Blood clots
definition
Blood clots can block blood vessels and lead to a number of different diseases and consequences (e.g. pulmonary embolism, heart attack, etc.). Blood clots arise, for example, from vascular injuries or a slower blood flow rate. They can arise in both arteries and veins. Blood clotting disorders and disorders can also lead to the formation of blood clots. Blood clots can be classified according to their composition and where they originated.

Causes of a blood clot
There are a number of different causes that can cause blood clots to form. Blood clot ("Thrombi") are constantly forming in our bloodstream. This is not a concern because our coagulation system can usually dissolve these thrombi on its own. So there is always a balance between the clotting of the blood and the dissolving of clots. This is important because good coagulation is necessary for wound healing, for example. Disturbances in the coagulation system and existing risk factors, such as smoking, can lead to an abnormally increased coagulation of the blood and thus to the formation of clots that cannot be broken down again. These can cause infarctions, embolisms and thromboses.
Hereditary thrombophilia is one of the main culprits. This is a genetic predisposition that leads to an increased formation of blood clots. Such predispositions are sometimes associated with an up to 80-fold higher risk of thromboembolism compared to the genetically unaffected population. The APC resistance, the factor 8 increase, the prothrombin mutation, the protein C and protein S deficiency and the antithrombin deficiency should be mentioned. All of these clinical pictures or predispositions intervene in our coagulation system in such a way that the blood coagulates more quickly and blood clots form.
Other risk factors for developing blood clots include
- Obesity
- Lack of exercise or immobilization (e.g. on long-haul flights, long bus trips)
- Heart failure
- severe infectious diseases
- Tumor disease
- increased tendency for blood to clot (e.g. after using artificial joints such as hip replacement or knee replacement)
- Pregnancy or after childbirth
- Diseases that are associated with increased viscosity (toughness) of the blood, such as polycythemia vera
- Estrogen therapy (e.g. hormone replacement therapies for menopause or contraceptive drugs)
- Smoking (especially in combination with preparations containing estrogen)
- Antiphospholipid syndrome
- Vascular wall changes due to arteriosclerosis
- Factors promoting arteriosclerosis such as smoking, high blood pressure and diabetes mellitus
Symptoms of a blood clot
Blood clots can trigger a wide variety of symptoms, depending mainly on where the clot formed or where it was taken. This results in very different clinical pictures, each of which is associated with a characteristic symptom.
Some of the most important medical conditions caused by blood clots are:
Heart attack and coronary artery disease
Various risk factors such as smoking, obesity, high blood pressure and diabetes mellitus lead to changes in the coronary arteries, which is known as atherosclerosis. So-called Plaques that are attached to platelets (thrombocytes) can. In the end it comes to that Vasoconstrictionwhich cause the clinical picture of coronary heart disease or lead to complete vascular occlusions (stenoses) when blood clots are detached. This usually leads to the classic Heart attack. The Key symptoms is referred to as Angina pectoris. It manifests itself through acute onset pain, which is localized behind the sternum. Patients also refer to this as chest tightness or speak of a feeling “as if someone were sitting on their chest”. A pain radiating to the left arm is also typical. In women, however, the symptoms can be a little more unspecific, so that sometimes there is only a dull pain in the area of the back or upper abdomen. It can continue to Sweats, nausea, vomiting and one strong fear response come.
Read our articles on this Heart attack and Signs of a heart attack
Thrombosis and pulmonary embolism
Blood clots can develop as venous thrombi in the venous system fix and there too Vascular occlusions to lead. Typically it can lead to a Closure of the deep leg veins come, which one as Phlebothrombosis designated. The affected leg may have a dull ache, be swollen and overheated, and show increased vein markings. There is a risk that the blood clot will break loose and through the venous system to the lungs is abducted. There the thrombus leads to one Pulmonary embolism. This is expressed in a acute shortness of breath with dizziness and weakness.
Read our articles on this Thrombosis pain and Pulmonary Embolism Symptoms
Phlebitis
The so-called Thrombophlebitis is a Inflammation of the superficial veins in the legscaused by blood clots. The inflamed vein is often hard and palpable, tender on pressure, overheated and reddened. You can feel it through the skin as a hard strand.
Please also read our article on this Phlebitis
More symptoms
In principle, blood clots can be carried into any organ and lead to small or large vascular occlusions and heart attacks. The symptoms also depend on the location of the event. For example, occlusions of cerebral vessels with acute neurological failures, as well as a stroke, or a splenic vein infarction with unspecific symptoms such as upper abdominal pain can occur.
diagnosis
The necessary diagnosis depends on the underlying clinical picture. While in an acute emergency situation, such as a heart attack or pulmonary embolism, rapid intervention is required, in the case of other manifestations such as thrombophlebitis, a detailed discussion with the patient is possible first. It is important to understand that there is no general diagnosis because the blood clot as such is not an independent clinical picture. In the anamnesis (patient discussion) it is important to be present Risk factorsthat can lead to increased clot formation and eliminate them as quickly as possible. These include, for example: Nicotine consumption, obesity, high blood pressure, poorly controlled diabetes mellitus, hyperlipidemia (high blood fat levels) Diseases of the coagulation system such as APC resistance, pregnancy, estrogen therapy, a old age (over 60) or one positive family history. The latter means that relatives suffered early from illnesses that were related to a blood clot (e.g. pulmonary embolism).
At a suspicion of a Leg vein thrombosis or a Pulmonary embolism as a result of a blood clot the so-called D dimers determine. These would be in this case elevated. Often the D-dimers are positive even without the presence of a leg vein thrombosis, so that an increase in the value alone does not indicate the presence of a disease.
In addition, imaging methods such as Ultrasound examination applied. A special examination that is very effective in diagnosing leg vein thrombosis is Compression sonography of the leg veins. An experienced examiner can identify a leg vein thrombosis very well. Procedures such as CT and MRI are also used, but are not part of the standard diagnosis.
Please also read: Detect thrombosis and Detect pulmonary embolism
When Blood clots in very atypical locations or a very young age of onset advanced thrombophilia diagnostics respectively. These diagnostics are intended to reveal diseases that lead to an increased tendency to clot. This includes, for example, APC resistance or the antiphospholipid syndrome. However, this is a special diagnosis that is based on the underlying tendency to clot, also known as thrombophilia.
In the diagnosis of the Heart attack stand that EKG, the Determination of the so-called heart enzymes (Troponin T) and the imaging process in the foreground. The latter are mainly the Echocardiography, the CT scan of the coronary arteries and the Coronary angiography. With the help of the CT and the cardiac catheter examination, the vessels can be displayed precisely so that the existing constrictions and their location can be seen.
Please also read: Diagnosing a heart attack
Another very important method with which vascular occlusions caused by blood clots can be displayed very nicely is that Angiography. During this investigation will be Vessels visible with the help of X-rays and contrast media made. Imaging tests like angiography, MRI and CT are still available for that Diagnosis of ischemic stroke, which is caused by the closure of important brain vessels as a result of a blood clot, is very important.
Dissolving a blood clot
Blood clots can be dissolved with the help of certain drugs. However, the dissolution of a clot is not always preferred in the therapy of thrombotic and embolic events, so that mechanical methods in which the clot is removed, for example by an instrument such as small forceps, are also used. In the treatment of strokes, clots with a so-called Lysis therapy to be resolved. The r-tPA is used for this. This medication can dissolve the clot. However, the procedure can only up to 4.5 hours after the onset of stroke symptoms be applied.
Anticoagulant drugs are commonly used when dissolving blood clots. In the case of a thrombosis of the leg veins, e.g. Heparin or anticoagulant tablets like Apibaxan used. In long-term therapy, the anticoagulant drug is usually used Marcumar® (Phenprocoumon) used. The duration of the medication depends on the severity of the disease and the risk factors present.
Please also read our topic on this Thrombosis prophylaxis
Blood clots in the head / brain
stroke
Almost 90% of strokes are called ischemic. This leads to an occlusion of an important vessel and, as a result, to one Insufficient supply of blood, nutrients and oxygen to the brain. A distinction is made between vascular occlusions caused by blood clots ("Embolus") arise, of these, the locally formed clots ("Thrombus") occurrence. Risk factors for embolic vascular occlusions of the brain are e.g. Atrial fibrillation or one Narrowing of the carotid artery ("Carotid stenosis").
Please also read our article on this Clogged carotid artery (carotid stenosis)
But there are also underlying diseases such as Diabetes melittus, high blood pressure, high blood fat levels (Hyperlipidemia), Obesity and a Nicotine abuse crucial for the formation of blood clots in the brain. These mainly lead to the closure of small vessels (lacunar infarction). Typically it comes to Stroke symptoms, which is through a Hemiplegia, Speech and speech disorder and expresses a sudden occurrence. It is important to act quickly here and initiate what is known as lysis therapy within 4.5 hours after the stroke event. The clot is dissolved with the drug r-TPA. Mechanical elimination of the clot (thrombectomy) is also possible.
Please also read: Stroke - these are the signs
Cerebral sinus and vein thrombosis
These clinical pictures are the occlusion of veins or the venous sinus of the brain by blood clots (thrombi). A distinction is made between two main mechanisms of development, namely the non-infectious and the infectious development. Non-infectious sinus and venous thromboses particularly affect women in the puerperium. Other causes include cancer, the use of hormonal contraceptives, underlying haematological diseases such as polycythemia vera and coagulation disorders (APC resistance, factor 5 disease, etc.). Infectious thromboses arise, for example, from the spread of a middle ear or sinus infection. Other infections in the facial area can also be carried into the cerebral vessels and cause thrombosis there. The symptoms can be similar to those of a stroke, but usually creep in over a certain period of time. However, the beginning can also be sudden. Typical are nausea, vomiting, headache, double vision, hemiplegia and drowsiness. Around 40% of those affected even suffer epileptic seizures. Imaging methods such as CT or MRI are used to confirm the diagnosis. The main focus of therapy is the stabilization of the patient and the immediate heparinization of the blood. The heparin makes the blood more or less “more fluid” and means that the brain is better supplied with blood again. Local thrombolysis (dissolution of the blood clot) can also be considered. In the case of infectious causes, antibiotics or surgical removal of the focus of the infection are used.
Read about this too Blood clots in the head
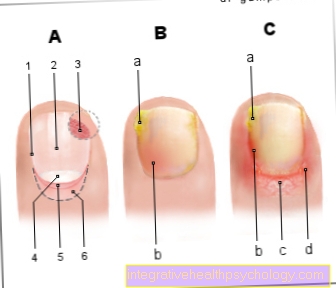
Blood clots in the eye
A distinction is made between vascular occlusions in the eye according to whether a vein or an artery is blocked. The most important blockages caused by blood clots are briefly discussed below.
Artery occlusion in the eye
The arterial occlusion in the eye is usually caused by the Carry-out of a blood clot from the heart (e.g. with atrial fibrillation) or through Inflammation. He is characterized by a sudden unilateral blindness of the affected eyee. The patient has no pain. The central artery or its smaller branches can be affected.
Please also read: Stroke in the eye
Vein occlusion in the eye

Vein occlusions in the eye usually develop more slowly than arterial occlusions. Chronic processes in particular are involved in the formation of the blood clot. The clot typically forms in the vein itself and is not carried away from any other part of the body. Risk factors for the formation of such clots in the eye veins are high blood pressure, diabetes mellitus, arteriosclerosis or diseases of the eye such as glaucoma or the retinal vasculitis (Inflammation of the blood vessels in the retina). The vein occlusion in the eye can sometimes be completely asymptomatic.
Please also read: Thrombosis in the eye
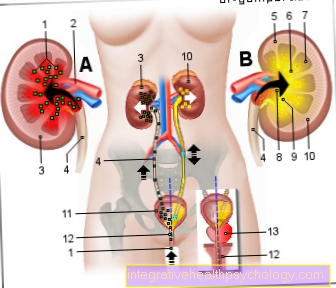
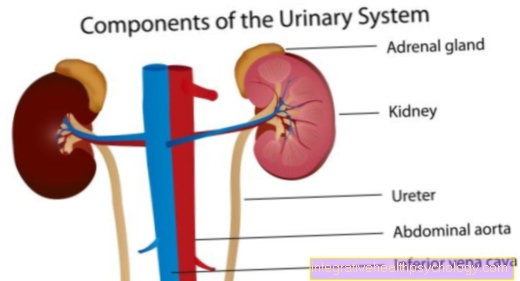
Blood clots in the lungs
Blood clots can cause life-threatening pulmonary embolism in the lungs. In a pulmonary embolism, a pulmonary artery is blocked. There are different ways in which pulmonary embolism can develop. The most frequent root cause is the embolism after Venous thrombosis. Most often, the blood clot (thrombus) comes from the deep leg and pelvic veins and enters the lungs via the inferior vena cava. People with phlebothrombosis (thrombosis of the deep leg veins) are particularly at risk. Less common A blood clot can also enter the lungs through the superior vena cava. This can typically happen during a hospital stay where the patient has a Central vein access receives. A pulmonary embolism is typical acute onset. Those affected breathe very quickly ("Tachypnea") and have trouble breathing ("Dyspnea"). Besides, it can too Breath-dependent chest pain, (Blood) cough, fever and one rapid pulse come. A Jugular vein congestion and a Drop in blood pressure can also show up. The treatment of pulmonary embolism follows strict schemes that differ mainly in whether the patient is in a life-threatening condition or in a stable patient. Pulmonary embolism is usually an acutely life-threatening condition in which those affected cannot do much. It is advisable to lie down with your chest raised and remain calm until the emergency services arrive.
Please also read: Pulmonary Embolism - These are the symptoms
Blood clots in the heart
Blood clots can also have serious consequences in the heart.On the one hand, they can arise there and be carried to other parts of the body, resulting in vascular occlusions, and on the other hand, the clots can also cause damage directly to the heart.
Coronary artery disease and heart attack
Vascular changes in the context of atherosclerosis (vascular disease) lead to thrombotic vascular occlusions. These clots are sometimes slightly different in their composition than in other parts of the body, but the consequences are the same. Different ground risk factors like diabetes, Smoke, high blood pressure and fat levels too high trigger the Deposits on the vessel walls and the attachment of blood cellsso that ultimately clots form. These clots can cause the typical Angina pectoris-Complaints like chest tightness and shortness of breath in the context of a coronary heart disease, on the other hand also a acute vascular occlusion and with it a perfect one Heart attack arise. For both clinical pictures there are complex therapy schemes which, in addition to acute measures, also provide for a reduction in risk factors, such as weight reduction and a smoking ban, as well as anticoagulant medication.
Please also read: Causes of a heart attack and Coronary heart disease (CHD)
Blood clots that are dragged out of the heart
With cardiac arrhythmias, the heart sometimes beats very irregularly or quickly. That can lead to the Blood flows turbulently and more clots form. In the heart, atrial fibrillation in particular poses a major risk for the formation of such blood clots. This clot can through the large vessels carried off into the brain and so lead to strokes. Furthermore, the kidneys and the spleen are at risk of suffering from heart attacks. Hence it is absolutely necessary that People with atrial fibrillation a permanent anticoagulation ("Anticoagulation") of the blood. Typically, the patients receive Marcumar®, which contains the active ingredient phenprocoumon. This medication is given as a tablet.
Blood clot in the leg
Venous thrombosis
Leg vein thrombosis is a relatively common condition that affects many people. It comes to Closure of the deep leg veins by the formation of a blood clot. There are a variety of Risk factors, such as that Smoke, long bed rest or congenital coagulation disordersthat lead to the vascular occlusion in the leg. Those affected complain about one Swelling and overheating as well as one dull pain of the leg. One complication of deep vein thrombosis is the The blood clot is carried into the lungs. This is known as Pulmonary embolism. Patients will be with Compression stockings and anticoagulant drugs treated like heparin and Marcumar®.
Please also read our topic on this Thrombosis in the leg
Phlebitis
In contrast to phlebothrombosis, thrombophlebitis affects the superficial veins of the legs. These become inflamed by blood clots located on the surface. Typically the The vein hardens under the skin, palpable and tender. In acute treatment, it helps to elevate the leg and cool it. Also be Compression bandages created. In order to achieve immediate freedom from pain, the clot can also be removed ("ThrombectomyIf the clot is very large or has a connection to the deep venous system, treatment with anticoagulant medication may be necessary here as well.
Word origin
The medical term for blood clots is thrombus. It is derived from the Greek and means something like "lump" or "plug" (plural thrombi; from Greek thrómbos, "lump, plug"; coagulum)