Aortic regurgitation
definition
The Aortic regurgitation is a Valvular heart disease of the Aortic valvebetween the left ventricle and the artery (aorta) is positioned. In the case of aortic valve insufficiency, the aortic valve no longer closes sufficiently, so there is one Leakcausing blood to flow back into the left ventricle against the actual direction of flow. This additional volume stresses the left ventricle and leads to a Increase in muscle mass and Expansion of the chamber.
Aortic regurgitation can result from either a disease of the flap come themselves or the ascending main artery following the aortic valve is diseased. This can then also be a Damage to the aortic valve condition.
In general, a chronic Aortic regurgitation of one acute Define aortic regurgitation.

Classification
Aortic valve insufficiency can be classified according to the time course - acute or chronic - or the severity.
Acute aortic valve insufficiency occurs suddenly and is usually caused by either a bacterial inflammation of the aortic valve or a dissection (splitting of the wall with bulging of the outer layers) of the aorta.
Chronic aortic valve insufficiency is characterized by a slow course with gradual development of the symptoms and can have various causes. An examination of the heart using ultrasound, color Doppler examination and ECG can determine the severity of the insufficiency. Decisive for the classification are the blood return flow and the damage to the heart muscle resulting from the additional stress.
First degree aortic regurgitation
First-degree aortic valve insufficiency is characterized by a backflow from the aorta through the non-closing aortic valve into the left ventricle (best seen in the color Doppler examination).
The return current has not yet damaged the heart, the walls of the left ventricle are not yet thickened and accordingly the EKG and the X-ray image are normal. The difference between systolic and diastolic blood pressure is still normal and is less than 60 mmHg (blood pressure amplitude).
Second degree aortic regurgitation
If the aortic valve closes increasingly poorly, the blood volume flowing back increases. This can be measured in the color Doppler examination. In the ultrasound of the heart you can see the incipient enlargement of the left ventricle due to the constant volume load. The signs of an enlarged left ventricle (so-called left heart hypertrophy) are also visible in the ECG and the X-ray. The blood pressure amplitude is now increased and is between 60 and 75 mmHg in the second-degree insufficiency.
Third degree aortic regurgitation
In third degree aortic regurgitation, the amount of blood flowing back is now more than half to three quarters of the amount ejected.
The volume load for the left ventricle is high, which can be clearly seen in the ECG, cardiac ultrasound and X-ray image. The blood pressure amplitude is around 110 mmHg with a low diastolic value (e.g. 160 mmHg systolic to 50 mmHg diastolic). The high amplitude of blood pressure is generally a characteristic of aortic valve insufficiency.
Figure heart valves

- Tricuspid valve -
Tricuspid valva - Mitral valve -
Valva mitralis - Aortic valve -
Valva aortae - Pulmonary valve -
Valva trunci pulmonalis - Right atrial -
Atrium dextrum - Right ventricle -
Ventriculus dexter - Left atrium -
Atrium sinistrum - Left ventricle -
Ventriculus sinister - Papillary muscle -
Papillary muscle - Superior vena cava -
Superior vena cava - Aortic arch - Arcus aortae
- Pulmonary artery trunk -
Pulmonary trunk
1 + 2 sail flaps
= Atrial clamp valves
= Atrioventricular valves
= AV valves
3 + 4 pocket flaps
You can find an overview of all Dr-Gumpert images at: medical illustrations
causes
Congenital aortic valve insufficiency is rare. One cause of a congenital form would be a so-called bicuspid aortic valve, an aortic valve with only two pockets. Usually, however, the aortic valve consists of three pockets, which is why a healthy aortic valve is called a tricuspid aortic valve.
If the aortic valve insufficiency does not exist from birth, the causes vary depending on whether the inadequate closure of the aortic valve occurs acutely or chronically, i.e. develops over years or decades.
Acute aortic valve insufficiency is usually caused by bacterial colonization of the valve as part of a bacterial inflammation of the inner lining of the heart (endocarditis). Less common causes are trauma or acute splitting of the wall layers of the aorta (aortic dissection).
Read more on this topic: Aortic dissection
Aortic valve insufficiency that develops over a longer period of time, correspondingly chronic aortic valve insufficiency, can be the result of a bicuspid aortic valve (see above).
A rheumatic fever after infection with streptococci can also lead to shrinkage and deformation of the aortic valve due to inflammatory processes.
Further reasons can be atherosclerotic changes (beyond the age of 60), connective tissue diseases such as Marfan syndrome or Ehlers-Danlos syndrome or the sexually transmitted infectious disease syphilis (syphilis). They widen the ring in which the aortic valve is anchored or widen the start of the main artery.
Frequency distribution
The aortic valve is that Heart valve, the most common one acquired valvular disease having. However, in the majority of cases there is a so-called Aortic stenosis, that is, a narrowing of the aortic valve. The one described here is less common Aortic regurgitation.
Detectable aortic valve insufficiency, regardless of the severity, is approx. 10% of the population to be found. Men are more often affected than women.
Symptoms
Acute aortic valve insufficiency presents itself as a serious clinical picture with acute left heart failure, which means that the left ventricle is no longer able to supply the body with sufficient blood. This causes a drop in blood pressure, to which the body responds with an increase in heart rate, which can be felt as a racing heart.
In its maximum form, this condition can lead to cardiogenic shock, which means that the heart does not provide enough blood for the organs of the body and also for itself.
Because the blood is not transported into the body to a sufficient extent, it backs up into the pulmonary circulation via the left atrium and causes a water lung (pulmonary edema) with shortness of breath.
In contrast to the pronounced symptoms of acute aortic valve insufficiency, chronic aortic valve insufficiency cannot cause any symptoms for years or even decades. Typical and relatively specific for chronic aortic valve insufficiency is a high blood pressure amplitude, for example with values of 180/40 mmHg. So there is a high systolic and a low diastolic blood pressure value. This requires a large and rapid pulse, which is known as the Pulsus celer et altus ("Water hammer pulse").
In addition, the systolic blood pressure in the legs may be more than 60 mmHg above the systolic blood pressure in the arms (Hill phenomenon).
Other pulsation phenomena can also be detected. These include, for example, a pulse-synchronous roar in the head, pulse-synchronous nodding of the head (Musset sign), pulse-synchronous pulsations of the uvula or pulsating carotid arteries.
After many years of complete freedom from symptoms, a reduction in performance and rapid fatigue can be recorded. Also shortness of breath due to the backflow of blood into the lungs, chest pain (Angina pectoris) Due to the reduced blood flow to the coronary arteries and left heart failure (the left heart chamber can no longer supply the organs of the body with sufficient blood) are symptoms that occur later.
You can also find detailed information under Symptoms of heart failure.
diagnosis
In the beginning there is external examination by simply looking at the patient. Is there a chronic aortic regurgitation before, the first signs can already be seen here, such as the pulse-synchronous nod of the head.
The Measurement of the Blood pressure yields values of, for example 180/40 mmHg. If the values measured on the legs are compared with the values measured on the arms, the systolic blood pressure legs 60 mmHg above that of arms.
At the next Palpation of body structures falls in the context of chronic aortic valve insufficiency, the so-called Pulsus celer et altus up, so a big and fast one Pulse. Also the Heartbeat, i.e. the palpable beating of the apex of the heart on the Chest wall, is amplified when touched and shifted down and left. These symptoms are absent in the case of acute aortic valve insufficiency.
For further diagnostics, listening to the stethoscope and playing Electrocardiogram (EKG) a role. In acute aortic valve insufficiency, the ECG is normal. Even with mild to moderate chronic aortic valve insufficiency, the ECG can still appear ordinary, with increasing severity signs of a Increase in muscle mass the left ventricle.
Furthermore, in a X-ray make out certain signs of the heart. In acute aortic regurgitation, the heart itself is normal, but there are signs of it Pulmonary congestion turn off. If, on the other hand, there is chronic aortic valve insufficiency, the heart is enlarged on the X-ray.
The so-called Echocardiography, so the Ultrasound scan of the heart, is the fastest and best method of examining acute or chronic aortic valve insufficiency today. It can either be done by placing the ultrasound head on the chest (so-called transthoracic echocardiography, TTE) or from the esophagus in which the patient has to swallow a tube with an ultrasound probe (so-called transesophageal echocardiography, TEE). Usually, however, an ultrasound scan of the surface of the chest is sufficient.
With the help of this ultrasound scan, the diagnosis can be confirmed and it can be determined how much blood is on the skin Aortic valve back to the left chamber flows.
Ultimately, a Left heart catheter examination Bring information. This takes place as soon as the diagnostic methods listed above do not provide sufficient information.
Heart murmurs
The heart sounds, which can be heard during the physical examination with a stethoscope, can be derived from the disease mechanism.
A first and a second heart sound can be heard in healthy people. The first marks the beginning of systole (ejection phase), the second the beginning of diastole (filling phase).
Since blood flows back into the left ventricle of the heart during diastole in aortic valve insufficiency, a decreasing flow noise can be heard shortly after the second heart sound (so-called early diastolic Decrescendo sound). In the case of higher-grade aortic valve insufficiency, the so-called Austin Flint sound occur, which has a rumbling character, begins in the middle of the diastole and extends into the early systole.
Read more about this under Heart murmurs.
echo
An ultrasound examination or echography of the heart is the best examination method to determine pathological changes. It can be performed externally through the wall of the chest or under short anesthesia through the esophagus.
The color Doppler examination, with the help of which flow movements can be observed, is particularly important. In a healthy heart, the valves should close tightly during the heart's actions. In the case of insufficiency, however, you can see a return flow into the heart chamber through the leaky valve during diastole, i.e. the filling phase of the heart chambers. This can be represented in the color Doppler as a so-called jet.
For more information, see Echocardiography.
therapy
The therapy one Aortic regurgitation can be done either conservatively or surgically.
Conservative therapy:
In general, patients who do not feel any symptoms and also can function well left ventricle own, be treated conservatively.
This includes one medical therapy with the aim of lowering the resistance against which the left ventricle works and keeping it as low as possible, so that sufficient blood is ejected from the heart and as little blood as possible back into the left ventricle flowing back.
Exists at the same time high blood pressure, it must be consistently controlled and treated efficiently, otherwise the aortic valve insufficiency will worsen.
Is there a Left heart failurewhich usually causes symptoms and for which no operation is possible, so should the left heart failure with the usual drug measures are supplied. Come for this ACE inhibitors, Beta blockers, Dehydrating agent (Diuretics), Aldosterone antagonists and Cardiac glycosides like digitalis into consideration. The use of these drugs follows a step-by-step plan of the New York Heart Association (NHYA).
With no symptoms and if the condition is stable, the patient should see a doctor every 12 months. If the changes in the heart have progressed further or if there is a change in the state of health, a doctor should be consulted every 3 to 6 months.
In the case of acute aortic valve insufficiency, it must acute left heart failure treated quickly. If this drug therapy does not lead to rapid improvement, an operation must be performed.
Is the acute aortic regurgitation by a bacterial colonization of the inner lining of the heart (endocarditis) conditionally, a antibiotic therapy be initiated.
Operative therapy:
Surgery should be considered when symptoms appear. Conservative therapy is then no longer to be advocated.
Sometimes an operation is also appropriate for patients without symptoms. This is the case when the so-called Ejection fraction (EF) is less than 50%.
The Ejection fraction (EF) is a ratio, namely the ratio of the blood, which in a Contraction from the heart is ejected to the whole blood in the left ventricle. With the help of the ejection fraction, a statement about the heart function can be made. Usually she gets with the help of a Ultrasound scan of the heart calculated and it should be over 55%.
Surgery may also be necessary for patients who do not experience any discomfort and who also have an ejection fraction (EF) of more than 50%. This is the case when the diameter of the left ventricle at the end of the relaxation and filling phase (diastole) is larger than 70 mm or at the end of the tension and discharge phase (Systole) larger than 50 mm. The easiest way to determine this is to do an ultrasound scan of the heart.
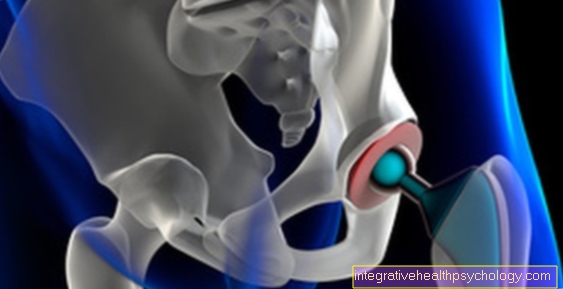
Surgical therapy for aortic valve insufficiency is usually a Valve replacement performed, that is, your own Aortic valve will be removed and replaced. The replacement can either be biological, i.e. consist of human or animal tissue, or the replacement is mechanical, i.e. manufactured artificially.
Indications for surgery
A recommendation for surgical treatment of the aortic valve insufficiency is made as soon as the disease becomes symptomatic. Symptoms include shortness of breath and reduced resilience, measurable in cardiac ultrasound.
Should the ejection rate of the left ventricle be less than 50% (so-called ejection fraction) or the diameter at the end of the ejection phase of the heart (systole) greater than 50 mm, these would be objective criteria for the incipient weakness of the left ventricle. The aortic valve should then be replaced to avoid major damage to the heart muscle from the insufficiency.
forecast
Patients with a chronic aortic regurgitation can be without discomfort for long periods of time. The life expectancy is without a mild to moderate chronic aortic valve insufficiency Symptoms not reduced. If the aortic valve insufficiency is more advanced, only those are still alive 10 years after the diagnosis Half of those affected.
Patients who already have symptoms have one worse prognosis on. Become Chest pain (angina pectoris) felt, the survival time is about 5 years, with symptoms of a weakness of the left heart (Left heart failure) the survival time drops to about 2 years.
The less the left ventricle was damaged before the operation, the better long-term prospects for patients who have undergone an operation.
How does aortic valve insufficiency affect life expectancy?
Aortic valve insufficiency puts a strain on the entire cardiovascular system. The disease progresses slowly, there is no spontaneous regression of the insufficiency or recovery of the aortic valve.
On the one hand, the heart muscle of the left ventricle sustains permanent damage from the volume load, which can result in cardiac insufficiency or arrhythmias. The heart tires more quickly and is less able to supply the body and its own muscle cells with vital oxygen.
On the other hand, as the volume load increases, the blood backs up from the left ventricle via the left atrium to the lungs or even to the right heart. The result is a congestion of the lungs up to pulmonary edema. The patient experiences shortness of breath as a symptom.
All of these factors can logically lead to a shortening of the lifespan at some point. The age at onset therefore plays an important role in life expectancy. The earlier aortic valve regurgitation is diagnosed, the higher the likelihood that the disease will eventually become life-limiting and require surgery.
Is it allowed to do sport with aortic valve insufficiency and if so, which one?
As long as the aortic valve insufficiency does not cause any symptoms or restricts everyday life, you can still do moderate exercise.
It is important, however, that a sport is chosen that demands the cardiovascular system evenly.
For example, sporting activities such as
- Cycle,
- leisurely jogging
- or swimming.
Competitive sports of any kind or sports with a sudden increase in performance, such as bodybuilding or ball sports, are not suitable and can even accelerate the course of the disease. Stress can also have a negative effect and put additional strain on the heart muscle.
However, as soon as symptoms arise that are associated with aortic valve insufficiency, all physical activity should be stopped. If the stress is too high, the disease becomes noticeable quickly with symptoms and sport should be stopped. The right balance between physical activity and protection of the heart is essential.