Lipedema - How Can I Tell It?
introduction
Lipedema is often very stressful for those affected.
They are characterized by a fat distribution disorder, which is particularly noticeable on the legs. Without a change in diet or a change in activity level, large amounts of fat accumulate on the legs. The disease affects almost exclusively women and usually occurs during the menopause, less often during puberty. For this reason, one suspects a connection between the development of the disease and the hormonal balance.
You might also be interested in: Connective tissue weakness

definition
Lipedema is a progressive disease that is characterized by an atypical, symmetrical accumulation of fatty tissue on the sides of the hips and thighs. The subcutaneous fat increases slowly but steadily. The pathological fat distribution can be different, so that sometimes the entire leg is affected. Then one speaks of the so-called "pillar leg", or the upper part of the thigh, the so-called "breeches". There are different stages of the disease. In later stages, bulges of fat may even form above the knees or ankles. Depending on how far the lipedema has progressed, the proportions of the upper and lower body no longer fit. This is particularly noticeable in people of normal weight with lipedema in the later stage.
How do I recognize lipedema?
Lipedema can often be recognized or at least guessed at at a glance. Particularly noticeable are the thick legs, which become significantly thicker due to a maldistribution of the fatty tissue. In lipedema, the volume is unevenly distributed between the upper and lower body. Affected people often have the feeling of very heavy legs. You can recognize lipedema mainly by the localization, they are mainly on the thighs and lower legs. The formation of fat on the inner thighs can lead to disturbances in the gait pattern and the legs can rub painfully against each other.
What you might also be interested in in this regard: Heavy Legs - What Can I Do?
Many bruises can usually be seen on the skin, as lipedema is associated with a tendency to hematomas (bruises).
In addition, the legs are often sensitive to pressure and pain. In warm weather, after long periods of sitting or standing, and in the evening, the edema causes a feeling of tension and pain. Those affected describe the pain mainly as dull, pressing and heavy, with the symptoms mostly getting worse over the course of the day. Lipedema is characterized by worsening when warm, standing or sitting for long periods of time. It is characteristic of the disease that the symptoms always appear symmetrically. A single leg or arm is never affected.
The symptoms usually begin in the legs and can only be detected in the arms in later stages of the disease. Orange peel is also typical of lipedema. Due to fat and water retention, small nodules form in the subcutaneous fatty tissue, which means that dents that resemble the surface of an orange can be seen. However, lipedema is only present if the hands and feet are not affected.
Read more on the topic: Swollen legs
Stage 1 of lipedema
In stage 1 of lipedema there is already a visible tendency towards the typical “breeches” shape. The skin is smooth and even, but shows an “orange peel” texture when pushed together (pinch test). At this stage, the subcutaneous tissue already feels thickened and soft, and structures that feel like styrofoam balls in a plastic bag can sometimes be felt, especially on the inside of the thighs and above the knees.
Stage 2 of lipedema
In the second stage there is a pronounced “breeches” shape and the skin already has a coarse-knotted surface with large dents and walnut to apple-sized knots (“mattress skin”). In stage 2, the subcutaneous tissue is thickened but still soft.
Stage 3 of lipedema
The third stage of lipedema is characterized by a pronounced increase in circumference and strongly thickened and hardened subcutaneous tissue. Those affected suffer from coarse, deformed flaps of fat on the inner thighs and knee joints, sometimes bulges of fat hang over the knees and ankles. Often the result is a knock knees position and abrasions on the knees.
What types of lipedema are there?
There are different types of lipedema that describe the different distribution patterns of the abnormally increased fatty tissue. On the legs there is the thigh type with the so-called "breeches". Here only the hips and thighs are affected by lipedema. In the case of the lower leg type, the lower legs are also affected, the shape is often described as the “waistband” type. There is also the ankle type ("bloomers", "Turkish pants", "suave pants"). The lower legs down to the ankles are also affected here. There you can see a clearly visible step that hangs down like a fat collar over the ankle. If the arms are also affected, which is often the case, the fat distribution here usually corresponds to the pattern of the legs.
Which doctor can confirm the suspected diagnosis?
Doctors who deal with blood vessels are primarily responsible for diagnosing lipedema.
Angiologists primarily deal with arteries and veins. So both types of blood vessels. The arteries lead the blood away from the heart, veins lead it back to the heart. These doctors are mostly involved in the treatment of circulatory diseases.
Another group of doctors are the phlebologists. They specialize in veins.
Lymphologists can also confirm the suspected diagnosis of lipedema. They deal with the lymphatic vessels. Veins only return about 90% of the fluid to the heart that arteries carry to all tissues. The remaining 10% get back into the circulatory system via lymph vessels.
Which doctors treat lipedema?
The first point of contact if you suspect lipedema should be your family doctor. The family doctor is familiar with the previous course of the disease, the way of life and the medication. If necessary, the family doctor can refer the person concerned to experts. There are dermatologists with the additional designation “phlebologist”, vein medicine. They can be the right person to contact if you have any complaints. If you would like to have a medical liposuction performed after successful drainage of the lipedema, a surgeon can be consulted. The family doctor can recommend appropriate colleagues and issue a referral for a consultation.
What diagnostic measures are there?
Normally, an inspection (looking) of the affected person's legs is sufficient to diagnose lipedema.
Here you can see the thick legs, which often have orange peel with many dents. The increased tendency to bruise can usually be seen at a glance. It is also possible to feel small "balls" under the skin. These are initially very small, but can grow to the size of a walnut. They consist of adipose tissue and stored fluid. In contrast to other edema, lipedema does not leave a dent after the skin has been dented. However, the thighs are particularly sensitive to pressure and pain.
One test that can be performed is the test for Stemmer's sign. This is negative in the presence of lipedema, which means that the skin over the fingers and toes can be lifted.
The structural changes under the skin can also be determined using ultrasound. Therefore, an ultrasound is often used for the final diagnosis.
Causes of Lipedema
The causes for the development of lipedema are not yet fully understood. Lipedema almost exclusively affects girls and women, which is why experts suspect hormonal causes. Lipedema can occur spontaneously or from one over time Lipohypertrophy arise, an increase in subcutaneous fatty tissue. It is likely that there is a hereditary component as approximately 20% of those affected have other cases within the family.With lipedema, there is an increased accumulation of fatty tissue in the subcutaneous tissue, but the process is different than with "normal" weight gain. This means that in lipedema no individual fat cells grow, but rather the fat tissue itself changes: the number of fat cells increases, so that the fat tissue of the subcutaneous tissue becomes thicker. It will also be structured more and more firmly. As a result, the fat cells form palpable nodules in the subcutaneous tissue.
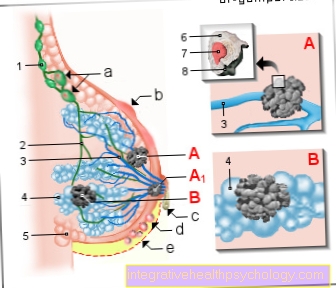
In addition, lipedema leads to a Microangiopathy, a disease of the smallest blood vessels (Capillaries). That leads to the permeability of the tiny Capillaries increases. At the same time, there is increased filtration in the vessels, which means that more water from the blood reaches the surrounding tissue through the vessel walls. This leads to the development of an edema above the connective tissue covering layer (Fascia). This water build-up can cause tenderness and pain on pressure.
Over time and the progression of the disease, the lymph vessels are stressed and the lymphatic drainage is disturbed, so that lymphedema can develop as a result of lipedema.
Is lipedema hereditary?
The reason for the development of lipedema is not fully understood. The tendency to develop lipedema is presumably hereditary. In about 20% of those affected there are further cases within the family.
Lipedema and thyroid disease - is there a connection?
There are comorbidities that are frequently diagnosed in people with lipedema. These include diseases of the thyroid gland such as overactive, underactive or Hashimoto's thyroiditis. In the Hashimoto's thyroiditis is an autoimmune disease that leads to chronic inflammation of the thyroid gland. In the long term, an underactive thyroid develops in the course of the disease. However, since the exact cause of the development of lipedema is not yet known, no scientific connection between the occurrence of lipedema and malfunctioning of the thyroid gland can be demonstrated. Nevertheless, many patients with lipedema report an accompanying hypofunction of the thyroid gland or Hashimoto's thyroiditis, in which hypofunction also occurs.
What accompanying symptoms suggest lipedema?
Above all, lipedema is characterized by thick legs. For no apparent reason (change in diet, less exercise), the legs suddenly become thicker and store fat. They are also sensitive to pain and pressure, in later stages the areas can even hurt without touching them. Some people describe a feeling of heat in the legs (or arms), even if the limbs feel cool on the outside. In warm weather, standing and sitting for long periods of time, or in the evening, the symptoms may worsen and a noticeable feeling of heaviness may appear in the legs.
Dents in the skin are also possible symptoms of lipedema. In addition, bruises and spider veins are common. Usually only the legs are affected at first, later the arms are added, so that prolonged work overhead (blow drying or brushing) often leads to discomfort. The arms are affected in 30-60% of lipedema patients. The symptoms of the legs are usually more symptomatic, so that the arms are often out of view.
You might also be interested in: Strengthen connective tissue
Pain and tenderness
Particularly in warm weather or after standing for a long time, symptoms such as pain and tenderness in the leg area are particularly pronounced in people with lipedema.
In such situations, in addition to the fat deposits on the legs, there is also a reduced transport of fluids from the legs back to the heart.
This leaves more fluid in the tissue, which leads to additional edema. These can trigger a feeling of tension, which is also associated with pain and tenderness. The pain is usually dull and pressing.
Increased tendency to bruise in lipedema
People who suffer from lipedema are extremely likely to get bruises. These are usually caused by the slightest bumps, and often the people affected cannot even remember having bumped at the given spot.
Nevertheless, the pain sensitivity at the location of the bruises is particularly high. Unfortunately, the exact cause of the increased tendency to bruise is not known. However, it could be assumed that this is due, among other things, to the fact that the blood accumulates in the veins and is more difficult to evacuate. The veins are often filled with blood and burst with light pressure.
Swollen, heavy legs with lipedema
The swollen and heavy legs gradually come to light in the presence of lipedema. First of all, more and more fatty tissue accumulates on the legs. This is particularly the case in the thighs, but the lower legs are also quickly affected.
How exactly this fat distribution disorder occurs is not yet known. A connection with hormonal control cycles is suspected. In the advanced stage of lipedema, congestion in the vascular system also occurs. Both the transport of the blood via the veins and the transport of the remaining fluid via the lymphatic system can be disturbed. As a result, there is increased fluid retention, which in turn causes the legs to swell more and cause a further feeling of heaviness.
Occurrence of spider veins in lipedema
Spider veins are a result of overloading the venous vascular system. Veins carry blood from the circulation back to the heart. This transport must take place against gravity, especially on the legs.
In diseases such as lipedema, the necessary transport mechanisms can be disrupted. This causes the blood to build up in the veins.
The once very thin and fine vessels on the skin are increasingly being filled with blood. These vessels lose their elasticity, so to a certain extent they wear out. These dilated veins appear as bluish, tortuous vessels on the surface of the skin.
You might also be interested in: Spider veins
Impression of knock knees associated with lipedema
The misdistribution of tissue and fat mass leads to disturbances of the gait pattern in the course of lipedema. Typically, a person with knock knees has a displacement of the leg axis. Normally, the hip joint, knee and ankle should be on the same axis.
If you have knock knees, the knee is further inside. If one talks about knock knees in connection with lipedema, it does not necessarily have to be such a leg axis shift. Often the impression of knock knees results from the deposition of fat flaps on the inside of the thighs. Only when a lot of tissue has accumulated on the thigh can incorrect loads and a change in the leg axis occur.
Cellulite (orange peel)

Cellulite occurs almost exclusively in women. They usually show up on the thighs and buttocks in the form of dents in the skin.
This is why the symptom is often referred to as orange peel. The changing process takes place in the subcutaneous (directly under the skin) fatty tissue and is characterized by fat accumulation and water retention.
The exact mechanism of its formation is not yet known. However, a connection with hormonal changes is suspected. This theory would explain why menopausal women are mostly affected. The symptoms also occur less frequently in girls during puberty (hormonal changes also take place during this period).
You might also be interested in: Exercises against cellulite
Tissue injuries (wound eczema) on the inner thighs
When a person suffers from lipedema, tissue mass and volume increase. As a result, tissue bulges can form on the inside of the thighs, which can rub against each other when walking.
This chafing often leads to wounds forming on the inside of the thigh at some point.
The changes in the tissue can also impair wound healing. As a result, the wounds that have formed do not heal properly or at least more slowly and become infected more frequently.
Wrinkles caused by the tissue bulges can also lead to the formation of wound eczema. Sweating, in particular, keeps the skin in the fold warm and moist, which means that wounds develop more quickly. Wound healing disorders often occur there too.
Lipedema in pregnancy
The cause of the lipedema is not clear, but experts suspect a hormonal connection, since almost only women are affected, especially in phases of hormonal change such as puberty, pregnancy or menopause. If lipedema occurs before or during pregnancy, you should make sure that the disease does not progress any further. The treatment looks the same as without pregnancy. That means that you pay attention to a healthy, balanced diet. However, a vegan low-carb diet or ketogenic diet should be avoided during pregnancy in order to provide the baby with the vitamins and nutrients necessary for development.
Regular exercise is good, especially sports like swimming, aqua jogging, or aqua aerobics. You burn fat and relieve the symptoms of lipedema through natural lymphatic drainage and cooling water. Surgical interventions such as liposuction should be avoided during pregnancy. Wearing compression stockings, on the other hand, is always suitable and important.
Treatment of lipedema
So far there is no causal therapy for lipedema. Nevertheless, there are ways to alleviate the symptoms of the disease in a targeted manner and also to reduce the circumference of the legs. Whether therapy is necessary depends on the stage of the disease. As a rule, doctors prescribe therapeutic measures from the second stage. The main purpose of the therapy is to reduce the accumulation of water in the tissue as much as possible, or to decongest the tissue. Methods for this are the complex physical decongestive therapy (KPE), which includes four measures: manual lymphatic drainage (once or twice a week), compression bandages in the sense of bandages or compression stockings (worn daily), physiotherapy and intensive skin care. Compression bandages are a good way to prevent more water from accumulating in the tissue, even in the early stages, or to prevent lipedema from worsening. It is advisable to carry out the complex physical decongestion therapy for life in order to prevent the formation of new edema.
After successful KPE, i.e. targeted dehydration of the lipedema, liposuction (Liposuction) where the doctor removes excess fatty tissue. There are sports that can alleviate the symptoms. Since lipedema reduces blood flow to the skin, it can be more prone to inflammation and scarring. Therefore, targeted skin care with moisturizing lotions is particularly important. You should pay attention to pH skin-neutral soaps and creams. Ingredients such as urea and Dexpanthenol are well suited for treating the skin with lipedema.
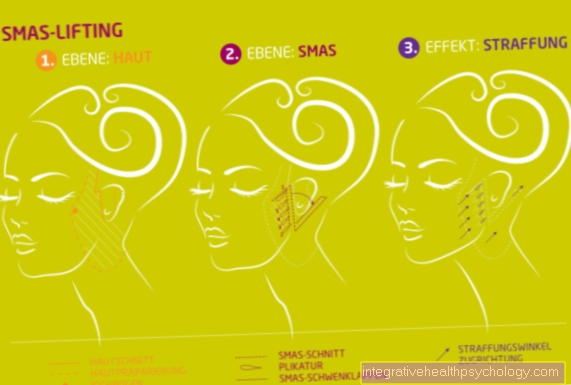
Does surgery help with lipedema?
Surgery / liposuction may be an option after successful complex physical decongestion therapy (CPE) after the lipedema has been successfully drained. For liposuction (Liposuction) the surgeon surgically removes fat tissue from certain areas of the body. Up to 70% of the fatty tissue can be suctioned off in the corresponding area. In the case of lipedema, the focus is on painful fat tissue proliferation with increased sensitivity to touch. Suctioning fatty tissue with gentle techniques can help with lipedema after targeted drainage. However, liposuction never removes all of the fatty tissue. Dents may form in the skin after the procedure. Special compression clothing helps against this.
Can you cure lipedema?
Unfortunately, lipedema is an incurable disease that is progressive. Since the cause has not been clarified, there is currently no causal therapy. What can be done, however, is to slow the progression of the disease. There are different stages of lipedema and without treatment the lipedema will usually get worse and the symptoms worse.
If you are affected and suffer from lipedema, you should start early with a targeted therapy in order to reduce the water stored in the tissue as much as possible. Complex physical compression therapy (KPE) includes manual lymphatic drainage, compression bandages, physiotherapy and intensive skin care. In the case of lipedema, this therapy should be carried out for as long as possible so that the edema does not re-form. A healthy diet, normal weight and exercise are also recommended.
Homeopathy for lipedema
There are people with lipedema who report the beneficial effects of Schuessler salts. In the morning "Biochemie No. 10" (5 tablets), at noon "Biochemie No. 5" (5 tablets) and in the evening again "Biochemie No. 10" (5 tablets) corresponds to a metabolism-stimulating treatment with Schuessler salts. It is also said to help rub jojoba oil on the legs twice a day. This should lead to water being washed out. A balanced diet and plenty of exercise are important components of homeopathic therapy for lipedema.
Diet in case of lipedema - what should be considered?
Lipedema is not a “reserve fat” that arises from improper diet and obesity. Lipedema is a fat distribution disorder that occurs symmetrically, particularly on the legs. A healthy diet and exercise are particularly helpful in the preliminary stages of lipedema in order to have a positive influence on the progression of the disease. Since lipedema does not develop like usual fat deposits, it cannot be combated with a radical weight loss cure. Nevertheless, weight loss in combination with exercise and compression stockings works against the aggravation. You should therefore try to set your own body weight to a Body Mass Index (BMI) between 19 and 25 and avoid weight gain.
Many sufferers report improvements in lipedema symptoms with a vegan low-carb diet or a ketogenic diet. It is assumed that the fat cells in the affected parts of the body no longer function properly, due to blockages, inflammation or deficiency symptoms, and therefore receive too little energy. Accordingly, when dieting with lipedema, one should make sure that enough enzymes, numerous vitamins, minerals and trace elements are consumed.
The diet should be anti-inflammatory, easy to digest, low in carbohydrates, and natural. This also protects the digestive organs so that the intestinal flora can regenerate. This increases the absorption capacity of the intestinal mucosa and important nutrients can be better absorbed. Green, edible plants such as algae, wild herbs (dandelion, nettle), green leaf salads and cabbage vegetables and culinary herbs are valuable for the organism and are anti-inflammatory. You should eat plenty of fruits, berries, mushrooms, legumes, sprouts, nuts and seeds. Healthy fats have a good ratio of omega 3 and omega 6 fatty acids; flaxseed oil, virgin olive oil and coconut oil are optimal. A healthy diet cannot cure lipedema, but it can have a positive effect on the symptoms and the progression of the disease.
Also read our article about Diet for lipedema!
Which sports help with lipedema?
Sports that take place in water are particularly suitable for those with lipedema, as the water pressure acts on the tissue like a kind of natural lymphatic drainage. Sports such as swimming, aqua jogging, aqua aerobics and aqua cycling are recommended. The coolness of the water can alleviate the pain, especially when it is warm, when the symptoms are often worse.
One should avoid long periods of standing and sitting. In principle, you should avoid being overweight with lipedema and maintain your ideal weight. Any sport, especially endurance sport, is welcome to reduce excess weight. Swimming is ideal for lipedema. Targeted leg exercises are also well suited, on fitness equipment or on a mat at home.Regular fascia training is recommended, especially with advanced lipedema. At best, you should do ten minutes of exercises with a fascia roller every three days to loosen the adhesions in the connective tissue. Overall, you should do the sport that is good for you and try to maintain your weight.
Fascia training for lipedema
Particularly with painful lipedema, small bumps or injuries cause bleeding quickly. At an advanced stage, the skin is poorly supplied with blood and is cool. Fasciae are connective tissue structures that form sheaths around all structures such as bones, muscles and organs. The lymphatic channels are also surrounded by fascia, so that the lymph flow depends on the condition of the connective tissue. If the lymph jams, the fasciae stick together. It can happen with lipedema. Therefore, facial training is useful to loosen the adhesions and to promote blood circulation. Fascia training with a fascia roller should be done regularly to keep the effect. The cells are manipulated by rolling on the fascia roller in such a way that they then fill up again with cell fluid. Ten minutes of training every three days is ideal for lipedema.
Can you go to the sauna with lipedema?
Basically you should avoid the sauna, hot sun baths and extreme heat with lipedema. The heat often makes the symptoms worse. If you don't want to do without it, you should at least shower the tissue with cold after a hot bath or sauna so that the vessels contract again. Alternating showers are particularly recommended.
Read more on the topic: Alternating showers