reduced strength.
Another symptomatic peculiarity of the thoracic disc herniation is the fact that there are problems with the Heart, how Racing heart or Palpitations, Dizziness and Shortness of breath can come. The symptoms are in part similar to those of one Angina attack, because some patients also describe chest tightness. If these symptoms and signs of paralysis occur, a doctor should be consulted immediately, as this is no longer a minor prolapse.
In general, as with any herniated disc, the severity of the prolapse plays a decisive role; it is decisive for the pain intensity.
- Symptoms of a herniated disc of the thoracic spine
- Herniated disc of the thoracic spine
- Stumbling heart through back (pain)
Abdominal pain with a herniated disc in the thoracic spine area
When it comes to abdominal pain, very few people think that the cause can be a herniated disc in the thoracic area. This is however No rarity. Due to the herniated disc Spinal nerves compressed. this leads to belt-like discomfort in the area of the ESPE. The pain that occurs as a result of compression of the spinal nerve roots in the thoracic spine area can also radiate into the abdomen. The pain character is usually stabbing or pulling radiating from the back. Often times, movement of the back or trunk increases the intensity of the pain. But forced coughing or sneezing can also increase the pain by manipulating the irritated spinal nerves. It is therefore important to consider a herniated disc in the thoracic spine after all organic causes of abdominal pain have been clarified.
Read more on the topic stomach pain
Signs independent of herniated disc
Pain caused by one disc prolapse going out can also have a significant impact on general well-being and be indirect signs of a herniated disc.
This can also be the case with severe pain
- nausea
- general malaise
- listlessness
- up to depressive symptoms
come.
Patients with chronic back pain will usually adopt postures that are gentle on the back and therefore cause less pain.
Also read our topic for more signs: Signs of a herniated disc

Unphysiological postures on the one hand and lack of exercise on the other will alleviate the symptoms, but on the other hand lead to incorrect stress and bad posture.
In some cases, slipped discs can go completely unnoticed (without symptoms), i.e. they do not cause typical symptoms.
This is the case in almost all initial stages, when the herniated disc begins to develop.
In the somewhat rarer acute herniated discs, in which the disc suddenly protrudes into the vertebral canal (spinal canal), acute symptoms almost always occur.
Most herniated discs start insidiously and are chronic.
So it can be months or years before symptoms arise for the first time before they cause symptoms.
Patients who have developed a herniated disc and strain themselves with one-sided movements or postures experience symptoms much earlier than people who move gently and in a balanced way.
The following topic may also be of interest to you: Is there a herniated disc without pain?
Neurological symptoms of a herniated disc
In advanced and severe herniated discs, back pain also occurs neurological symptoms revealed. These include, on the one hand, discomfort, often in the form of tingle or Numbness expressed by the patient.
Depending on which vertebra is affected and which intervertebral disc slips out between the adjacent vertebral bodies, these so-called tingling paresthesias can occur on the arms, fingers or legs.
At first, the patients complain of a "strange" feeling, which is compared to the feeling of "touching cotton wool". Sometimes there is a tingling sensation in the aforementioned areas, which in turn makes the patient restless. In some cases the feeling of "Falling asleep“An extremity, over a long period of time. Sometimes there are reports of "ant running" on the skin.
The pain is often provocable. While sitting (especially when bending forward) or when standing for a long time, the symptoms are usually described as more severe.
In addition to pain you can often also Numbness or Tingling sensation in herniated discs become symptomatic.
- Is tingling a sign of a herniated disc?
and - Is numbness an indication of a herniated disc?
In pronounced and severe cases of Herniated discs neurological motor symptoms are also added, i.e. certain parts of the body can no longer be moved in the usual way. What is very stressful for the patient is an important one for the doctor Diagnostic criterion.
Tingling sensation as a symptom of a herniated disc
The tingling sensation falls under the medical category of paresthesia and is a type of sensitivity and sensation disorder.
In addition to the tingling sensation, the term paresthesia describes other unpleasant body sensations such as numbness and temperature perception disorders without an associated adequate stimulus.
The pathophysiology behind the paresthesia lies in different mechanisms. On the one hand, the tingling sensation can be caused by damage to sensitive pathways, but on the other hand, it can also be caused by injuries to the endings of the sensitive nerve fibers. These are unmyelinated and therefore more vulnerable, and react to the damage with a spontaneous discharge. The tingling sensation is caused by excessive nerve activity without an adequate stimulus. In the case of a herniated disc, the first-mentioned mechanism applies. In addition to nerve damage, the tingling sensation can also be caused by reduced perfusion (circulatory disorder).
Patients who experience a tingling sensation due to a herniated disc describe this as an uncomfortable, sometimes even painful feeling on the surface of the skin. Often the feeling of "Ants run“Written on the skin. The pain can be stabbing, pulling and burning as well as tingling or electrifying.
Patients often report numbness in a corresponding region in connection with the tingling sensation.
Please also read our relevant topic: Tingling - Signs of a Herniated Disc?
Please also read our relevant topic: Leg tingles - what's behind it?