Nosocomial infection
definition
Nosocomial comes from the Greek "nosos" = illness and "komein" = to care for. Nosocomial infection is an infectious disease that occurs during or after a stay in a hospital or other inpatient medical facility.
These facilities also include nursing homes and old people's homes. One speaks of a nosocomial infection if the disease 48 hours at the earliest or occurs later after admission to the respective medical facility. Any infection that occurs before that is called a outpatient referred to, or may not be safely classified as nosocomial.

root cause
The characteristic of nosocomial infections is that one different germ spectrum than with conventional outpatient germs. So the main cause is staying in a place that has these germs in increased numbers or that encourages them to strengthen. The increased use of antibiotics in hospitals has resulted in many strains of bacteria Resistance to antibiotics could develop.
If a germ develops a mechanism of resistance to one or more antibiotics, a stronger antibiotic must be used. Other “neighboring” bacteria also notice this, so to speak, and can then develop resistance under certain circumstances. It is now also known that many pathogens develop resistance through the use of antibiotics in animals in industrial, factory farming. The resistance of the MRSA.
Pathogen
The causative agents of nosocomial infections are often bacteria that naturally colonize the body in a certain fixed population and are in principle not actually harmful. They only become harmful when they migrate away from their original body location or are carried away, e.g. if a stool germ gets into a skin wound on the lower abdomen or arm. If the patient has a severely weakened immune system (for example after organ transplantation or bone marrow transplantation), this increases the susceptibility to infection.
These patients are given drugs that are supposed to stop the reactions of their own immune system. Certain chemotherapy treatments can also prevent the bone marrow from producing enough immune cells. If a body has been exposed to increased stress (serious illnesses, operations), the immune system is strained and “busy” anyway and may not be able to fight off other germs sufficiently.
Read more on the topic: Chemotherapy side effects
A distinction can be made between two large groups of germs: puddle and airborne germs.
Wet or puddle germs include: Pseudomonas, Legionella, E. coli, Proteus, Enterobacter and anaerobes. They are called puddle germs because they are transmitted through “wet paths” in the hospital. They can be found in wash basins, breathing hoses, inhalation devices, cleaning agents that have been diluted too much, and rarely even in weak disinfectants.
The dry or airborne germs are: S. epidermidis (coagulase negative) and Staphylococcus aureus (coagulase positive), Enterococcus spp., Candida spp., Mycobacteria. They are transmitted differently, namely via medical staff, not wearing protective clothing, via contaminated contact surfaces (such as duvets, medical devices, bedside tables), room air, but above all through insufficient hand disinfection (most common transmission route!).
Another problem group are the germs of the multi-resistant pathogens, which can no longer be killed by several antibiotics. The exact development of resistances is a complex and not yet fully understood process. However, there are certain risk factors that favor the development of multi-resistance. If a patient is in the hospital or nursing home for more than 4 days or has a long hospital stay, the risk increases compared to a patient who only has a short stay in the hospital.
If a patient is ventilated with a breathing tube for more than 4-6 days, the risk of an infection with multi-resistant germs also increases. The air we breathe is humid and thus encourages the penetration of the "puddle germs" and requires thorough hygienic care.
Open skin wounds are an equally endangered entry point. It is now also known that antibiotic therapies that are too short or therapies with the wrong antibiotic promote the development of resistance. Patients who are particularly at risk for dry germs chronic lung disease to have. The lungs are equipped with their own defenses, which are weakened in the case of permanent or structural diseases.
The best-known of the multi-resistant pathogens is above all MRSA, as it is reported about in the media more often. It is a germ called Staphylococcus aureuswhich colonizes every human being as a skin germ and only becomes dangerous if, for example, it colonizes wounds or develops resistance.
The M in MRSA stands for the antibiotic Methicillin, but could just as well stand for “multi”, because it is usually resistant to many antibiotics. The show more multi-resistances VRE (Vancomycin-resistant enterococci). These are intestinal germs that are resistant to the antibiotic vancomycin. The group of ESBL (expected spectrum beta lactamase) are germs that form a certain enzyme, the beta lactamase, that for example the group of Penicillins overrides.
However, drugs have been developed specifically against this, which inhibit this mechanism again and are partly used. therefore easy to control. The is particularly feared among medical professionals Pseudomonas aeruginosa, as it can cause serious illnesses and develops increasingly more resistance.
The germs mentioned can rarely be treated with antibiotics. In medical laboratories, certain tests can be used to find out which antibiotics the respective germ is still sensitive to, and these can then be used as therapy if necessary.
How many nosocomial infections are there in Germany and how many deaths do they cause?
Getting an exact number is difficult because it exists no reporting requirement for nosocomial infections. Some are also overlooked or incorrectly classified as “outpatient infections”. Very rarely there are cases in which a "perfectly healthy" patient suddenly dies of a nosocomial infection. Nosocomial infection is in most cases a complication and not the main cause responsible for the death of the patient.
In 2006 the Robert Koch Institute set up several large studies to determine how many nosocomial infections there are each year. The results after counting and estimating showed the following data: A total of 400,000-600,000 nosocomial infections per year are assumed, of which 14,000 are due to MRSA. Around 10,000-15,000 patients died of hospital-acquired infections.
Scientists estimate the current numbers higher, but these vague estimates are not reliable. For example, a study from 2016, in which the Robert Koch Institute was involved, shows an estimate of 90,000 deaths that can be attributed to nosocomial infections. Depending on the criteria according to which such a study is structured, the numbers come out more or less.
The most important thing here is that early on recommendations regarding the avoidance of nosocomial infections have been declared by the Robert Koch Institute as a consequence and are regularly updated
Which hospital-acquired infection is the most common?
The most common pathogens are Escherichia coli, Staphylococcus aureus, Clostridium difficile, Enterococcus faecalis and Enterococcus faecium. A study by the Robert Koch Institute from 2012 showed the following: The most common nosocomial diseases are (in descending order) wound infections (24.7%), urinary tract infections (22.4%) and pneumonia and respiratory infections (21.5%) %).
How can you avoid nosocomial infection?
In principle, nosocomial infections can be avoided by trying to cure the disease that promotes them or treat them as well as possible. Hygiene measures and a critical assessment of when and which medical measures should be taken can shorten hospital stays and make nosocomial infections preventable.
In the nosocomial pneumonia (Pneumonia) professional hand and device disinfection (e.g. of inhalation devices) should be carried out. Inhalation of gastric juice, saliva or food should be prevented. This can be done by sucking off the secretion with special probes and timely intubation (i.e. inserting a ventilation tube) in the event of swallowing disorders. With the help of occupational and physiotherapy, training can also be carried out with which correct swallowing can be (re) learned, or that eases coughing up from the lungs.
Nosocomial urinary tract infections can be avoided by not inserting an indwelling catheter. There are also special hygiene regulations with regard to the installation and replacement of indwelling catheters. Nursing staff should use closed urinary drainage systems with a non-return valve and a puncture-enabled collection system. If a urinary tract infection is suspected, a small urine sample can be taken cleanly so that therapy can be initiated at an early stage.
A urine bag should always be positioned so that it is below the level of the urinary bladder, so that the urine cannot simply flow back. At best, the laxative tube should not be in loops, so that no urine can collect in the tube, which encourages bacteria to multiply. An indwelling catheter is not an optimal solution for patients who are supposed to have a catheter for more than 3 days.
A so-called one would be better suprapubic Catheter that goes straight through the Abdominal wall leads into the urinary bladder. Sometimes, however, it cannot be foreseen in everyday hospital life whether a patient will need a catheter for longer than 3 days. Efforts are also made to be able to discharge the patient without a catheter rather than to make him dependent on the catheter. Therefore, unfortunately, too many indwelling catheters are often used in everyday clinical practice.
At nosocomial wound infections wound hygiene plays a major role. Patients should not remove or change bandages themselves if wounds are still open (i.e. not healed). When applying plasters and bandages, strict rules and sequences apply, which nursing and medical staff learn at an early stage and usually adhere to. A far greater risk of poor wound healing are risk factors such as old age and diseases, such as Diabetes mellitus. A weakened immune system also plays an essential role here.
The affected part of the body (e.g. the leg) should be raised and only changed by trained personnel. Patients can themselves ensure that weeping bandages are changed immediately. Wetness here refers to excessive wound secretion. In the case of purulent inclusions, the pus should be able to drain through incisions. You can also pull the pus or excess wound secretion out of the wound by applying a so-called lavage or drainage. The process of wound healing can also be checked precisely because the amount of fluid collected is recorded.
To rinse and clean a wound, antiseptic solutions like Octenisept will use. At sign one Blood poisoning antibiotic therapy that affects the entire body system can be used.
Furthermore, visitors and patients themselves can contribute to improved hygiene measures by using the hand disinfection, which is available at every hospital and ward entrance. Exact instructions for correct hand disinfection can now also be found on the toilets. Some hospitals have now also introduced a ban on shaking hands.
A few clinics have meanwhile also started to control the changing of clothes by medical personnel using automatic laundry pick-up and drop-off machines. There are also hospitals in which doctors are no longer allowed to wear the coat-like smock, but instead wear short-sleeved kasaks.
consequences
The consequences of a nosocomial infection can be varied. For example, a nosocomial pneumonia lead to death. A nosocomial urinary tract infection, on the other hand, (like cystitis) can be quite harmless.
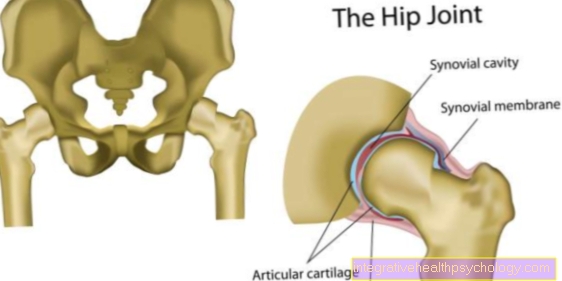
In the case of wound infections, it all depends on which part of the body is affected, how large the wound is and in what general condition the affected patient is. Wound healing disorders can result, e.g. when using a prosthesis (“new hip”) it may even be necessary to remove the prosthesis.
In principle, any bacterial infection that is not treated with antibiotics, inadequately treated or treated with the wrong antibiotic can lead to blood poisoning. Blood poisoning is a dangerous and serious disease that can also lead to death.