What types of depression are there?
Overview of the types of depression
Depression has long been a known disease. Over the years, numerous scientific studies have gained new knowledge about the disease, its course and its neurobiological processes. Thus the perception of the disease has changed.The number of originally defined subtypes has also been significantly reduced to this day.

The first type of depression is what is known as unipolar depression. This type is divided into mild, moderate and severe depressive episodes. The fourth subtype is the severe depressive episode with psychotic symptoms. In addition to the symptoms of severe depression, there are also delusions and hallucinations.
Unipolar depression is unidirectional and is different from bipolar disorder (e.g. manic-depressive illness).
The next major classification group is that of recurrent depressive disorder. So this is a recurring depressive episode. In patients who have already suffered more than one depressive episode, it is always a recurrent depressive disorder. This group also includes winter depression, a seasonal depression.
A third group of depression is persistent mood disorders. Here the symptoms are often not as severe as in "real" depression or mania. However, the symptoms persist for a much longer period of time and do not occur in episodes.
Cyclothymia and dysthymia are sub-forms of this group. In cyclothymia, the mood alternates regularly between phases of depression and phases of elation. The symptoms do not reach that of pure depression or pure mania.
Dysthymia is a chronic depressive mood that lasts for years, also with weak symptoms.
Bipolar disorders are closely related to depression. Here episodes of depressed mood and manic episodes occur alternately. The bipolar disorders have subclasses. A distinction is made between whether it is a manic or depressive episode and whether psychotic symptoms such as delusion or hallucinations are present at the same time.
A group belonging to depressive disorders in the broader sense is that of reactions to severe stress and adjustment disorders. These include acute stress reactions, post-traumatic stress disorders and adjustment disorders. Theoretically, one could also mention mental disorders in the puerperium in a broader sense. These include, for example, depressive episodes that occur for the first time within 2 years of the child's birth.
Apart from the above-mentioned subclasses, there are no further subdivisions of depression in the international classification of diseases (ICD-10). Terms like neurotic depression, reactive depression, or somatogenic depression were used earlier, but are now out of date.
Endogenous depression / major depression
Obsolete nowadays, a distinction used to be made between internally induced depression, reactive depression and neurotic depression caused by external events.
This subdivision has been changed because it is assumed that all depressions arise from the interplay of various internal and external factors (multifactorial genesis).
The term "major depression" is used to describe a major depressive episode (major = large, significant). The patient shows all three main symptoms of depression: depressed, sad mood, loss of joy and interest, and severe listlessness. In addition, there are at least five secondary symptoms. These include, for example, loss of self-esteem, feelings of guilt, decreased appetite and weight loss, sleep disorders with early waking and morning low, suicidal thoughts, poor concentration and a negative future perspective.
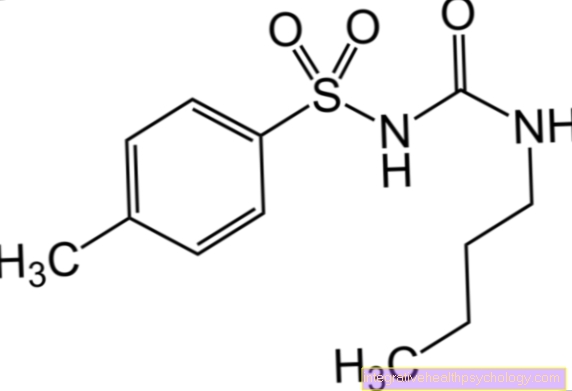
A severe depressive episode is an illness that requires urgent treatment and is extremely stressful for the person concerned and their relatives. The drug of choice here is often drug therapy in combination with psychotherapy.
Manic Depressive Disorder
Manic-depressive disorder is a bipolar disorder. Bipolar describes that there are two poles of mood between which the person concerned fluctuates back and forth. In contrast, there is unipolar depression with only one mood pole.
The bipolar disorders belong to the upper group of affective disorders. To be diagnosed, the patient must have had at least one manic and one depressive episode. In most cases, that doesn't mean that people's mood will fluctuate within a day. It is more likely that those affected have longer-lasting episodes that are characterized by one of these two mood extremes.
Patients with bipolar disorder can be depressed for months, but manic episodes can also occur that last for weeks to months. Exceptions to this are patients with so-called ultrarapid cycling. Within a few days there are fluctuations between one and the other extreme.
The symptoms of a depressive episode have already been mentioned above. The main symptoms include sadness, a loss of happiness and interest, and a reduced drive, with other secondary symptoms. In a manic phase, the symptoms turn into the opposite.
Those affected have a permanently elevated, exuberant or irritable mood for at least a week. Other symptoms are: megalomania and clearly increased self-confidence. A significantly reduced need for sleep, often only 2-3 hours per night for weeks.
There is also a strong urge to talk. The subjective feeling that the mind is racing. This is noticed by the listener as a flight of ideas. Here the manic patient jumps from one topic to the next apparently without any sense or understanding, the listener has difficulty following the context. Excessive spending, gambling or sexual activity are also possible "side effects" of mania. It is not uncommon for patients to go into debt because they can no longer objectively assess their actions.
Bipolar disorder occurs on average at a younger age than pure depression. The mean age of onset at the onset of the first episode is between the ages of 17 and 21. Men and women get sick about equally often.
At this point, you can also read our main page on bipolar disorder at: What are the symptoms of bipolar disorder?
Cyclothymic disorder
Cyclothymia is one of the persistent mood disorders. It describes a persistently unstable mood that constantly fluctuates between two extremes. So it is manic-depressive illness (bipolar disorder) in a weakened form. Episodes with a slightly depressed mood are replaced by episodes with a slightly manic (hypomanic) mood. However, the depressive and manic symptoms never reach the extent of depression or bipolar disorder. Some patients with cyclothymia develop depressive disorder during their lifetime.
People who suffer from cyclothymia have more than average relatives who suffer from bipolar disorder. Cyclothymia usually develops at an advanced age and often lasts for a lifetime.
Neurotic depression
The term neurotic depression is out of date. Today it is no longer used in the classification of mental illnesses. As mentioned earlier, depression used to be divided into three types. Reactive depression triggered from the outside, endogenous depression triggered from the inside, and neurotic depression triggered by emotional stress. An experience of emotional overstrain was seen as a trigger for neurotic depression.
Today, the term dysthymia has replaced the term neurotic depression. Like cyclothymia, dysthymia is one of the persistent mood disorders. It is a chronic depressive mood that lasts for several years (sometimes for a lifetime) and in terms of its severity does not reach the level of depression.
So the symptoms of dysthymia are similar to those of depression, but they are not as pronounced. Compared to depressive episodes, which if left untreated, usually last a few months, dysthymia is chronic.
People with dysthymia are at increased risk of developing depression. They suffer above average from other mental illnesses such as anxiety disorders, personality disorders, somatoform disorders and alcohol and drug abuse.
The first signs of dysthymia often appear in childhood. The therapy of dysthymia is almost analogous to that of a depressive episode. Drug therapy with antidepressants and / or psychotherapeutic treatment are possible.
Somatogenic Depression
The term somatized / somatic depression is also out of date these days. Nowadays we speak of a masked depression. In masked depression, the depression is masked by the superficial appearance of physical symptoms. There are unspecific physical complaints such as back pain, headache, feeling of pressure on the chest and dizziness. It often takes a long time before the psychological symptoms, i.e. those of depression, emerge so that the correct diagnosis can be made.
Not to be confused with somatogenic depression, but it means something completely different. Somatogenic depression is depression that is causally triggered by a physical illness. Numerous diseases can cause somatogenic depression. The most typical examples are patients with cancer, patients after a heart attack or patients with diseases that are associated with chronic pain. The treatment is medication and psychotherapeutic.
Psychogenic Depression
Three types of depression are summarized here under psychogenic depression: reactive depression (outdated term), neurotic depression (outdated term) and exhaustion depression. All these three forms of depression have in common that they are triggered by a certain emotional event such as traumatic experiences. Examples are divorce, death of a close relative, loss of job, accident or violence.
In the classification of mental illnesses, the term psychogenic depression is most likely to be found under the collective term of reaction to severe stress and adjustment disorders. This is not depression in the strict sense. This is discussed in more detail in the next paragraph.
Reactive depression
Reactive depression is a psychogenic depression. However, both terms are no longer relevant. Reactive depression means the development of depressive symptoms in response to an emotionally stressful event. Today this type of mental disorder can be found under the Reaction to Severe Stress and Adjustment Disorders section.
The following disorders are found in this area: the acute stress reaction, the post-traumatic stress disorder and the adjustment disorder.
The acute stress reaction occurs quickly after strong psychological or physical stress. It subsides within a few days. Affected people describe the feeling of standing next to them, the ability to concentrate is clearly restricted, restlessness with sweating, fear and racing heart can occur.
Post-traumatic stress disorder (PTSD) occurs after a catastrophic event. As a rule, it does not start immediately after the event, but weeks to months later. Those affected experience the trauma again and again in so-called flashbacks, resulting in nightmares, feelings of emotional numbness, listlessness, joylessness, frightfulness, sleep disorders and fear. Thoughts of suicide are common. PTSD is usually not chronic, but it can last for many months.
The adjustment disorder occurs after stressful life events or changes in living conditions. Examples are separation or bereavement. It leads to a depressed mood, fear, worry and feeling overwhelmed in everyday life. The symptoms usually go away within six months. In the case of adjustment disorder and post-traumatic stress disorder, the use of drug / psychotherapeutic therapy can be necessary and helpful.
Winter depression
Winter depression is known in technical jargon as seasonal depression. In the classification of mental illnesses, it is subsumed under recurrent depressive disorders. As the name suggests, this type of depression occurs primarily in the winter months. This is believed to be related to the lack of daylight at this time of year, which can cause depression in susceptible patients.
In contrast to non-seasonal depression, winter depression is often associated with an increased need for sleep and an increase in appetite with weight gain. Light therapy, in particular, has established itself as a means of treating seasonal depression. In the morning after getting up, the light of a very bright special lamp is used for about 30 minutes. This is supposed to minimize the lack of light, which is the main trigger for depression, and thus alleviate the depressive symptoms.
PMS
Premenstrual syndrome (PMS) is associated with physical and psychological complaints and occurs shortly before the onset of the female period. Mood swings, irritability, and rapid crying often occur during this phase. Some women have severe depressive symptoms. These include sad mood, sleep disorders, loss of interest and joylessness, tension and cravings.
If the symptoms are severe, it is also referred to as premenstrual depression (PMD). This often occurs month after month and is very stressful for the women concerned. It can initially be assumed that hormonal fluctuations are the cause of the symptoms, but no reliable evidence has yet been found for this. Depending on how pronounced the symptoms are and how high the level of suffering is, drug therapy with antidepressants may be considered.
Find out more about the topic here: Premenstrual Syndrome and Depression.
Childhood Depression
Children can also suffer from depression, even if the age peak for the disease is later. It is estimated that around 3.5% of primary school children and up to 9% of teenagers suffer from depression.
Depending on the age of the child, depression shows up differently than in adults. In young children who are not yet of school age, anxiety, physical complaints such as abdominal pain, loss of appetite, sleep disorders and outbursts of emotions with aggressive behavior can be groundbreaking. In adolescents, the typical symptoms of depression are more likely to emerge. However, with a special focus on a disorder of self-esteem, hopelessness, a feeling of worthlessness and the feeling that “everything doesn't matter anyway”.
Sleep disorders, decreased appetite and weight loss, and social withdrawal are also common. Sad mood, loss of interest and joylessness can be added. Thoughts of suicide also play a decisive role in adolescents and should definitely be taken seriously. In adolescents in particular, self-harming behavior is common. This can occur in healthy adolescents, but it can also indicate the onset of suicidality or a feeling of emptiness and numbness.
Depressive episodes in children are usually shorter than those in adults; they usually do not last longer than 3 months. Medicinal and psychotherapeutic variants are used therapeutically. A major depressive episode often requires hospitalization. Bipolar disorder, in particular, a change from episodes of manic and depressive moods, occurs relatively early in life and can therefore already manifest in adolescence.
During the manic phases, there is strong self-overestimation, mood swings, reduced need for sleep, the urge to talk and excessive sexual behavior. At the other extreme, the symptoms of a depressive episode appear, which have already been described in detail above. Especially during puberty, it is not always easy to distinguish whether the behavior of the adolescent is still normal or already psychologically abnormal behavior. Conversations with teachers or friends may also help. Children and adolescents with depression or bipolar disorder should definitely be presented to a psychiatrist and / or psychologist in order to plan the further necessary therapeutic steps.