Gastric bypass surgery - you should consider this!
introduction
Gastric bypass is the most common operation in the context of bariatric surgery (= surgery for overweight). As the name suggests, the aim of this operation is to support weight loss in severely overweight patients with the help of a “stomach reduction”. However, this surgical procedure is not considered to be the method of choice, but is more likely to be used when all other attempts to lose weight have not been successful.

How does gastric bypass work?
In gastric bypass surgery, most of the stomach is "paralyzed" by guiding the chyme from the stomach entrance directly into the small intestine. This means that a small part of the stomach remains and the digestive juices of the stomach are not lost. The smaller remaining stomach has a volume of up to 50ml and, with this smaller volume, represents a kind of "food brake".
Preliminary examinations
The operation to produce a gastric bypass is particularly suitable for overweight patients who either have a BMI of> 40 (obesity grade 3) or a lower BMI, but also show other diseases such as diabetes mellitus, sleep apnea or heart disease.
As a rule, gastric bypass surgery is only used if conservative measures (nutritional advice and changes, physical exercise, etc.) have previously been tried over a certain period of time and have been unsuccessful. In some cases, e.g. However, if the BMI is> 50, gastric bypass surgery can be performed directly without prior conservative attempts at therapy.
Before an operation, therefore, the suitability of the operation is checked as part of a detailed physical examination and by means of a detailed anamnesis. The stomach is briefly checked for pathological changes such as tumors, ulcers or inflammation using a gastroscopy. An ultrasound examination of the (upper) abdomen is also carried out with special attention to gallbladder problems such as Gallstones that can be removed as part of the operation.
Both examinations are necessary because the changed anatomy after the operation means that the original stomach can no longer be mirrored and gallstones can no longer be removed.
How does the operation work?
Gastric bypass surgery is performed under general anesthesia, which means that the patient is unconscious for about 90-150 minutes while being intubated and ventilated. The operation itself is carried out almost exclusively using the keyhole technique (minimally invasive surgery / laparoscopy), less often via a larger incision (open surgery).
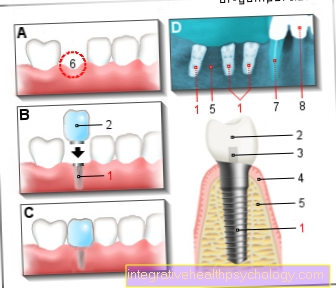
The surgical instruments and a camera are inserted into the abdominal cavity through several small skin incisions after the abdominal cavity has been filled or "inflated" with a gas (CO2) so that the abdominal wall is lifted and the surgeon has a better view of the organs. After finding the stomach, it is cut off with a row of staples just below the stomach entrance. Below the end of the esophagus there is a small residual stomach (Stomach pouch), which usually has a capacity of less than 50ml. The remaining, closed stomach remains in place and is, so to speak, "shut down".
Next, the small intestine in the area of the jejunum (Jejunum) severed: The lower end of the incision is then "pulled up" and connected to the small remaining stomach (Gastrojejunal anastomosis). The upper end of the cut of the severed jejunum is now connected to the section of the small intestine that follows the jejunum.
Overall, the following functional picture emerges: The ingested food reaches the small remaining stomach via the esophagus and from there without contact with the duodenum directly into the small intestine and later into the large intestine. All digestive secretions from the stomach and duodenum (bile / pancreatic juice) are passed directly into the small intestine and fed there to the food to be digested.
Another name for gastric bypass surgery is Roux-en-Y gastric bypass.
Find out more at: Roux-en-Y gastric bypass
Aftercare
Immediately after the operation, a slow, gentle diet and physical mobilization follow during the hospital stay. The advantages of the keyhole technique quickly become apparent, as the small cuts make it possible to reduce pain and "get back on your feet" more quickly. The sutures or staples of the closed small skin incisions can usually be pulled between the 10th and 14th day after the operation.
Due to the lower stomach volume, large meals can no longer be consumed, so that particular care must be taken to eat several small, protein-rich portions throughout the day and to consciously chew the food well. You should avoid very long-fiber meat or vegetables, as well as foods and drinks with a high sugar content.
Since vitamins and nutrients can no longer be absorbed so well as a result of stomach reduction, it is also necessary to take food supplements for life so that deficiency symptoms do not occur. In order to recognize and treat these in good time, regular blood tests by the family doctor are necessary.
Medicines can also differ in their effect due to the changed gastrointestinal passage time: it may be necessary to adjust the dose of the medication to be taken, which must be discussed individually with the attending physician.
Risks of gastric bypass surgery
In principle, the usual risks associated with an operation also apply to gastric bypass surgery: injury to neighboring structures such as nerves, vessels or other organs, wound healing disorders and wound infection and the risks of anesthesia.
Since gastric bypass surgery is an intervention on the gastrointestinal tract and the anatomy is changed by means of newly created intestinal connections, there is always the risk that one of the new gastrointestinal connections is not tight (Anastomotic leakage), which in the worst case leads to postoperative peritonitis (Peritonitis) can lead. Furthermore, any intervention on the gastrointestinal tract can in retrospect lead to a temporary paralysis of the intestine. This can lead to digestive problems and even constipation that may need treatment.
A dreaded risk is the so-called dumping syndrome: Because only a small residual stomach with a relatively small filling volume is left, the functional collecting reservoir for food is also omitted, so that the food "falls down" from the esophagus into the small intestine. without lingering in the stomach and being digested beforehand. On the one hand, this can lead to diarrhea and circulatory problems shortly after eating, and on the other hand, the body is relatively flooded with sugar, so that more insulin is released and subsequently hypoglycaemia can easily occur.
Read on under: Risks of gastric bypass
Duration of the operation
It is difficult to predict how long gastric bypass surgery will take, as it always depends on many factors. On the one hand, the duration depends on the selected surgical method, i.e. whether the operation is minimally invasive or open over a larger abdominal incision.
On the other hand, the duration also depends on the individual anatomy of the patient and on intraoperative difficulties and complications. In some cases it can happen that gastric bypass surgery is started laparoscopically, but cannot be completed without complications, so that a switch to the open surgical procedure is necessary. Here, too, the operating time is changed or extended accordingly.
On average, however, an operation time of 90-150 minutes can be expected.
Hospitalization
Precise information about the length of the hospital stay cannot be made across the board either, as this also depends on a number of factors. On average, however, a 4-6 day hospital stay should be expected.
As a rule, patients are admitted to the ward the day before the operation and prepared for the operation. After the procedure has been carried out successfully, there will be an inpatient stay of 3-5 days, during which the diet and physical mobilization take place. However, the postoperative length of stay can also vary individually, depending on how quickly the recovery occurs and whether there are postoperative complications.
Sick leave
The length of sick leave after the operation also varies from person to person and depends largely on the type of occupation of the respective patient. In addition, how complex the operation was, intra- and post-operative complications and individual recovery times.
On average, a sick leave of 2-5 weeks can be expected. After this time, a full physical capacity can be assumed again, so that one can speak of a complete healing.
When can I smoke again?
It should be no secret that smoking is inherently bad for your health. But nicotine consumption has a negative effect on wound healing in particular. You should refrain from smoking one to two days before the operation, as this has a positive effect on the safe performance of general anesthesia. After the operation, smoking should be avoided, if possible, until the wounds have healed (internal and external skin wounds).
When can you drink alcohol again?
It is usually possible and advisable to drink fluids very quickly after the operation, but not to consume alcohol. Drinking alcoholic beverages should actually be completely avoided after gastric bypass surgery, as their effect changes significantly due to the changed gastrointestinal passage time: By bypassing the stomach and quickly forwarding food and liquids into the small intestine, its mucous membrane comes into contact with a lot of alcohol more quickly. The alcohol is therefore absorbed more quickly, the "flooding" of the alcoholic effect happens more quickly and unfiltered, the liver is also increasingly challenged and the risk of developing liver cirrhosis is greater over time.
However, there is no absolute ban on alcohol.
Post-op nutrition
After gastric bypass surgery, a change in diet is necessary, which should take place in phases.
- During the hospital stay after the operation, the diet is gradually built up again, starting with fluid intake (tea, water, soups) and then yoghurt products.
- Solid foods are still to be avoided in the second to fourth week after the operation; here, too, the diet is restricted to liquid and pulpy foods (e.g. pureed foods).
It is important to ensure that the diet is as low in fat and sugar as possible, and drinks containing carbohydrates and carbonated acid should also be avoided.
- From the fourth week onwards, you can gradually start eating solid foods, which should primarily contain protein-rich, low-fiber products (e.g. chicken, fish).
- Smaller meals should be consumed, as the capacity of the smaller stomach is significantly lower.
- The simultaneous consumption of liquids and solid food must also be avoided, as well as products with a high sugar content, as all of this can cause the food to pass too quickly in the gastrointestinal tract and thus cause digestive problems.
- After an individually long period of getting used to solid food, the lifelong change in diet is similar: small meals, at least 3 per day, balanced mixed food, rich in protein and low in fat, sugar and fiber, drinks without sugar and carbon dioxide, avoid alcohol.
- Due to the changed gastrointestinal passage of food, vitamins and nutrients can also be changed or absorbed worse, so that a lifelong intake of food supplements is usually necessary in order to avoid deficiency symptoms.
Learn more at: Post-gastric bypass nutrition
How much does gastric bypass surgery cost?
It is difficult to give an exact cost estimate for gastric bypass surgery because the costs vary considerably in different clinics. On average, however, one speaks of amounts between € 6,500 and € 15,000.
It is important to know that it is still not a standard benefit in the statutory health insurance funds, but gastric bypass operations are only approved on application and only under the strictest examination and prerequisites and thus also accepted. Otherwise, you will have to bear the costs yourself, so it is highly recommended that you find out about the necessary requirements in detail before applying.
When does the health insurance cover the costs of the surgery?
The cost of gastric bypass surgery is covered by the patient's health insurance company. However, since this is not a regular assumption, an application for assumption of costs must be submitted to the health insurance company in advance.
For this it must be clarified whether on the one hand certain conditions exist, e.g. :
- BMI> 40
- Age between 18 and 65 years
- at least. 2 unsuccessful diet attempts
- Exclusion of addictions / mental disorders / pregnancy / severe metabolic diseases
- Willingness for permanent changes in diet and lifestyle
The application can be worked out together with the family doctor or with a doctor from the selected obesity center and should then be handed in personally to the relevant health insurer.
Can gastric bypass be reversed?
Yes, every gastric bypass operation can theoretically be "operated back".Since no organs are removed as part of gastric bypass surgery, the artificially created gastrointestinal connection can be loosened again to bypass it and returned to its original proportions.
However, this is a second, risky procedure, so that the risk-benefit ratio must be carefully weighed. Whether this makes sense and when there is a medical indication must be discussed in detail with the treating surgeon.
Recommendations from the editorial team
You might also be interested in:
- Risks of gastric bypass
- Post-gastric bypass nutrition
- Gastroplastics
- Gastric band
- Stomach reduction