Eczema
definition
By definition, eczema is a non-infectious, inflammatory skin disease that only affects the top layer of skin (epidermis) and possibly the top layers of the dermis, which are located directly below the epidermis and are interlocked with it.
Since eczema is not caused by pathogens, it is also not contagious. With a prevalence between 3 and 20%, eczema is the most common skin disease.
It is assumed that almost everyone will develop eczema at least once in their life. In addition, eczema is by far the most common occupational disease.
You can find more information about contagious rashes at: Is my rash contagious?

introduction
The term "eczema“(Also called rash, skin inflammation, itching or incorrectly called dermatitis) is a collective name for a variety of non-infectious, inflammatory diseases that affect the top layer of the skin.
There are many different causes that can lead to eczema and depending on the one they can look quite different. However, a typical course of symptoms is in phases, with the acute phase being characterized by inflamed, itchy and reddened skin.
Reliable therapy options are available for most forms of eczema, but they should also be used as early as possible to avoid complications.
Causes of Eczema
There is a Variety of causes for eczema. In principle, one differentiates between
- endogenous (if the disease is from internal factors triggered) and
- exogenous (when the eczema is through external influences eczema.
In addition, one differentiates between
- acute
- chronic Eczema
and can also classify according to the respective localization (e.g. hand-foot eczema).
Roughly you can get most of eczema in three subgroups classify:
1. Atopic eczema
2. contact eczema and
3. seborrheic eczema
1. "Atopic eczema" is another term for the Atopic dermatitis. This is the classic representative of one endogenous eczema, as the neurodermatitis (atopic dermatitis) by various inherited factors comes about. There is a predisposition here Allergies in general, so atopic eczema often comes with hay fever or asthma occurs.
2. At the Contact eczema one again distinguishes between one
- allergic and
- one toxic Shape.
The allergic contact eczema arises when a Allergy to a substance that comes into contact with the skin. A common example of this is nickelOther options are latex or ingredients in perfumes, creams, hair dyes.
This allergy is one Type 4 allergywhich means she's a Late reaction is.
First, the skin has to be done "sensitized" to the allergen be why it only with repeated contact actually reacts with the substance.
Then you can up it after contact with the causative material Symptoms comes Hours to days pass away. This will make the Identifying the cause is often difficult.
To a toxic contact eczema it happens when the skin is over one long period away Contact with harmful substances, mostly chemicals. This group includes, for example Acids, alkalis, cleaning agents, solvents and detergents.
3. Seborrheic eczema is created by a gincreased production of sebum and an incorrect composition of this substance.
In addition, there are various other causes that can trigger eczema, for example UV radiation, Medication, one Overproduction of sweat Etc.
Of the main risk factor for eczema in general is dry skin. People who wash their skin very often or stay in living rooms with dry air are more likely to develop eczema. With them is namely The protective acid mantle of the skin is disturbed and therefore more susceptible to external influences. Long-term UV radiation can also increase the risk of developing eczema, as this also damages the skin permanently.
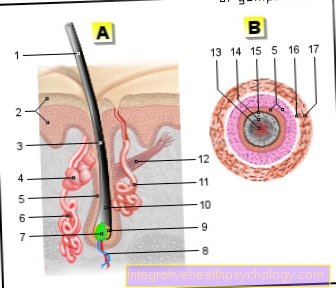
Figure causes of eczema

Facial eczema
(allergic-inflammatory
related skin irritation)
- Reddening of the skin
- swelling
- Blistering
- Pimples
- psoriasis
Causes:
A - contact allergies -
Metallic substances -
Nickel allergy (earrings,
A necklace)
B - types of cosmetics -
Skin creams, powders, lotions
C - stress -
Mental stress,
Neurodermatitis
(Skin disease)
or psoriasis
D - pregnancy -
atopic pregnancy dermatosis
(Neurodermatitis, hay fever,
Bronchial asthma)
E - toddler -
Neurodermatitis
(Skin disease),
Cradle cap (in infancy)
Alternative treatment:
F - aromatherapy -
Oils with intense fragrances
(Lavender, lemon balm, thyme,
Peppermint)
G - chemical substances,
vegetable substances
(Chamomile, sage leaves,
Marigold)
H - bath therapy,
Face wraps, steam baths,
Regions by the sea
with salty air
You can find an overview of all Dr-Gumpert images at: medical illustrations
Symptoms of eczema
Although the eczema is in their Emergence and thereby also in hers characteristic appearance and their localization can be clearly distinguished, they all have in common that they are one phased Take course.
First of all, every eczema is in the acute phase. At this point, the predominates acute inflammatory reaction of the skin. That means that the affected skin area reddened is itchy and often due to Water retention swelling occurs.
Sometimes, in addition to these typical changes, one also finds Scales, blisters, or lumps, some of which also secrete fluid (“wet”). Over time, the vesicles dry out, creating crusts. Dander can also occur now. Especially if the eczema affects the scalp Dandruff occasionally the only symptom.
To a Chronification Eczema happens when it keeps coming back again in the same place occurs or never heals properly. In this chronic stage are eczema then rather by a Thickening and flaking of the skin and a coarsening of the skin structure (Lichenification) marked.
This condition is often found for allergic eczema, which often also Discoloration in the neck or torn ear flaps (owing to dry skin) demonstrate.
Please also read our article on this Rash on the neck
It can also be used in chronic eczema too scratch marks caused by itching and inflammatory lumps appear. At the same time, there may also be areas of skin that are still in the acute stage of eczema.
Depending on Cause of eczema is there certain placesat which it occurs preferentially:
- Atopic eczema is common in the Flexion folds (e.g. in the Elbows or the Back of the knees) or on the Scalp (especially noticeable in babies as "cradle cap").
- Contact eczema occurs where the allergenic substance with the Skin in contact came. As the classic representative of this group nickel and many jewelry items contain nickel, you can often see allergic contact eczema on the Ears, the Wrists or around the neck - just where jewelry is worn. Light induced Eczema is mainly found on areas of skin that are often exposed to the sun.
Diagnosis of eczema
A dermatologist can usually diagnose eczema on the basis of its clinical appearance without an examination as a visual diagnosis put.
Still can further examinations or tests necessary be to the Cause of eczema to find out. If the medical history survey (anamnese) provides an indication of an allergy, an allergy test (depending on the type of allergy a Prick or patch test) help.
Often there multiple triggers or risk factors come together and these are sometimes not directly associated with the eczema by a patient (for example through the Wearing jewelry or taking Medication several days ago), it is often not easy to find out the cause of eczema.
The therapy of eczema

The therapy of eczema depends on the one hand on its stage and on the other hand on its cause. In general, eczema is usually treated externally locally with the help of certain creams or ointments.
The more weeping the eczema, the more water the agent used should contain. On the other hand, ointments containing a lot of fat are used for very dry skin. Ointments that contain some form of the anti-inflammatory cortisone are usually used for an acute flare-up.
Antihistamines, which can also be used in general for allergic eczema, can help against itching. If atopic eczema is present, it can make sense to take additional drugs that have an influence on the immune system and / or have a desensitization carried out.
If topical therapy does not work, most of the drugs mentioned can also be taken in the form of tablets (which makes them systemic). If definite triggers for eczema could be determined, for example nickel, latex or certain medications, then these substances must of course be avoided as consistently as possible.
Read more on the topic: Medicines for skin diseases
Ointments for eczema
Next to the Avoid triggering substances or cosmetics, the treatment of eczema consists of the application of ointments. It is important that the composition of the ointment is adapted to the condition of the skin.
So is with one weeping eczema an ointment with high water content is chosen, whereas in the case of crusts and flakes, a greasy consistency is important for skin care.
The ointments are particularly effective when they are used in the form of compresses. Prescription drugs like Cortisone (a glucocorticoid) are anti-inflammatory and locally immunosuppressive. If the affected, open skin area is still infected with bacteria as a complication, an antibiotic or antiseptic ointment is applied.
Course of eczema
In principle, eczema can be treated well and is therefore usually no further cause for concern. However, this assumes that the cause of the eczema has been correctly identified. If this does not happen, there is a high chance that eczema will become chronic or recurring.
In addition, if the treatment is inadequate, eczema can be a gateway for pathogens and thus secondary to infection (Superinfection). It is therefore important that eczema is treated adequately regardless of the cause in order to avoid consequential damage.
Prophylaxis for eczema
Since it is so many different causes for eczema, there are also various preventive measures, which are then often aimed at avoiding a specific type of eczema. In general, however, you can take care of it dry skin to avoidif you want to prevent eczema:
- do not wash the skin too often
- leave too long in the water
- Humidify room air
- use special, moisturizing care products
- any Avoid skin-irritating substances (or wear gloves)
- avoid excessive solar radiation(especially if you have sun-sensitive eczema!)
When it comes to clothing, make sure that you are too skin-friendly fabrics how Cotton or silk and washes them before wearing them for the first time.
In addition, of course, it goes without saying that if you have ever had eczema was a so-called secondary prophylaxis operates by preventing further attacks. To do this, you absolutely have to triggering substancee.g. nickel, avoid them consistently.
Eczema by location of occurrence
Eczema on the face
Eczema occur in addition to other parts of the body on the face.
In the facial area, eczema occurs mainly on the cheeks or in the area of the nose.
It is to be distinguished acute from chronic Facial eczema.
- The acute eczema on the face is usually triggered by certain substances that cause an allergic skin reaction. Typical of this are the successive occurrence of reddening of the skin, itching and blistering.
- With chronic Eczema on the face on the other hand, the symptoms of reddening of the skin, swelling and blistering occur at the same time, the immune system is activated in a different way.
Potential triggers for eczema on the face are all sorts of foreign chemical and natural substances. Most of the time, the skin of the person concerned has never come into contact with it. On the face, especially cosmetics are like Skin creams, powder or Make up often the cause. In this case, the only thing left to do is to stop using the product immediately if you suspect it.
Because they often use a lot more cosmetics, women suffer from eczema on the face slightly more often. Children are also affected more often than average, whereas older people suffer less from facial eczema, which is related to the reduced activity of their immune system.
In addition to stopping the triggering product, further treatment may be necessary depending on the severity. In the acute stage with redness and severe itching come mainly ointments containing cortisone for use. However, the correct dosage and duration of use are particularly important in the face. In later stages with oozing blisters, moist pads made from moisturizing lotions or soothing ingredients such as chamomile or black tea should be used.
Eczema in the ear
Eczema can also occur in the ear.
Both the outer ear canal, as well as that Inside or outside of the auricle to be affected.
The symptoms are the typical ones that occur in other parts of the body with eczema. Which includes itch, one Redness and swelling and Blistering. A distinction is made between weeping eczema and dry, and acute eczema from chronic.
If the eczema occurs on the earlobe or the pierced auricle, one can Nickel allergy be the trigger. In this case, it is advisable to remove the plug immediately and switch to nickel-free jewelry.
If, on the other hand, the eczema is further inside or extends into the ear canal, it is advisable to consult a specialist in ear, nose and throat medicine.
Eczema on the eyelid
Eczema on the eye, especially on the eyelid (Eyelid eczema), occur less often than on other parts of the body, but are not uncommon.
The causes of a Eyelid eczema are diverse.
A distinction is made between a chronic and an acute form of eyelid eczema. Dehydration eczema, which is characterized by regular lines in the epidermis, can be distinguished from this.
It is more common in the elderly and is caused by skin dehydration. Acute eyelid eczema is often triggered by contact allergies, but non-allergic, predisposed skin diseases can also be the cause. Since the Skin around the eye around the thinnest skin of our body, some substances can only trigger eczema at this point if there is only a slight tendency towards allergies, even if other parts of the body have much more contact with the corresponding substance.
By involuntary eye rubbing, theoretically all substances with which our hands come into contact come into question. Most often, however, it is cosmetics, personal hygiene- and cleaning supplieswhich are well tolerated on the rest of the body skin, but can trigger eczema on the lid. Contact lenses or contact lens fluid can also trigger such eczema.
For treatment, the triggering substance should of course be avoided if known. We also recommend the use of cosmetic products and ointments that are labeled as non-allergenic and unscented. The application of cortisol to the eye is critical to rate. If it cannot be avoided, the duration of use should be limited to a few days. Nourishing ointments and poultices made from chamomile or black tea can also provide relief.
Eczema on the corner of the eye
Eczema can also appear on the corner of the eye. Causes for this can be allergic reactions, but also viruses such as herpes zoster. Treatment is carried out with different ointments, which may contain antibiotics or anti-virus drugs, depending on the cause.
Eczema on the buttocks / anal eczema
An eczema on the bottom, so a Anal eczema, is a Inflammation of the skin of the anus and / or the surrounding skin (Perianal region). The course of the disease can be acute, subacute (a little more creeping) or be chronic. Anal eczema always occurs as a result of other dermatological or microbial diseases or in the context of other diseases of the rectum or anus.
The cumulative-toxic eczema, which is characterized by a weeping, severely itchy anal region, occurs in particular Hemorrhoid disease or Intestinal parasites on.
The most important treatment step is recognizing and treating the underlying disease. Contact allergic eczema, on the other hand, is triggered by allergens found in toilet paper or skin care products, for example. The corresponding products should be avoided in the future, for care it is best to only use water and pure olive oil or petroleum jelly to avoid further irritation from potential allergens. Temporarily the skin can with local Glucocorticoids be treated.
Atopic eczema, which is better known under the name, makes up a somewhat smaller proportion of anal eczema Neurodermatitis is known.
- Eczema on the buttocks
and - Anal eczema
The eczema in the baby
The most common form of eczema in babies is atopic (Greek for placeless) Eczema, better known as neurodermatitis.
However, this term is misleading in that it assumes that there is an inflammation of the nerves. In Germany, up to 15% of children develop neurodermatitis by the time they start school, 60% of them in their first age.
Thus, atopic eczema is the most common skin disease in children. The origin is multifactorial, whereby genetic predisposition, immunological changes and environmental influences such as the child's diet (e.g. cow's milk is suspected to be a trigger) seem to play a role.
Atopic eczema manifests itself primarily through very dry, sensitive skin, with the face and neck, as well as arm and knee bends being particularly affected. The most painful thing for the babies, however, is often very intense itching, which leads to the children permanently scratching the diseased skin areas.
In babies, the so-called cradle cap on the scalp can be an early form of atopic eczema. The disease usually runs in episodes and can take on very different forms and dimensions, from harmless to severe. The treatment must be adapted accordingly.
Read more on the topic: Eczema in the baby
Eczema according to its manifestation
Asteatotic eczema
Astetatotic eczema is also known as so-called desiccation eczema or dehydration eczema.
It is eczema that occurs due to the reduced fat content of the skin.
So-called lipids (fats) protect the skin from drying out and are therefore very important for a healthy skin barrier.
The lack of lipids therefore leads to inflammation of the skin.
The asteatotic eczema is a chronic eczema that is particularly due in the elderly
- improper or excessive personal hygiene or
- occurs as an undesirable side effect when taking medication.
Drugs such as isotrentinoin, bevacizumab or indinavir, in particular, promote dehydration of the skin.
The eczema usually occurs from the age of 60 and often gets worse in winter.
The extensor sides of the arms, the shins and the trunk are particularly affected.
The asteatotic eczema resembles a "dry river bed" with
- deep tears in the skin,
- Flaking and
- superficial bleeding due to being scratched by the person affected.
The therapy of astetatotic eczema takes place via a greasing of the skin and the use of cortisone ointments on the affected area in order to control the inflammation.
Atopic eczema
Atopic eczema is also popularly known as neurodermatitis.
It is a chronic inflammatory skin disease that usually occurs in childhood and is associated with a disruption of the skin barrier.
It is assumed that over 13% of children in Germany suffer - at least temporarily - from atopic eczema.
By early adulthood, around two thirds of the children originally affected are symptom-free again.
In adulthood, atopic eczema appears to affect around 2 to 3%.
Typical of atopic eczema is
- very dry skin that is prone to severe itching and eczema.
In adults and adolescents, eczema is mainly found on the flexor sides, neck, back of the hand and skin folds.
In infancy, however, the localization differs somewhat and the eczema is mainly found as a so-called cradle cap on the scalp and also on the extensor sides of the arms and legs, as well as on the face.
- Characteristic of the severely itchy eczema is the tendency to redden and crust formation.
- Scratching the skin causes cracks and, if it is protracted, hyperpigmentation, so that the skin appears darker.
Other typical changes are associated with atopic eczema, which are also known as the stigmata of atopy. These changes include:
- a deep hairline,
- a double lower eyelid fold - so-called Dennie Morgan sign -,
- a thinning of the lateral eyebrow (Hertoghe sign) and
- fading of the skin when pressure is applied (white dermographism).
Atopic eczema occurs in most cases in combination with allergies.
These are mainly food allergies.
The therapy of atopic eczema comprises a step therapy which is adapted to the severity of the eczema.
- Everyone affected receives basic care with moisturizing and water-binding creams to strengthen the skin barrier.
- Furthermore, trigger factors of eczema, such as special foods or itchy clothing, should be avoided.
- In the second stage of therapy, topical cortisone creams, disinfecting lotions and tablets that inhibit itching (antipruriginous) and topical calcineurin inhibitors are used.
The latter are drugs that regulate the immune system.
- Light therapy is also an option at this stage of therapy.
- As an extreme measure, systemic immunoregulatory therapy with tablets or injections can be carried out.
Commonly used drugs include cyclosporine, azathioprine, MMF, and also oral cortisone supplements.
- For some time now, there have also been newer drugs known as biologics.
These are only approved for severe forms of atopic eczema.
Find out more about this: Treatment of atopic dermatitis
Dyshidrotic eczema
Dyshidrotic eczema is eczema that affects the palms of the hands and soles of the feet and usually occurs in phases.
Characteristic of dishydrotic eczema is the appearance of about 0.1 cm large vesicles with a clear content.
The dishydrotic eczema can occur in the context of various underlying diseases, such as
- atopic eczema,
- palmoplantar psoriasis or
- mycosis occur.
- It can also be used in allergic contact dermatitis or
- occur as a drug side effect.
Furthermore, the cause is often unclear, then one speaks of idiopathic dyshidrotic eczema.
The eczema occurs predominantly in the warm season.
The small, clear vesicles that are characteristic of eczema usually appear suddenly and in groups on the sides of the fingers and palms - similarly on the feet.
The blisters are very itchy.
When the vesicles merge to form larger vesicles, one speaks of a pompholyx.
In this case, a bacterial or mycotic (fungal) infection of the eczema can arise as a complication.
Dyshidrotic eczema is associated with
- local cortisone preparations,
- Light therapy and
- Care of the affected areas treated.
If the infection is more severe, however, cortisone tablets are taken for therapy.
Allergic contact eczema
Allergic contact eczema occurs when the skin comes into contact with a triggering allergen.
A typical allergen that many people react to is nickel, for example.
Therefore nowadays jewelry is made nickel-free almost without exception.
Other common allergens are fragrances, Perubalm, chromium and cobalt.
Allergic contact eczema is one of the most common diseases in Germany.
Typically occurs about 24 to 48 hours after exposure to the allergen
- mostly blurred, red plaque on,
- that itches a lot and
- rises above the skin level.
If the reaction is very severe
- big bubbles that
- burst and leave crusts and erosions.
If the allergen repeatedly comes into contact with the skin, chronic eczema develops, which is characterized by the formation of scaly plaque with crusts and erosions as well as coarsening of the skin.
The therapy of allergic contact eczema mainly includes avoiding the allergen and using local cortisone preparations.
Irritant contact eczema
The irritative contact eczema is often referred to as toxic contact eczema.
It is direct damage to the skin from an external cause, such as contact with an acid.
In over 90% of cases the hands are affected, less often the feet.
One differentiates between that
- acute from
- chronic irritative contact eczema.
Acute eczema results from direct contact with a sufficient dose of the triggering substance.
Chronic irritative contact dermatitis occurs as a gradual consequence of constant contact with a substance that has only low toxicity.
This can be household cleaning agents, for example.
The skin barrier is damaged over a longer period of time.
Typically, it is a sharply demarcated eczema that occurs only where the skin came into contact with the toxic substance.
The appearance of eczema includes
- Scaling,
- Redness,
- Crusts,
- Tears and
- blistering.
Therapy consists of strict avoidance of the triggering cause and local treatment with ointments containing cortisone.
If an occupational disease is suspected, a professional doctor's procedure must be initiated and appropriate safety precautions taken at the workplace.
Nummular eczema
Nummular eczema characteristically shows therapy-resistant, coin-shaped, scaly plaques that are sometimes very itchy.
The plaques are found all over the body and can accompany congestive dermatitis.
The exact cause of nummular eczema is generally unclear.
A connection to clinical pictures such as atopic eczema, psoriasis or a chronic microbial colonization of the skin is being discussed.
Men are more often affected than women and show eczema mainly on the lower legs and less often on the thighs, back and palms.
There is no uniformly effective therapy for nummular contact eczema.
Therapy with oral antibiotics and local cortisone preparations can be used.
In severe forms of eczema, additional light therapy and internal cortisone therapy are possible.
Seborrheic eczema
Seborrheic dermatitis primarily affects men between the ages of 40 and 60 and is more common in HIV and Parkinson's patients.
The cause is a combination of excessive sebum production in the skin and over-colonization with the yeast Malassezia furfur.
Eczema improves with sunlight and worsens with stress.
Typically, it occurs in areas of increased sebum production, such as:
- the hairy scalp,
- the front and rear welding channels,
- the cheeks,
- behind the ears and
- the nose and mouth region.
The eczema shows coin-shaped, reddened foci with yellow-greasy scaling.
Sometimes there is severe itching - especially when the scalp is affected.
Often, seborrheic eczema is a visual diagnosis.
HIV diagnostics should be carried out in very young patients with pronounced seborrheic eczema, as seborrheic eczema occurs more frequently in HIV.
The therapy includes the use of creams or shampoos with the fungicidal active ingredient ketoconazole, as well as stays in the fresh air and in the sun.
If the spread is very strong, local cortisone preparations can be used.
Usually symptom-free intervals can be achieved in this way.
A cure for the eczema is not possible, so the skin changes keep spreading.
There is a special form of infant seborrheic eczema, also known as head gneiss.
Eczema primarily affects the scalp and occurs immediately after birth.
It will go away on its own after a few months.
The seborrheic infant eczema should not be confused with the cradle cap, which usually only appears after the third month of life and is accompanied by itching.
Disseminated eczema
Disseminated eczema is one of the extremely rare forms of eczema.
Women of this form are even less affected than men.
In disseminated eczema, various affected areas of the skin occur, especially on the arms and legs.
In most cases, the symptoms keep coming back even after treatment.