Symptoms of gingivitis
introduction
Symptoms can vary depending on the patient. Not every inflammation always has to bring about the same problems. Also important is the difference in how the gingivitis came about. Depending on this, the course of this inflammation also changes. Thus, some patients develop some symptoms over time, while others do not. The general state of health also influences which symptoms occur and, above all, how severe they are. A good example is pain. Some patients do not notice this inflammation for a long time because it does not hurt at first and is thus dragged on. Other patients are more sensitive and feel every little change in the mouth area.
Read more on the subject at: Inflammation of the gums

Symptoms
- Bleeding gums spontaneously, when touched or when brushing your teeth
- Gums come off the tooth
- soft gums
- reddened gums
- swollen gums
- Color change from pale pink to red
- Gums seem to have increased in size
- Feeling of pressure and / or tension in the affected area
- lots of plaque above the gumline
- harmonious and symmetrical course of the gingival margin no longer recognizable
- Tartar
- sensitive tooth necks and teeth
- Change in tooth position due to swollen gingiva
- seemingly loosened teeth
- Teeth become longer
- Symptoms of Acute Necrotizing Ulcerative Gingivitis (ANUG)
- pus
- acute fever
- Powerlessness
- Pain
- Bad breath
Pain
Pain is a protective function of the body and leads to a immobilization of the painful part of the body. The pain signal is generated by certain messenger substances that are produced by immune cells. Pain while chewing can also occur if the teeth are subjected to excessive stress. The inflamed gums are compressed and stretched. It can also lead to referred pain in the jaw joint and ear. Headaches are also common.
Read more on the subject at: Pain associated with inflammation of the gums
Functional impairment is a sign of inflammation. The muscles of the temporomandibular joint are shut down. Sometimes it also tenses up when trying to use it. Since one of the head muscles belongs to the mouth closers, tension can also lead to headaches. Due to a connection between the oral cavity and the middle ear, inflammation of the gums can also spread to there, so that it comes to an otitis media.
Read more on the subject at: Pain associated with inflammation of the gums
pus
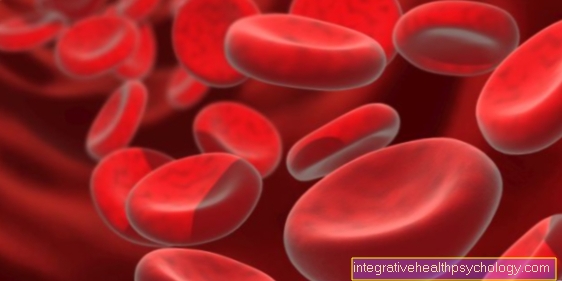
Pus only forms when there is severe inflammation associated with bacteria. A side effect of pus is bad breath. If this does not go away despite brushing your teeth, you should seek the advice of a dentist. The focus of inflammation is usually noticed for the first time through the bad breath or a feeling of pressure. The purulent area should never be touched or squeezed with bare fingers. The risk that bacteria get into the blood and then spread is too great. There is a risk of bacteremia, which is bacteria in the blood, which is a risk for those with heart problems.
A differential diagnosis that pus is leaking on the gums is that the tooth has died from tooth decay. This diagnosis is confirmed if there is no pain in the tooth in question. The nerve is already dead and no longer feels anything. The pus could also come from an abscess on the tooth. An abscess itself is a collection of pus in a cavity, such as the gingival pocket or at the tip of the root. However, as soon as you notice the pus, you should see a dentist as soon as possible. The inflammation could spread to surrounding soft tissues or even the bones if left untreated. Cold helps against pain. The cold shouldn't get directly onto the tooth, but a damp, cold cloth on the cheek will help.
Read more on the subject at: Inflammation of the gums with pus
fever
Fever is seldom seen with mild gingivitis. The same applies to periodontal disease. The reason for this is that these two diseases are chronic. Every now and then, severe periodontitis can lead to spurts of pus. The temperature of the body can be slightly increased. Fever is more commonly observed in association with acute necrotizing ulcerative gingivitis (ANUG). Some areas of the gums die spontaneously. In addition, there is pus with bacteria that destroy the gums. Since the ANUG often runs very quickly, the body has no chance to fight it. The pain makes it difficult to eat. In such cases, only antipyretic antibiotics and painkillers help. Conversely, it is also possible that after an illness, for example angina, which was accompanied by a fever, inflammation of the gums may occur. This is because the body was weakened and used its strength to treat the sore throat.
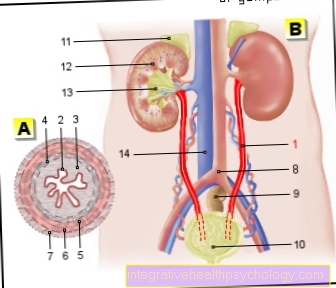
Swollen lymph nodes on the neck
The system of lymphatics and lymph nodes is built up in such a way that the lymph collects in ever larger vessels and runs into one main vessel. The collecting vessels of the head area lie on the neck. This means that these lymph nodes collect all waste products and pathogens and fight them. In response to the work involved in fighting the pathogens, the lymph nodes swell. The lymph nodes on the lower jaw are particularly affected by inflammation of the oral mucosa.
Read more on the subject at: Lymph node swelling in the neck
Swelling of the lining of the mouth
A sign of inflammation is the tumor, i.e. the swelling. This occurs because the blood vessels let more blood cells, such as red blood cells or immune cells, pass through their walls. This phenomenon is triggered by certain messenger substances. This permeability is also promoted by pressure in the vessels (for example high blood pressure) or by minor injuries (for example also in diabetics). The gums can also be swollen, because gum inflammation often results in gum growths that look very swollen and some of them are. The swelling that is triggered by bacteria and causes inflammation is to be distinguished from an allergy, which also causes the oral mucosa to swell, or a swelling caused by Candida, a yeast that weakens the immune system.
Read more on the subject at: Swelling in the mouth
Gingival pocket
The gingival pockets or pseudo-pockets that form between the tooth and the gum tissue are created when the tissue is destroyed by the inflammation. On the one hand, the gums are stretched by the swelling and no longer lie close to the tooth. On the other hand, the bacteria that are in the dental plaque migrate deeper and further towards the tip of the root. These bacteria destroy the fibers that hold the teeth in place in the tooth socket, creating space between the tooth and the gums. If this soft plaque becomes tartar, it is much easier for a pocket to be formed because the tartar keeps the soft tissues from the tooth. Often the depth of the pocket cannot be determined with the probe because solid tartar gives an incorrect reading.
Read more on the subject at: Gingival pockets
Periodontal disease
Periodontal disease is the slang term for periodontal disease. Periodontitis does not develop overnight. It is always preceded by marginal gingivitis.Marginally because the gingivitis only stretches along the free gums, other tooth supporting structures are not affected. The disease is fluid, unless the inflammation of the gums is stopped. The tooth holding apparatus also includes the fiber apparatus, on which the teeth are suspended in the tooth socket, and the jawbone, which gives the tooth stability and the gums a shape. If the fibers are affected by the inflammation, tooth loosening occurs. The likelihood of losing the tooth is greater. It is also possible that the tooth shifts because the opposing tooth is loading it incorrectly and the neighboring teeth are no longer stable enough to hold it in place.
A bigger problem is that the bacteria migrate to the bone and demineralize it. They remove substances from the bones that give it strength and stability. The bone is gradually broken down. As a result, the tooth is even less stable. An advanced inflammation of the periodontium can establish itself so that it is not reversible. Since the blood circulation in the gums is increased and there are many bacteria in this area, the risk of bacteria spreading is very high. This is a problem in that it affects the heart, especially in patients with cardiovascular disease. Complications from periodontal disease have also been noted in diabetic patients and pregnant women.
Read more on the subject at: Periodontosis and Periodontitis
Inflammation of the gums without pain
Pain is a subjectively felt feeling. This means that each patient experiences feelings as painful in different ways. Some people are very sensitive to pain and feel every little change. Others are insensitive to pain and can withstand a lot of hardship. This is due to the different hormone levels. Many typical symptoms occur without pain, which is a problem because the inflammation is not recognized for a long time. The reddening of the gums is not painful at first. Likewise, some swelling is not accompanied by pain. Occurring bad breath is usually not noticed.
A noticeable sign is bleeding gums when brushing your teeth. In its early stages, bleeding is not itself painful. Of course, the bristles can hurt if you apply too much pressure. The presence of bacteria in the form of plaque deposits or even tartar does not hurt in any way. Rather, it forms a protective layer that protects the tooth enamel from the cold and heat.
Evidence of HIV infection
Inflammation of the gums with bleeding gums can be a side symptom of an infection. This disease is favored by the fact that the immune system is weakened and is unable to fight the bacteria that constantly appear in the mouth. 44% of all patients experience swallowing pain and a sore throat, so the diet could be the wrong one. Another symptom is mouth ulcers. However, these do not form in the entire mouth, but are more like spots. It is important that not every inflammation of the gums allows conclusions to be drawn about an HIV infection.
Read more on the subject at: Symptoms of AIDS