Root inflammation
Synonyms in the broader sense
Root inflammation, pulpitis, apical periodontitis
introduction
In the case of tooth root inflammation, the tip of the root is often inflamed. For this reason, one speaks of an "apical periodontitis. A tooth root inflammation can, among other things Caries bacteria, one Fall or by that Grinding of the tooth for e.g. a crown emerge.

If the tooth is too badly affected by one of these influences, the body reacts with an inflammation of the tooth root, more precisely the inner workings of the tooth, i.e. the tissue that supplies the tooth with nutrients and gives it feeling.
Root canal treatment can help preserve the damaged tooth.
Symptoms- an overview
The root inflammation that occurs as a result of periodontitis (inflammation of the periodontium) can show itself through:
- Pain especially when touched, tenderness to knock
- Pain radiating to the face and jaw
- Pain when chewing, brushing teeth
- Tenderness
- Gingival pockets
- reddened gums
- possibly emerging pus
- a "big cheek"
- fever
- Toothpicking
Depending on the extent of the destruction of the tooth bed, loosening occurs.
Read more on the topic: Symptoms of tooth root inflammation
Pain in a tooth root inflammation
A tooth root inflammation can lead to severe discomfort and unpleasant pain. Exercise and exercise can increase this uncomfortable feeling. In the majority of those affected, pressure builds up as the abscess tries to spread and displaces the tissue. The increased blood flow during sport can cause this pressure to expand and become stronger. Furthermore, stressful situations can also have a negative effect on the pain, since the stress hormone cortisol leads to a stronger pain perception.
Read more on the topic: Abscess on the tooth
The pain can go from a feeling of pressure to a throbbing, throbbing pain. As soon as this state is reached, a doctor should be consulted as soon as possible in order to prevent systemic diseases from developing. The pain can radiate to other areas due to the central location and also lead to severe headaches or pain in the sinuses. Patients also report pain due to restricted movement of the head or neck. Simply turning the head can lead to discomfort.
Read more on the topic: Pain in a tooth root inflammation
Root inflammation with pus formation
If a purulent abscess with swelling has already developed due to the tooth root inflammation, physical exertion is not advisable. An abscess describes a pus-filled, encapsulated cavity. The body is already severely weakened by the infection and further physical exertion with additional weakening of the body can create a free gate for the bacteria to get into the bloodstream. The bacteria can not only lead to long-term cardiovascular diseases.
Read more on the topic: abscess
Acutely, the pus cells can pass through the bloodstream and lead to sepsis, blood poisoning. This disease is acutely life-threatening and only 50% of all sepsis diseases survive this acute condition. The bacteria reach all organs through the bloodstream and begin to attack them systematically and simultaneously. Therefore, in the case of a purulent abscess, the dentist or the emergency room should be visited and then physical rest should be ordered so that the body can regenerate.
Read more on the topic: Purulent tooth root inflammation
Dead tooth
As soon as the caries-causing bacteria have reached the pulp and the nerve fibers embedded in it, a strong inflammatory process is triggered.
The inflammation damages the nerve fibers and causes severe pain.
In some cases, the bacteria mentioned above have another portal of entry:
- You can also advance to the root of the tooth from deep gum pockets. These deep gum pockets arise in the course of a disease of the teeth supporting system known as periodontal disease. The gums (gingiva) are irritated by plaque deposits (biofilm consisting of food residues and waste products of the bacterial metabolism), which proceed from the neck of the tooth, along the tooth root, into the depth. As a result, the first thing to do is inflammation of the gums (gingivitis), which leads to the well-known bleeding gums.
As the disease progresses, foci of inflammation develop around the tooth root, which spread towards the tip of the root and ultimately pass over to the jawbone.
Despite this second port of entry, an untreated carious tooth defect is the main cause of a tooth root inflammation to this day. Since the main reason for the development of caries and / or periodontal disease is inadequate or inadequate oral hygiene, an inflammation of the tooth root is also triggered to a certain extent by a lack of dental care.
Read more on the topic: Dead tooth
Note
Ultimately, a tooth root always leads to damage to the nerve fibers and blood vessels within the tooth pulp and the tooth root.
However, since every tooth is dependent on the supply of blood and nerve impulses, a tooth whose pulp has been attacked by inflammatory processes will “die off”.
A so-called "dead tooth" is created. This means that the tooth still remains in the jaw and can also be used for chewing for the time being, but is not supplied with nutrients, oxygen or the like.
As a result, the hard tooth substance sooner or later becomes brittle and the tooth breaks under stress (for example when biting hard).
A dead tooth must be treated in any case, otherwise there is a risk
- of Tooth loss or
- of the Spread of inflammation to other tissues; The spread of the inflammatory processes to the eye socket, the eye and the neck region is particularly dangerous
Often the inflammatory processes attack the tooth root skin after attacking the tooth root and root tip (tooth root inflammation) and then go to the Jawbone over. A further expansion can then result in a abscess and / or open into a fistula.
A dead tooth can remain in the jaw for a long time. This is because a tooth has no vital (functional) nerve fibers no longer causes pain.
Furthermore, the tooth enamel and dentin can survive for a long time without the supply of nutrients from the blood.
One recognizes a dead tooth aovert dark discoloration, parts of the hard tooth substance can also break off.
Inflammation of the root of the tooth
It is not the root of the tooth that is inflamed, but rather the tissue surrounding it, called the periodontium, that becomes inflamed. Untreated periodontitis penetrates deeper and deeper towards the tip of the tooth root with its destruction of the tooth support apparatus and causes inflammation of the surrounding tissue. If the periodontal membrane is inflamed as a result of bacterial influences and the tooth holding apparatus is destroyed, toothache occurs and the tooth becomes loose.
Read more on the topic: Periodontal disease
Such an inflammation can be present in both living and market-dead teeth. Every touch, both horizontally and vertically, creates pain. Bacteria can also get into the entire organism from this source of inflammation and cause infections there.
Read more on the topic: Pain at the root of the tooth
A tooth root inflammation just at the tip of the root (Apical ostitis) can be painless for a long time. It only occurs in a tooth whose pulp has died and which has not received a root canal treatment. But teeth with a root filling can also get inflammation at the root tip. Unfortunately, the end of the root canal is branched like a delta and therefore cannot be covered with the root filling up to all branches.
As a result, bacteria can still remain in these corners. Antibacterial root fillings provide some protection, but not in all cases. The result is an escape of the bacteria into the bones and a reaction from the body. A chronic focus of pus forms, which is shielded by the body's own defenses with a connective tissue wall. The bacteria keep multiplying and the hearth expands. This leads to tooth root inflammation and breakdown of the bone. Bacteria can get into the bloodstream from this source and affect other organs, primarily the heart.
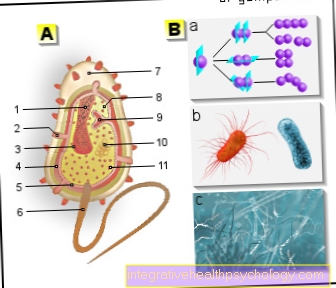
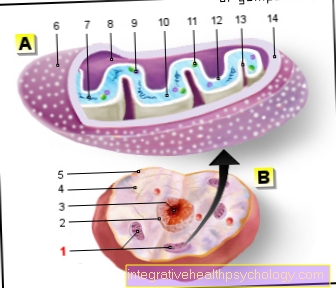
Figure root inflammation

- Tooth enamel -
Enamelum - Dentin (= dentine) -
Dentinum - Tooth pulp in the tooth cavity -
Pulp dentis in Cavitas dentis - Gums -
Gingiva - Cement -
Cementum - Root skin -
Periodontium - Alveolar bone (tooth-bearing
Part of the jawbone) -
Pars alveolaris - Opening of the tooth root tip -
Foramen apicale dentis - Blood vessels
- Nerve fibers
Root inflammation -
Pulpitis
a - dental caries -
Caries dentium
b - gingivitis -
Gingivitis
c - Entz. of the tooth support system -
Periodontal disease
d - Entz. at the root tip -
Apical ostitis
You can find an overview of all Dr-Gumpert images at: medical illustrations
Treatment of root inflammation
The only way to get a root infected tooth is to have one
- Root canal treatment
- and possibly a root resection.
Read more on the topic: Treatment of root inflammation
Root canal treatment
The most common treatment method is root canal treatment with subsequent root canal filling.
In advance, the dentist will take an X-ray of the affected tooth and carry out a so-called vitality test.
During the vitality test, the tooth is exposed to a cold stimulus and it is checked whether the patient feels this cold in general, whether there is pain or whether the stimulus no longer triggers any reaction. If the tooth is dead, the vitality test will be negative.
During the root canal treatment, the affected tooth is “drilled open” and the pulp and nerve fibers are removed with the help of differently thick root files (Reamer, Hedström or K files).
In this way, the dentist removes the inflamed tissue and tries to fix the tooth root inflammation.
This is followed by an alternating rinse with different solutions.
The solutions used are hydrogen peroxide (H2O2), anti-inflammatory, antibacterial chlorhexidine (CHX) and sodium hypochlorite.
In many cases, it is possible to immediately fill a root canal with a tooth that was already dead before the start of treatment.
However, if the inflammation is very advanced, the dentist will probably first insert a medication into the root canals and let the tooth rest for a few days.
In a separate session (approx. 3 - 5 days later) the drying and filling of the tooth roots begins.
As soon as the tooth roots are germ-free and dry, they are filled with so-called guttapercha points and a density cement. The gutta-percha points are made of rubber-like material that should fill the hollow tooth roots and seal them tightly.
As a rule, an X-ray control image is used to check whether the root is filled to the tip (apex) and the tooth is then closed.
Read more on the topic: Treatment of root inflammation
Apical resection
Sometimes, however, such a root canal treatment is not enough to rid the diseased tooth of the inflammation. The dentist then has the option of performing a tip resection. In a root tip resection (apectomy), the tip of an inflamed tooth is removed.
The prospect of saving the tooth in this way is included 90 – 97%.
During the operation, the gums in the area of the diseased tooth are first opened and then the jawbone is opened with the help of a so-called ball burr (osteotomy).
This gives the doctor a good overview of the tissue to be treated and can cut off and remove the inflamed tooth root tip.
A so-called retrograde root filling is then carried out. Retrograde means that the root canals are not filled starting from the tooth crown, as is usual. The gutta-percha points are introduced starting from the severed root tip. This has the advantage that the root filling begins exactly at the end of the tooth roots.
Then the gums are sutured with about 2 - 3 stitches.
The nerves can be damaged during a surgical root tip resection, which manifests itself in the patient's loss of sensitivity in the area of the lip (numbness). In addition, as with any operation, bleeding and / or wound healing disorders can occur.
The patient is therefore urgently advised to refrain from consuming alcohol and nicotine after the operation, as alcohol can also cause toothache.
Read about this: Toothache after consuming alcohol
Home remedies
Home remedies such as clove oil or rosemary leaves cannot reach the source of inflammation as rinses. They only soothe the inflamed gums. Therefore, home remedies should never be used as the sole therapy for treating tooth root inflammation, as they will not correct the problem. In general, the use of home remedies should be discussed with the dentist.
Cool
In general, cooling always helps with swelling if a few rules are followed. It is advisable to use a cooling compress that is wrapped in a towel. This cooling compress can then be held on the affected area. It is important that this cooling process lasts a maximum of 10 minutes and then a period of at least one hour is observed until the next time it is cooled. This is particularly important, as long-term cooling is harmful. The permanent cooling causes the blood vessels to contract and the area is poorly supplied with blood.
At this point, the body senses the state of freezing and takes action against it. The blood pressure and heart rate rise and the affected area warms up again. This, in turn, is the perfect environment for bacteria, as they multiply particularly quickly and in many different ways when it is warm, and the inflammation spreads even faster. With targeted cooling, this does not happen and the swelling spreads more slowly because the bacteria do not prefer cold. However, this can only buy time, the abscess does not regress through pure cooling.
Remove tooth
In most cases, the abscess that has arisen from a tooth root inflammation originates in a tooth. If the pus in the swelling has been drained by a dentist through a relief incision, the tooth must also be removed. (Tooth extraction) The nerve within the tooth has died and, due to the massive inflammation, it can usually not be saved with a root canal treatment. The bacteria have started to metabolize the nerves and the surrounding bone tissue and the tooth is no longer well anchored in its original bone compartment.
He has loosened up. Once the tooth has been removed, after the wound has healed completely (approx. 2-3 weeks), you can plan how and in what form the gap between the teeth will be closed. When planning implants, it is often necessary to wait 6 - 12 weeks after extraction until the bone has completely regenerated; this can be done more quickly with a bridge restoration, as only complete soft tissue regeneration is required here.
Read more on the topic: Tooth extraction
Administration of antibiotics in the case of a tooth root inflammation with pus formation
In addition to surgical therapy, in which a relief incision is made in the abscess and the tooth is extracted, the dentist also prescribes an antibiotic. The antibiotic works in such a way that it either destroys the bacteria themselves or prevents them from multiplying and thus achieves that the body is freed from the bacterial load much faster.
According to this spectrum of activity, antibiotics can be divided into a bactericidal or a bacteriostatic group. The bactericides kill and destroy the bacteria, the bacteriostatic ones prevent them from multiplying. It is important that the patient strictly adheres to the antibiotic medication ordered by the dentist and that the preparation is finished so that no resistance can develop. If the intake is not followed at the right time or for long enough, it is possible for bacteria to survive and adapt against this antibiotic.
They form a resistance and the antibiotic no longer works with secondary diseases. As a rule, the penicillin preparation amoxicillin is prescribed, and clindamycin is used for allergies.
Read more on the topic: Antibiotic for tooth root inflammation
Consequences if not treated
If a tooth root inflammation remains untreated or if the affected tissue is not completely removed by the treating dentist, this has further consequences:
- In such cases, the inflammation will most likely spread to and damage the structures surrounding the tooth.
- After attacking the root and apex of the tooth, the inflammatory processes often affect the periodontal membrane and then spread to the jawbone.
- A further expansion can lead to the development of an abscess and / or a gingival fistula.
- In the case of untreated tooth root inflammation, bacteria can enter the body's circulation and infect other organs there, including the heart. There is then a risk of heart valve inflammation. (Endocarditis)
Read more on the topic: Treatment of root inflammation
Causes- an overview
Root inflammation is often caused by:
- untreated deep tooth decay
- untreated gingivitis
- untreated periodontal disease
- deep gum pockets
- Grinding the teeth (rarely)
- Traumas (falls, grinding teeth)
Causes in detail
A tooth root inflammation (pulpitis) is an uncomfortable, extremely painful disease, for which there are several causes:
- This dental disease is primarily triggered by bacteria that migrate from a carious tooth defect via the root.
In some cases, the responsible bacteria also get to the tooth root through deep gum pockets. These deep gum pockets are usually caused by a long-term, untreated inflammation of the gums (gingiva) or in the course of periodontal disease (the inflammatory disease of the periodontal system known as periodontal disease is actually called periodontitis). - Untreated, deep caries is still the most common cause of tooth root inflammation, because the caries attack "works" its way into the depth of the tooth over time and there damages the pulp and the nerve fibers embedded in it.
The bacterial colonization in the depth of the tooth and the resulting inflammatory processes lead to severe pain and progressive death of the tooth.
The exact reasons for these inflammation-related processes have not yet been clarified in detail. However, it is believed that your own immune system plays a major role in its development. - But it is not just the harmful effects of bacterial colonization that are the causes that favor the development of a root tip inflammation.
Such a clinical picture can also arise from traumatic influences. This means that in some cases a tooth, or rather its root, can break through through “acts of violence”, for example by biting too hard, a violent blow on the jaw or severe grinding of teeth.
See also: broken canine tooth - The dental trauma itself is not immediately perceived as such by most patients, as it usually does not cause any pain at first and does not affect the person affected any further. Only in the course of time do foci of inflammation develop in the area surrounding the “broken tooth”, which cause pain and drive the patient into the dental practice.
- In this context, too, inflammatory processes can occur within the tooth pulp, the blood vessels and nerves of the tooth are irritated and / or damaged and, sooner or later, a tooth root inflammation develops.
The grinding and preparation of a tooth in the sense of prosthetic dentistry (supplying with crowns, bridges, inlays ...) can attack the tooth and promote the development of a tooth root inflammation.
Read more on the topic: Causes of a root inflammation
Note
However, as with most dental diseases, the main cause of tooth root inflammation is poor and / or incorrectly performed oral hygiene.
diagnosis
In the inflammation of the tissue surrounding the tooth root caused by periodontitis, the diagnosis of tooth root inflammation is made by probing the depth of the pocket with a periodontal probe.
In addition, an X-ray provides evidence of the extent to which the bone has already been damaged.
The inflammation and the pus focus (Granuloma) at the tip of the root can only be diagnosed on the basis of the X-ray, as long as it is still without symptoms. The abscess is of course obvious and does not require any further diagnostic measures. An abscess describes an encapsulated cavity filled with pus.
prophylaxis
Since the cause of a tooth root inflammation of the tissue surrounding the tooth root is periodontitis, the cause lies in the bacterial plaque. Removal of plaque is the best prophylaxis.
The inflammation at the tip of the tooth root is the result of tooth decay and cleaning the teeth is a prophylactic measure here too. The best prophylaxis for inflammation at the tooth roots is the thorough daily removal of plaque.
A six-month visit to the dentist for professional teeth cleaning is also beneficial for maintaining healthy oral hygiene.
Read more on the topic: Professional tooth cleaning
Root inflammation and exercise
In the case of tooth root inflammation, physical exertion achieved through exercise is not recommended. When the body is exerted, the vessels contract and blood pressure and heart rate rise. The body warms up. This gives the bacteria that trigger the inflammation the perfect environment to multiply and create or quickly enlarge the abscess.
The body is weakened and even more vulnerable through exercising. The immune system hardly has a chance to fight against the infection by the bacteria. There is also the risk that the bacteria will get into the bloodstream more easily and become a systemic problem. The bacteria quickly reach central organs such as the heart and can easily damage the heart by weakening the immune system.
Read more on the topic: Exercise for a root inflammation
The disease myocarditis can develop, in which the heart muscle is attacked by the bacteria and the muscle cells are damaged. This weakens the heart muscle and leads to heart failure. This condition is life-threatening because the heart muscle is no longer as resilient as before and as a consequence there is an increased risk of heart attack and heart medication may have to be taken for life. Therefore, in the case of a tooth root inflammation, you should keep your distance from exercise until the end of sport in order to avoid any serious consequences.
Read more on the topic: Myocarditis
forecast
If the inflammation of the periodontium is not so advanced that it has become loosened, the prognosis and treatment of the root inflammation is good. If it is very loosened, the tooth is lost. After an apicectomy, the tooth can be preserved and therefore the prognosis is very good.
Summary
Inflammations at the root of the tooth affect either the tooth holding apparatus or the jawbone at the tip of the root. They are the result of periodontal disease or tooth decay. Therapy consists of either cleaning the gingival pocket, an extraction or a root resection.