Myotonic dystrophy
Synonyms
Dystrophia myotonica, Curschmann disease, Curschmann-Steinert disease
engl .: Myotonic (muscular) dystrophy.
introduction
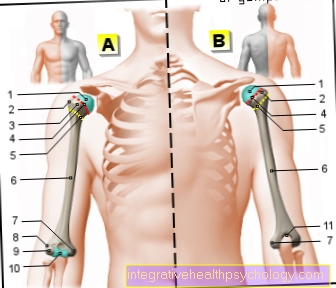
Myotonic dystrophy is one of the most common muscular dystrophies. It is associated with muscle weakness and muscle wasting, especially in the face region, neck, forearms and hands as well as the lower legs and feet. Characteristic here is the combination of the symptoms of muscle weakness and delayed muscle relaxation after contraction. In addition, disorders of other body systems occur in different degrees: testicular loss and hormone disorders, cardiac arrhythmia, clouding of the lens (cataracts), swallowing and speech disorders, occasionally the intellectual performance is impaired in the course of the disease. Myotonic dystrophy is a hereditary disease that has a tendency to appear earlier from generation to generation. A characteristic change in the genetic material on chromosome 19 was found to be the cause of the disease, which leads to a reduced build-up of a protein that ensures the intactness of the muscle fiber membrane. Overall, the severity of the disease and the involvement of various organs varies from patient to patient, and the life expectancy of the patient is primarily determined by the involvement of the heart. There is no causal therapy for the disease, the disease-related symptoms of the affected organs can be treated symptomatically with medication. There is an increased risk of anesthesia during operations, which can be reduced by using certain drugs.
definition
Dystrophic myotonia is the most common muscular dystrophy in adulthood and is associated with muscle weakness, atrophy and delayed muscle relaxation after activity. The disease can also affect various other organ systems. Clinically, there are 3 different forms of myotonic dystrophy
- a congenital (innate) with the onset of symptoms in infancy
- an adult (most common form) starting in the second and third decades of life and
- a late form that begins at an advanced age.
Epidemiology
The frequency of myotonic dystrophy is given as 1/8000 - 1/20000. The disease is inherited in an autosomal dominant manner, which means that the children of those affected have a 50% risk of developing the disease themselves, regardless of gender. There is a tendency that the onset of the disease is earlier from generation to generation and the disease is more pronounced ("Anticipation“).
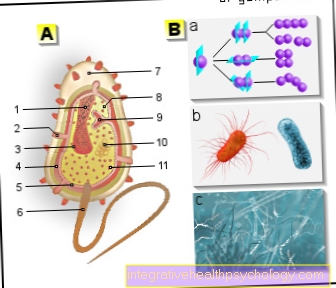
root cause
The cause of the myotonic dystrophy is the extension of a section in Chromosome 19 beyond a certain level. This leads to a reduced production of a protein that is partly responsible for the stability of the muscle fiber membrane. The extent of the lengthening increases with inheritance from generation to generation and shows a certain connection with the onset and severity of the symptoms.
Symptoms
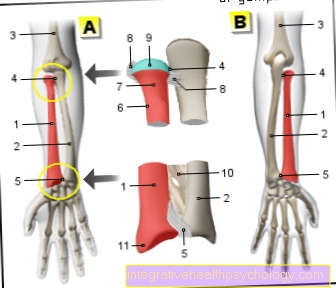
In the adult form of myotonic dystrophy, the combination of progressive muscle weakness, especially in the hand and forearm, foot and face muscles, with a delayed relaxation reaction of the muscles after exercise (myotonia). This can also be observed particularly in the hand and finger muscles, as well as in the facial and throat muscles. B. Difficulty loosening a clenched fist or opening your closed eyes again. As the disease progresses, it can lead to difficulty swallowing or, due to involvement of the respiratory muscles, impaired breathing.
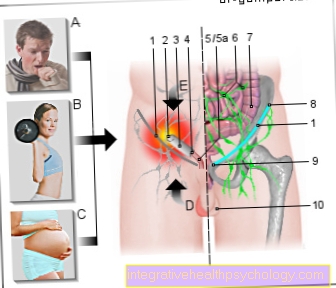
Arrhythmias are observed in the heart, palpitations and stumbling of the heart. In the area of the genital organs, symptoms such as shrinkage of the testicles, absent or irregular menstruation and pregnancy complications appear.
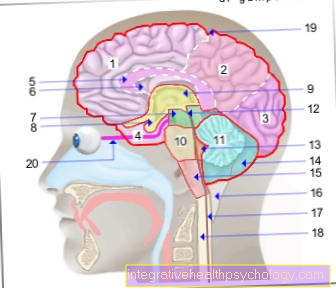
In addition, the patients often suffer from opacities of the lens (cataract, "cataract") and inner ear hearing loss.
In the childhood form of myotonic dystrophy, the affected children fall early due to muscle weakness ("floppy infant“= Flaccid newborn baby), drinking and thriving weakness and delayed motor development. The course of the disease is usually more severe. The late course of the disease can, under certain circumstances, be atypical and, for example, only be discovered in the context of further diagnostics for cataracts or in the context of a family clarification of cases of illness in direct offspring. Patients with myotonic dystrophy have an increased risk of anesthesia, as the disease can lead to various common anesthetics more frequently to complications, especially in the area of the cardiovascular system and respiration, than in healthy patients. It is therefore important that the anesthetist is informed about the presence of the disease in advance of an operation.
Differential diagnoses
Differential diagnoses include other myotonic disorders depending on the prevailing symptoms (delayed relaxation of the muscles) or other muscular dystrophies (muscle wasting). Furthermore, diseases of the nervous system can lead to weakness and loss of the muscles controlled by the affected nerves.
Diagnosis
Clinically groundbreaking is the presence of myotonia (delayed relaxation) of the muscles with muscle atrophy (reduction in size and shrinkage of the muscles). When measuring the electrical muscle activity in the EMG (electromyogram), a characteristic finding of the low level of the individual rashes (as in muscular dystrophies) and the occurrence of rapid discharge series (as in myotonia, so-called "Dive bomber noise).
The blood test shows the symptoms of muscle cell death (increased value of a muscle enzyme, "CK") and possibly the consequences of involvement of the endocrine system (decreased values for sex hormones). The human genetic examination can detect the elongation of a section on chromosome 19 in blood cells, which is characteristic of myotonic dystrophy. If the diagnosis of myotonic dystrophy has been made, it is important to clarify the function of the heart at least by means of an EKG (electrocardiogram) in order to find indications of a possible dysfunction at an early stage.
therapy
A causal therapy for myotonic dystrophy is currently not possible. Cardiac arrhythmias can be treated with medication and, if necessary, with a pacemaker, and muscle spasms with medication that have a stabilizing effect on the activation state of the muscle cell. If there are hormonal disorders, these can also be treated with medication. To a certain extent, physical therapy can be used to counteract the symptoms of muscle weakness in order to ensure the patient's mobility and to prevent poor posture.
forecast
The disease progresses slowly and varies from patient to patient. The life expectancy of patients is reduced to an average of 50-60 years, and death often occurs Heart failure a.



.jpg)