Breast cancer
Synonyms in a broader sense
- Breast cancer
- Mum Ca
- Invasive Ductal Mum Ca
- Invasive Lobular Mum Ca
- inflammatory breast ca
English: breast cancer
Definition of breast cancer
Breast cancer (breast cancer) is a malignant growth (malignant tumor) of the female or male breast.
The cancer can originate either from the ducts of the glands (milk ducts = ductal carcinoma) or from the tissue of the glandular lobules (lobular carcinoma).

Occurrence in the population
Breast cancer (Mamma-Ca) is the most common malignant tumor disease in women.
Every year around 50,000 women develop breast cancer in industrialized countries. In other words, this means that almost every 8th to 10th woman in industrialized countries will develop such a tumor in her life.
The time of the recurrence of breast cancer is usually around the age of 40. Another point in time at which women increasingly develop breast cancer is after the menopause (climacteric). However, young women in their 20s can also develop breast cancer.
Around the age of 40, breast cancer is the leading cause of death for women in industrialized countries.
If one looks at the number of new cases of breast cancer over the course of a few years, one comes to the conclusion that the rate of women who develop breast cancer every year is increasing from year to year (increasing incidence of breast cancer).
In the developing countries, however, it is very different. Breast cancer is a rarity there.
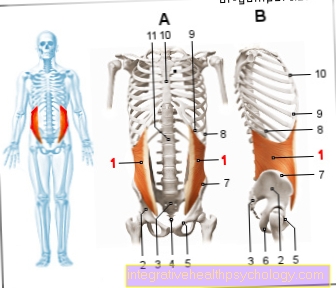
Illustration breast cancer

Breast Cancer - Breast Cancer
(Malignant tumor of the mammary gland)
- Axillary lymph nodes -
Nodi lymphoidei axillares - Lymph vessels -
Vasa lymphatica - Milk duct -
Lactiferous duct - Lobule of the mammary gland -
Lobuli glandulae mammariae - Adipose tissue -
Corpus adiposum mammae - Cancer cell -
Cell with altered genetic material
(Mutated cell) - Nuclear body -
Nucleus - Cell wall
Breast Cancer Symptoms:
a - Enlarged lymph nodes
b - lump in the chest
c - fluid leakage
from the nipple
d - skin dimples in the chest
e - change in color,
Size, shape of the chest
A - ductal carcinoma
(80%) - milk duct cancer, developed
located in the cells of the milk ducts
A1 - Paget's carcinoma -
a ductal carcinoma develops
especially in the nipple tissue
B - Lobular carcinoma
(15%) - lobular cancer,
arises in the mammary gland lobules
You can find an overview of all Dr-Gumpert images at: medical illustrations
Breast cancer of the nipple
Breast cancer of the nipple is also called Paget's disease. This cancer can grow either locally or invasively. In contrast to classic breast cancer, Paget's disease shows some characteristic symptoms. Itching, burning and flaky skin changes on the nipple are typical. There may also be retractions on the nipple or a bloody dissection from the nipple.
In the diagnostic work-up, a small piece of tissue is taken out with a punch and this is examined by the pathologist. Mammography and sonography are also performed. Breast cancer on the nipple is similar to various skin tumors or benign skin changes that can also appear in this area. If possible, the therapy is carried out surgically, followed by systemic therapy.
Read more on the topic: Paget's disease
Causes and Risk Factors
The exact cause of the development of breast cancer is still unknown. In about 5% of all breast cancer patients, however, a connection between breast cancer and a change in a gene was found (autosomal - recessively inherited gene mutation).
More about the causes on: Causes of breast cancer
The change (mutation) in those affected is either on the BRCA-1 gene (Breast approxncer 1 gene = breast cancer gene 1) on chromosomes 17 or the BRAC - 2 gene (Breast approxncer 2 gene = breast cancer - gene 2) on chromosomes 13. If a patient inherits such a change in a gene, he has an increased risk of developing breast cancer.
If you have any further interest in this topic, then read our next article below: BRCA mutation
Other risk factors that can promote the development of breast cancer are
- an early onset of the menstrual period (menarche)
- as well as late onset of menopause (menopause)
- no children (nulliparous)
- Women who gave birth to their first child after the age of 30 (late Primipara)
Ask other risk factors
- Overweight (obesity)
- Ovarian cancer (ovarian cancer)
- Uterine cancer (endometrial cancer)
- Cancer of the colon and rectum (colon cancer / colorectal cancer)
Some benign changes in the breast tissue (connective and / or glandular tissue) (mastopathy grade 2 and 3) can also be an increased risk of breast cancer. Smoking also increases the risk of developing breast cancer.
What are Risk Factors?
When it comes to risk factors, a distinction is made between hormonal, hereditary and other risk factors. When it comes to hormonal risk factors, the longer the active hormonal period, the higher the risk. This means that women with an early onset of menstrual bleeding and late onset of menopause are at increased risk. This is also the case with women with no or few pregnancies, as well as when taking hormonal contraceptives in the last 5 years or hormonal preparations after the menopause.
One of the hereditary risk factors for breast cancer is the mutation in the BRCA gene, the breast cancer gene. However, there are a number of other mutations that are among the risk factors for developing breast cancer. In addition to these two large groups of risk factors, there are other factors that are summarized under other risk factors.
These include, for example, old age, high density of breast tissue, low physical activity, lack of sleep, smoking or type 2 diabetes mellitus. A positive breast cancer history is also one of the risk factors for breast cancer. A positive medical history means an existing breast cancer on one side or another lesion that has not yet degenerated.
Read more about this on our website Breast cancer risk.
What is the breast cancer gene?
The breast cancer gene is a mutation, i.e. a change in the genetic make-up, in the BRCA genes. There are many other genes that are associated with a higher risk of breast cancer, but the BRCA gene is the best studied. The mutation is inherited as an autosomal dominant trait. This means that if one parent is a carrier of the mutation, children have a 50 percent risk of inheriting this mutation and therefore an increased risk of cancer.
People who carry a mutation in this gene have an approx. 60-75 percent lifetime risk of developing breast cancer and, depending on the exact mutation, a 10-60 percent lifetime risk of ovarian cancer. Typical of the breast cancer gene is the early age of onset and time tumors occur more frequently than in the normal population. If a mutation in the BRCA gene is suspected in the family, genetic testing can be carried out. First, a person who is already ill is tested and, if the result is positive, the direct family can be offered genetic testing. The breast cancer gene is also found in a quarter of all men with breast cancer. Because the cancer risk is so increased, all people at risk are included in an intensified early detection program in order to detect any tumor findings as early as possible.
Further information on the subject can be found at: Is Breast Cancer Hereditary?
Age
Age is a risk factor for breast cancer.
The risk of developing breast cancer increases with age, and younger women are rarely affected. The majority of women only develop breast cancer from the age of 40 and especially from the age of 50. Most diseases occur after menopause.
The mean age of onset of breast cancer is 64 years.
All other cancers appear on average only at an older age. The risk of developing breast cancer is further increased if a late growth spurt occurred in adolescence or if the menopause (climacteric with subsequent menopause) occurs late.
Statistically, women who were over 30 years of age when their first child was born are also more at risk of developing breast cancer.
Breast cancer from smoking
Smoking is a major risk factor for breast cancer. Studies have shown that women who smoke have a 17% higher rate of breast cancer. In strong women, this rate is even increased by 21%. It is also interesting that women who smoked more than 5 years before their first pregnancy are particularly at risk. This has to do with the fact that the breast does not fully differentiate until after the first pregnancy and is very vulnerable to harmful influences before that.
Breast cancer from alcohol
The consumption of alcohol is a risk factor for breast cancer or other cancers. Alcohol is probably its most harmful effect if it is consumed daily. Then even small amounts of alcohol (5-15 grams) are enough to have harmful effects on the mammary gland tissue. Hence, abstaining from alcohol is far more effective than simply reducing the dose.
Breast cancer and the pill - is there a connection?
Taking the pill can increase the risk of breast cancer. This is due to the hormones that are contained in the pill. In a more recent study it was shown that the risk of breast cancer can be increased by up to twenty percent if you are currently taking the pill or if you took it up to 5 years ago. The risk increases the longer you take the pill. In absolute terms, this means 13 additional women out of 100,000 who get breast cancer, which can be converted into 0.013%. The increased risk of breast cancer should always be weighed against the benefits that the pill brings with it.
Vitamin D and breast cancer - what is the relationship?
Studies have shown that low vitamin D levels are associated with higher all-cause breast cancer mortality. However, it is not clear whether advanced cancers lead to a lower vitamin D level, i.e. whether it is the consequence of the cancer or the cause of the more severe course. So far, however, it is not recommended to take vitamin D supplements as a lump sum, as the effects of the preparations on the course of the diseases have not yet been sufficiently investigated.
Disease emergence
Breast cancer develops from preliminary stages over several years. Initially normal cells (differentiated cells) change over time, they dedifferentiate, so to speak (undifferentiated cells). They can then usually no longer be controlled by the body's regulatory mechanisms, but continue to grow and change independently. Ultimately, the cancer cells lose their original function.
The preliminary stage (precancerosis) of breast cancer of the excretory ducts (invasive ductal breast carcinoma) is a so-called surface carcinoma of the milk ducts (ductal carcinoma in situ = DCIS). It accounts for 90% of all breast cancer precursors. In this surface carcinoma the cells are already changing, but do not grow into the depths of the tissue in a destructive manner. As the name suggests, surface carcinomas therefore grow superficially. They cross a certain line (basement membrane) that does not separate the superficial cells from the surrounding tissue. The cancer cells of the surface carcinoma also do not settle (metastasize) in other organs. About 20% of these surface carcinomas of the milk ducts occur on both sides and in several places (multiple).
If such a surface carcinoma grows (proliferates) faster than vessels can form which can supply the surface carcinoma with nutrients, some parts of the tumor can die (necrosis). These dead parts can calcify in the further course. These calcifications can be detected in breast cancer tissue using mammography.
Destructive (destructive, invasive) breast cancer that penetrates (infiltrating) the surrounding tissue can develop from these surface carcinomas of the milk ducts, i.e. the preliminary stage of breast cancer of the milk ducts. This usually happens in less than 10 years.
The preliminary stage of breast cancer of the lobules (invasive lobular breast carcinoma) is also a surface carcinoma (lobular carcinoma in situ = LCIS). This does not proliferate in the ducts but in the tissue of the lobules (lobules). Dead tissue is less common than with surface carcinoma of the milk ducts, and therefore calcifications are less common. About 30% of it occurs on both sides and about 60% of it is located (localized) in several places (multicentric). After about 25 years, this preliminary stage will develop into breast cancer of the lobules.
Please also read our pages Breast cancer stages and Breast cancers.
Breast cancer of the milk ducts is the most common type of breast cancer, followed by breast cancer of the lobule. Another rare form of breast cancer is mucinous carcinoma, also called gall disease, which can produce thick mucus. Medullary carcinoma and papillary carcinoma are also other rare forms of breast cancer. Other rare forms are tubular carcinoma, adenoid-cystic carcinoma and comedo carcinoma. The latter is a malignant tumor with dead cells (necrosis) in the middle.
So-called inflammatory breast cancer (inflammatory breast cancer) takes a special form. It accounts for 1-4% of all breast cancers. The name comes from the fact that the breast looks like there is inflammation. The colonization of cancer cells in the lymphatic system (lymphangiosis carcinomatosa) of the skin leads to overheating and reddening (erythema) of the breast. The breast is also swollen. The skin has indentations (orange skin). In the case of a breast with this type of appearance, it must always be clarified whether it is an inflammation or breast cancer.
Please also read our article on this Swelling of the chest.
Paget's carcinoma (Paget's disease of the breast) is a special type of breast cancer. In this type of breast cancer, the lump connects to the nipple (nipple). The nipple is red, flaky, and itchy
What types of breast cancer are there?
There are a number of classifications that structure the different types of breast cancer. For example, you can look at the histology, i.e. the tissue composition, of cancer. A distinction is made here between in situ carcinoma and invasive carcinomas. In situ carcinoma is a non-invasively growing tumor that has not yet crossed the cell boundaries. In this group, histology continues to differentiate ductal from lobular in-situ carcinoma. In the case of invasive carcinomas, the most common carcinomas are "of non special type" (NST), which cannot be assigned to any specific type.
Special forms of breast cancer are inflammatory breast cancer (inflammatory breast cancer) and Paget's disease, an inflammatory tumor of the nipple. Then you can classify the different types of breast cancer according to their receptor status, which is relevant for the therapy decision. The best known is triple negative breast cancer, which has no receptors for antibodies or hormones. All constellations of receptors are divided into different groups and, together with the size and differentiation of the tumor, the therapy is derived from this.
Find out more about the topic: What types of breast cancer are there?
What are the signs of breast cancer?
Breast cancer is usually associated with symptoms only at an advanced stage. The earliest form of DCIS only shows symptoms in around 20% of all women. It is possible that there are indentations on the chest, which can also be reddened. You should always pay attention to asymmetries of the skin and the contour of the breast. These can be a sign of local changes in the breast tissue. One sign that structured cancer screening should detect early on is local hardening of the breast.
They are often blurred, insensitive to pressure and cannot be moved. The most common localization is in the upper and outer areas of the chest and near the armpit. As part of cancer screening, the lymph nodes in the armpit are also palpated, as these may be enlarged to palpate in advanced breast cancer. The displaced growth of breast cancer can cause lymphatic vessels to become blocked and lymphedema to develop. This leads to water retention in the breast and can result in skin changes such as orange peel. If breast cancer is very advanced, it can manifest itself as a drop in performance and weight loss.
Read more on the topic: How do you recognize breast cancer?
How can I recognize breast cancer?
In order to detect breast cancer early, you should scan your own breast regularly.
It is recommended to feel the breasts for lumps and changes about a week after the menstrual period, during this time the breast tissue is very soft and easy to examine. The armpit should also be palpated for swollen lymph nodes. There are several ways to palpate the breast. A gynecologist should be asked about the correct implementation. As a rule, the lumps discovered during self-examination are benign (especially in young women), but any change should be clarified by a doctor.
A breast tumor is found in more than half of the cases in the upper outer quarter of the breast, which is why this area should also be given special attention during self-examination. Breast cancer, however, is not always easy to detect in self-examination.
In addition, every woman should have an early diagnosis examination by a gynecologist once a year. Physical exam and regular medical check-ups play a major role in the early detection of breast cancer. Women between the ages of 50 and 69 have the option of having a mammography screening (chest x-ray) every two years. Before the age of 50, only about 20 percent of all breast tumors occur, which is why only high-risk patients before the age of 50 should receive regular mammography screening.
Another important way of detecting a breast tumor at an early stage is, in addition to self-examination and mammography screening, an ultrasound examination (Sonography) of the breast. Even if a lump was discovered during the palpation examination, an ultrasound examination is always carried out. For example, it can be differentiated whether it is a benign cyst in the breast (cavity filled with fluid) or a fibroadenoma (frequent benign new tissue formation in the female breast).
Some forms of breast tumors can be diagnosed with the ultrasound examination, in unclear cases one is used to be sure Breast biopsy (taking a tissue sample) taken and examined.
In principle, it is advisable to consult a doctor for every change that is perceived in the chest.
Changes that indicate breast cancer can include:
- nodular tactile findings,
- newly appeared retractions and bulges of the chest,
- Discharge from the nipple
- a retraction of the nipple.
Breast cancer can be detected early or excluded through further examinations.
Please also read our page Detecting Breast Cancer, Pus from the nipple
Is Breast Pain an Indicator of Breast Cancer?
Breast cancer does not cause pain or other discomfort in the early stages.
Cyclical chest pain, which occurs regularly in connection with the menstrual cycle and usually disappears with the start of your period, is in most cases due to hormone fluctuations and is therefore not a cause for concern and is not a sign of breast cancer.
In later stages, breast cancer can occasionally cause pain, which in most cases occurs unilaterally in one breast and is not related to the menstrual cycle.
Where is breast cancer located?
Breast cancer is most commonly located in the upper, outer quadrant and can extend as far as the lymphatic drainage pathways in the armpit. The reason for this is that the largest gland volume is present at this point. Theoretically, breast cancer can also be located anywhere else in the breast.
Symptoms
Often times, breast cancer is not detected by a certain discomfort or pain. Most breast cancer is diagnosed when the person concerned or the gynecologist feels a lump during the check-up.
However, there are some signs that at least need to be clarified whether it could be breast cancer.
These include, for example, hardening of the breast or the breast skin, as well as pain, pressure or a feeling of tension in the chest.
In addition:
- Retraction of the breast skin
- Inflammation of the breast or breast skin
- Itching around the nipple area
- Changes in the nipple
or - Fluid leaking from the nipple (especially bloody secretion)
As with any cancer, breast cancer can also have general symptoms such as a general feeling of weakness, loss of appetite, weight loss (unintentionally, in a short time) or night sweats. However, one or more of these symptoms does not necessarily have to be caused by breast cancer . They can also be triggered by other diseases.
In more advanced stages, breast cancer is sometimes only recognized when daughter tumors (metastases) have spread to lymph nodes or other organs.
Read more about this: Lymph node involvement in breast cancer
Depending on the location of the tumor settlement (metastases), symptoms such as a palpable thickened lymph node in the armpit, shortness of breath or breathing difficulties, bone pain, but also headaches, impaired consciousness and impaired sensitivity can result.
These complaints are not exclusively caused by cancer and can also occur with other diseases or in some cases in healthy people.
Read more about this on our website Symptoms of breast cancer.
Breast cancer pain
Chest pain is very common, with almost all women experiencing chest pain, especially in the second half of the cycle. These pain usually get better or go away with the onset of your period.
These complaints are harmless and are caused by hormones.
Breast cancer does not cause discomfort or pain, especially in its early stages. However, symptoms such as pain, pressure, or tightness in the breast can occur in breast cancer.
Since these symptoms of breast cancer can also indicate other diseases (e.g. fluid-filled cysts in the breast), it is always advisable to have the symptoms clarified by a gynecologist in order to find out the actual cause.
Read more about the here Signs of breast cancer.
Back pain
If back pain occurs which can only be linked to breast cancer, the suspicion of bone metastases must be considered. Of course, back pain can have many other causes, but if you are known to have breast cancer, a metastasis should be ruled out as far as possible.
Metastases
In the advanced stages of breast cancer, tumors can spread (metastases) to other organs, for example in the bones.
Individual breast cancer cells migrate to other tissues or organs via the blood or lymph flow. So far, it does not make sense to search for these individual cells using sophisticated methods, as many of them perish as a result of adjuvant hormone or chemotherapy.
Even so, some of these breast cancer cells may sooner or later grow into metastases, most commonly:
- in the bones
- the lungs
- the lymph nodes above the collarbone
- the liver
- of the skin
or - in the brain
These metastases can still be discovered decades after an initially successful treatment of breast cancer. At present, it is not always possible to achieve a permanent cure when metastasis occurs in breast cancer.
The current aim of treatment is to control the disease for as long as possible, alleviate symptoms and maintain the quality of life of those affected. Depending on where metastases have formed, the course of the disease can vary greatly.
Several factors play a role in the treatment, such as the biological characteristics of the tumor, age, hormonal situation, general health and the wishes of those affected.
In the treatment of metastases, drugs are primarily considered, as they have a systemic effect (affecting the whole body).
Hormone and chemotherapies are available, and bisphosphonates for bone metastases. In some cases, metastases can also be operated on or irradiated.
Read more information on this topic below Metastases in breast cancer.
Bone metastases
Bone metastases in breast cancer are most commonly found in the spine, pelvis, or long tubular bones such as the thigh bone. You may notice pain in the area or sudden fractures without trauma. Bone metastases are either stabilized by surgery or they can be irradiated. The irradiation can both lead to the bone substance becoming more stable again and also relieve the pain. Which therapy method is used must always be decided in the individual case.
Metastases in the liver
Metastases in the liver are not atypical of advanced breast cancer and often occur within three years of initial diagnosis. Typical symptoms may include yellowing of the skin or a palpable enlargement of the liver. As long as they can be locally delimited and have not yet grown around larger vessels, they can be operated on and removed. It is important that the metastases are removed in their entirety and that no remnants remain.
Metastases in the brain
Metastases in the brain can manifest themselves in the form of paralysis, other failures or changes in personality. This depends a lot on how big the metastasis is and where in the brain it is located. If there is only a single metastasis, an attempt would be made to remove it with an operation and then irradiate the region. Whole-brain irradiation is considered if there are two or more metastases. In addition to this specific therapy, systemic chemotherapy, immune and hormone therapy should also be used.
What does lymph node involvement mean?
Lymph node infestation generally means that tumor cells have accumulated in the lymph nodes. It also means that it is no longer a question of local tumor growth, but that the tumor has already achieved systemic spread. The tumor cells are transported to the nearest lymph nodes via the lymphatic drainage pathways in the breast. In the case of the breast, these are the lymph nodes in the armpit. Lymph node involvement also plays an important prognostic role in breast cancer.
Read more on the topic: Lymph node involvement in breast cancer
It depends on whether the lymph nodes are affected and how many. In addition, the lymph node involvement has an impact on the therapy. If you suspect that the sentinel lymph nodes are affected before the operation, they must be removed and pathologically examined during the operation. The sentinel lymph nodes are the lymph nodes that are attacked first when the tumor spreads. If the sentinel lymph nodes are not infected by tumor cells, the remaining lymph nodes can remain in the body. In the event of an attack, at least 10 lymph nodes are removed from the armpit.
Diagnosis of breast cancer
Most women (around 75% of all women with breast cancer) notice a lump in their breasts themselves as the first sign of breast cancer and then visit (consult) their gynecologist. In other patients, breast cancer is discovered, for example, during a preventive examination.
The attending physician must first find out about the patient's symptoms and risk factors (anamnesis). Both breasts must then be viewed (inspected) and scanned for possible nodes (palpated) become. If the doctor finds something abnormal, a mammography and / or mammography ultrasound of the breast is performed.
Mammography is a special type of chest x-ray. It is carried out during cancer screening or when breast cancer is suspected. Conspicuous clusters of cells in the breast can be easily recognized.
Mammosonography is a special type of ultrasound examination (sonography) of the breast. It is usually done in addition to mammography.
Magnetic resonance imaging (MRI) of the breast (breast MRI) is rarely used as an examination method, since this method misses 60-70% of all cancer precursors, for example. However, magnetic resonance imaging of the breast can be useful for distinguishing a tumor from a scarred change in the breast. Magnetic resonance imaging of the breast is also a helpful examination for discovering breast cancer if cancer cells are found in lymph nodes of the armpit, but no tumor in the breasts is visible in mammography or mammography.
Please also read our topic: MRI for breast cancer
For a more detailed examination of a tumor, a tissue sample (biopsy) can be taken from the tumor with the help of a special needle (minimally invasive fine needle aspiration). This tissue sample can be used to identify what type of tumor it is and whether it is malignant or benign (benign). If the tumor is malignant, a statement can also be made about the type of breast cancer present.
Read more about here Tissue samples in breast cancer.
If a malignant tumor has been recognized by means of the above-mentioned examinations, it makes sense to examine other organs in which the cancer settles for cancer (screening). This is done by taking a chest x-ray (Chest x-ray), an ultrasound scan of the liver (liver sonography), a gynecological examination and a bone scintigraphy.
Read more on the topic: Chest x-ray (chest x-ray)
A bone scintigraphy is an imaging procedure used to visualize tumors or inflammation using nuclear medicine methods. More precisely, this means that a certain substance, in which so-called radionucleotides are present, is injected into a vessel of the patient. In a bone scintigram, these radionucleotides accumulate specifically in the bone, specifically directly in the cancer or inflammatory cells. They emit bundled gamma rays that can be measured with a special camera (gamma camera) and converted into an image. If the patient now has cancer cells in the bone that have spread from the breast cancer, this can be recognized with the help of such a scintigraphic image.
Please also read our page Breast cancer screening.
Mammography
Mammography is a procedure that works with X-rays and can reveal microcalcifications in the breast. It is part of the breast cancer screening program. From the age of 50, every woman is recommended to have a mammogram every two years. In addition, mammography is used in women over 40 to clarify abnormal palpable findings.
Read more on the topic: Mammography
How do you feel breast cancer?
An important part of the early detection of breast cancer is the instruction of the patient to palpate the breast independently. Before you start to feel, you can also look at the breasts on the same side. New asymmetries indicate changes in the tissue. So you look at indentations, bulges or changes in the skin. In addition, you also look at the nipples, as there is breast cancer here too.
The palpation examination is carried out once with the arms hanging and then with the arms raised. You should be careful to feel all areas of the chest. This works best if you divide the breast into four quadrants and work on each quadrant one after the other. The palpation examination is always carried out with two hands. One hand feels and the other works as an abutment. It is important to always scan both breasts side by side. In addition to the breast, the most important lymph node regions should also be palpated. This includes the armpits and the areas above and below the collarbone. Here you pay attention to enlarged lymph nodes, which can be palpated spherically.
Read more on the topic: How can you feel breast cancer?
What is breast cancer screening?
Breast cancer screening includes structured and regular preventive examinations aimed at discovering the early stages of breast cancer. In women without risk factors, the breast cancer screening program starts at age 30. However, many gynecologists also perform a palpation examination of the breast as part of the gynecological examination and instruct the patients to self-examine. From the age of 50 to the age of 69, a biennial mammogram is part of the early detection, in addition to the palpation examination. Sonography or an MRI of the breast are only used for special questions and are not standard.
If there is a hereditary breast cancer in the family, an intensified early detection program is carried out. As a rule, you start with the annual palpation examinations from the age of 25 and the mammography from the age of 40. There are also family constellations in which mammography can be indicated from the age of 30. Particularly in this group of patients is also that from the age of 25, in addition to the palpation examination, a sonography and an MRI are performed annually. There is currently no breast cancer screening for men. Structured early examinations can be useful for people at risk.
Read more on the topic: Breast cancer screening
Breast cancer in men
Breast cancer in men is by far not as common as that in women. In Germany, 1.5 out of 100,000 men develop breast cancer every year. This means that every 800th man in Germany will develop breast cancer in the course of his life. Breast cancer in men is genetically predisposed in 25% of cases, but obesity and radiation to the chest wall can also increase the risk of breast cancer in men. The diagnosis is based on the scheme for female breast cancer.
There will be a consultation with a doctor, a physical examination, as well as mammography and sonography. Since breast cancer in men often has a hereditary cause, genetic counseling should also be offered to identify other people at risk. As a rule, a mastectomy is performed as surgical treatment and the sentinel lymph nodes are removed and examined, as is the case with women. In the case of larger tumors (> 2 cm), lymph node involvement or negative hormone receptor status, re-irradiation is always carried out in men. The surgery is followed by adjuvant system therapy. The recommendations for chemotherapy and immunotherapy are identical to those for women. Often, male breast cancer is also positive for the hormone receptor. In this case, tamoxifen is given for 5 years as in women. Aromatase inhibitors are rather atypical for men.
Breast cancer is the most common type of cancer in women, which is why, from a purely statistical point of view, men have a much lower risk than women of developing breast cancer. Since breast cancer is a typical disease in women, this type of tumor is often discovered late in men.
For most men, it is difficult to find out what exactly caused the breast cancer in retrospect. So far, only a few factors are known that increase the risk of breast cancer in men. These include, for example, so-called breast cancer genes. There are some inherited or spontaneously occurring genetic changes that increase the risk of breast cancer in both women and men (e.g. BRCA genes, breast cancer genes). These genetic changes are only found in a few people affected. Hormonal factors also play a role in the development of breast cancer. Men (like women) also produce the sex hormone estrogen, but usually in much smaller quantities than women.
Higher estrogen levels occur, for example, in people who are very overweight or have liver diseases such as cirrhosis or shrinkage.
Suspected of increasing the risk of breast cancer, there are also hormones for increasing performance, such as those taken by bodybuilders over a long period of time.
Men who have what is known as Klinefelter's syndrome (one or more extra female X chromosomes) are at a similarly high risk of breast cancer as women.
Breast cancer in men is noticeable through palpable lumps. However, fluid secretions from the nipple, small inflammations or wounds or a retraction of the breast skin or the nipple are also considered warning signals for breast cancer.
Ultrasounds and mammograms (chest x-rays) are also used in men, but are not as useful as they are in women.
The diagnosis of breast cancer is made through a biopsy (tissue sample) taken from the breast and examined. The treatment of breast cancer for men also differs little from that for women.
Areas suspected of being tumors as well as neighboring lymph nodes from the armpit are surgically removed. Sometimes supportive measures are necessary after the operation to destroy tumor cells that may have remained in the body (e.g. radiation therapy of the chest wall, chemotherapy). Anti-hormonal therapy is often indicated in men, since the tumor grows in an estrogen-dependent manner.
For more information see also: Breast cancer in men
What are the symptoms of breast cancer in men?
In men, too, painless lumps in the breast region are a sign of breast cancer. Furthermore, with whitish discharge from the nipple, changes and retraction of the nipple, as well as ulcers on the breast for malignant changes.
In the early stages there are no general symptoms, later there may be general exhaustion and decreased performance. Metastases, spread of the tumor in the body, can also lead to specific symptoms, depending on where they occur. Skeletal pain on bone metastases and swelling of the arm in the case of lymph node metastases in the armpit region can occur.
Read more about this at: How do you recognize breast cancer in men?
Treatment of breast cancer
Tumor markers
Two tumor receptors play a major role in breast cancer. The determination of these receptors, or markers, is of great importance for therapy and also for prognosis. On the one hand, you determine the HER2 receptor. A positive receptor status is initially associated with a poor prognosis, since the tumors are usually more aggressive.
However, these tumors can be treated very well with antibodies. Second, the hormone receptor status is routinely determined. Other tumor markers, which are determined for example in colon or pancreatic cancer, are usually useful in breast cancer. The tumor marker CA 15-3 can be determined in advanced breast cancer. However, it cannot be used to detect metastases, but only to control the course of therapy.
surgery
The operation in the treatment of breast cancer represents a central pillar of the therapy. As long as no metastases can be detected, an operation is aimed for in every patient. Breast cancer can be treated with two different surgical methods. Either a breast-conserving operation (BET, breast-conserving therapy) is performed or the breast is removed as part of a mastectomy. Which procedure is used depends on the extent and location of the tumor.
The mastectomy is the older of the two methods. During the operation, the entire breast (glandular tissue and skin) and, if necessary, the underlying pectoral muscle is removed. A breast augmentation with a breast implant can take place at a specified interval after the operation or the radiation. The newer BET only removes the tissue with the tumor and a small piece of skin.
The rest of the glandular tissue and skin are left. BET is now carried out in around 70% of all patients and inevitably involves irradiation of the remaining tissue. Every operation usually includes the removal of lymph nodes from the armpit. How many lymph nodes need to be removed depends on whether there are tumor cells or not.
Also read the article on the topic: Surgery for breast cancer
chemotherapy
Chemotherapy (short: chemo) is of great importance in the treatment of breast cancer.
Not every form of breast cancer can and must be treated with chemotherapy; there has to be a clear reason for it.
Each breast cancer must be treated differently and each time an individually tailored and carefully selected therapy must be carried out. With chemotherapy as part of the breast cancer treatment plan, depending on the phase of the disease in which the chemo is performed, a distinction is made between:
- primary (neoadjuvant)
- adjuvant
or - palliative therapy.
Primary chemotherapy is usually done before surgery, which can be especially important if, for example, surgery is not possible, if the tumor is too large or inflamed. Most of the time, surgical treatment is then carried out to finally remove the tumor. One speaks of adjuvant therapy when chemotherapy is carried out after an operation and there are no tumor deposits in other organs (metastases). If tumor settlements have already been proven, chemotherapy can also be useful; this is then referred to as palliative therapy.
This palliative chemo can be useful to treat symptoms such as pain caused by metastases, shortness of breath or skin symptoms.Chemotherapy drugs) Many factors have to be taken into account, such as organ functions (especially heart and bone marrow), tumor settlements, symptoms and much more. Since many different chemotherapeutic agents are approved for the treatment of breast cancer in Germany, an individual and optimal therapy can be achieved.
Read more on the topic: Chemotherapy for breast cancer
Here you can also find out about the general Therapy for breast cancer and the Irradiation for breast cancer to inform.
Irradiation
After each breast-conserving operation, the remaining breast tissue and possibly also the armpit on the side is irradiated. This is to prevent a second tumor from forming locally. So far, irradiation has only been referred to in rare cases, e.g. in elderly patients with a certain tumor constellation. After a complete breast removal, re-irradiation is only initiated in advanced tumors or if not all of the tumor tissue could be removed. However, the individual indication for irradiation must be made by the treating team of doctors and general statements cannot be made here.
Irradiation of the lymph drainage pathways in the armpit is also possible after surgical removal of the lymph nodes. This is said to improve overall survival. Similar to radiation after mastectomy, the decision to irradiate the lymphatic drainage path must be made by an interdisciplinary team. So-called boost radiation can still be carried out in young patients. Here, the former tumor bed is irradiated with a higher dose after surgery to reduce the risk of recurrence. In addition, inoperable tumors can also be irradiated with the aim of reducing the tumor mass to such an extent that an operation is possible.
Read more on the topic: Irradiation for breast cancer
Hormone treatment
Hormone therapy, or anti-hormone therapy, is performed on hormone receptor positive tumors. Hormone receptor positive means that the tumor has receptors for estrogen or progesterone. It is usually performed after the operation and also after any chemotherapy. In general, hormone therapy should be carried out for at least 5 years. A longer administration of the preparations can then be weighed against the individual risk of relapse. Since hormone therapy has significant side effects, many discontinue therapy before the age of five, which increases the risk of death.
Which preparation is used for hormone therapy depends on whether the woman is still before menopause or is already in the menopause. Tamoxifen is usually prescribed for younger women who have not yet entered menopause. It blocks the tumor's estrogen receptors and decreases the production of hormones by the ovaries. This means that the tumor cannot receive any growth signals from estrogen. Common side effects of this therapy are hot flashes, nausea, and rashes. In women who are already through menopause, aromatase inhibitors are given as hormone therapy. It also inhibits the formation of estrogen, which can no longer have a stimulating effect on the breast or on any remaining breast cancer cells. The side effects are similar to those of tamoxifen.
Read more on the topic: Hormone therapy for breast cancer
Antibody therapy
Antibody therapy is used for HER2 receptor positive breast cancer. The antibody blocks the HER2 receptors on the tumor, which means that the tumor can no longer receive growth signals via this receptor. The therapy is carried out in parallel with chemotherapy and lasts for 1 year. The most common active ingredient is called trastuzumab and is given as an infusion every one to three weeks. The main side effect of the antibody is damage to the heart. Therefore, a cardiac examination must be performed every 3 months during therapy.
Aftercare
The treatment of breast cancer consists of several forms of therapy. An important component are the operating theater with possible re-radiation and systemic therapies such as chemotherapy, immunotherapy or hormone therapy. Depending on the findings and the constellation of the tumor, chemotherapy and immunotherapy can also be started before the operation. The follow-up treatment after the operation then consists of the so-called adjuvant system therapy, in which the preoperative medication is continued and hormone therapy may be added.
If hormone therapy is indicated (if the receptor status is positive), it will be carried out for at least 5 years. Post-mastectomy treatment, i.e. breast removal, usually includes breast reconstruction. Own tissue or implants can be used here. After the primary treatment is complete, you automatically move on to follow-up care. This should run over a period of 10 years so that recurrences can be recognized and treated at an early stage. Follow-up care includes regular physical exams and consultations with a doctor, as well as annual mammograms of the remaining breast tissue.
Find out more about the topic: Follow-up care after breast cancer
When is a mastectomy necessary?
Breast-conserving therapy is always attempted whenever possible. However, some tumors grow so unfavorably that such an operation is not possible. This is the case, for example, with many large tumors that have infiltrated into the skin. Since in such cases one cannot always be sure that the entire tumor has been removed or if the remaining skin layer is not sufficient for a maintenance therapy, one would rather aim for a mastectomy, i.e. a removal of the breast.
Read more about: Mastectomy
A mastectomy is also aimed at with smaller tumors, from which not all parts can be safely removed. Since a breast-conserving operation always has to be re-irradiated, patients who cannot or do not want to be irradiated for various reasons are also given breast amputation. In addition, mastectomy is necessary for inflammatory breast cancer and also when there are multiple tumor foci in the breast.
Breast implants after breast cancer
After a mastectomy, the removal of the breast, is performed either immediately in the same session or at a time interval thereafter, the breast is reconstructed. Either your own fat tissue or a breast implant is used for this.
Prognosis and Chances of a Cure for Breast Cancer
A number of factors determine the course and prognosis of breast cancer.
Knowledge of these prognostic factors enables an estimation of the risk of tumor spreading (metastasis) and of suffering a relapse (relapse) after treatment.
Age and menopausal status (before or after the menopause), the tumor stage, the degree of degeneration of the cells and characteristic properties of the tumor play a role in the chances of recovery.
The smaller the tumor is, if no lymph nodes are involved and no daughter tumors (metastases) have formed, the better the prognosis and thus the better the chance of recovery.
Later stages are often less favorable. The degree of degeneration of the malignant tumor cells can also be helpful in assessing the prognosis.The tumor stage provides information about the aggressiveness and growth rate of the tumor. In addition, there are certain properties of breast cancer cells that determine the growth of the cell and differ between the individual breast cancer diseases. Cell growth can be promoted by female hormones (estrogens) because they have so-called estrogen receptors.
Other types of receptors also play a role. Knowledge of these characteristic properties of tumor cells makes it easier to choose the right treatment and provides information about the prognosis.
Another prognostic factor is the age of the patient at the time of diagnosis, as women under 35 years of age suffer more relapses and the prognosis is considered less favorable than in other age groups.
It is also relevant for the prognosis whether the patient is still bleeding or is beyond menopause.
Basically, the earlier breast cancer is discovered, the better the prognosis and the better the chances of recovery.
Read more about the topic on our website Breast cancer prognosis, breast cancer follow-up.
What is the breast cancer survival rate?
The survival rate for cancer is given as the 5-year survival rate. These statistics do not look at how long the individual patients survive, but rather how many patients are still alive after 5 years. The overall 5-year survival rate is 88% for women and 73% for men. The 10-year survival was 82% for women and 69% for men. However, the individual rate depends on a large number of factors, such as the tumor size, degree of degeneration or lymph node involvement, so that the survival rate must always be calculated individually.
Read more about this: Life expectancy in breast cancer
Is Breast Cancer Curable?
Breast cancer is the most common form of cancer in women and the incidence of breast cancer continues to rise in western industrialized countries.
The mortality the disease, however, has shown itself in the last few decades clearly declining. The chance of a cure for breast cancer are good, more than three quarters of those affected are still alive five years after treatment.
The significant improvement in the chances of recovery and the quality of life of those affected are due to the progress made in the diagnosis and treatment of breast cancer.
The development of the Mammography screenings (Chest x-ray) and from organ-preserving and reconstructive surgical procedures, as well as the discovery of the hereditary forms of breast cancer and the availability of hormone, chemotherapy and antibody therapy have contributed to the fact that breast cancer has become curable in an increasing number of cases.
An early detection of the tumor usually means a greater chance of a cure.
In more than 90 percent of cases, breast cancer can be cured if the tumor is smaller than one centimeter.
With a tumor size of two centimeters, the chance of recovery drops to about 60 percent.
In rare cases, however, breast cancer may no longer be curable, even if it was discovered at an early stage. The screening process (such as the annual check-up at the gynecologist) reveals around 70 to 80 percent of breast cancer tumors at a stage in which they are curable.
Also the Relapse rate (relapse) after an initially successful treatment of breast cancer is due to the optimized therapy method in recent years decreased.
Is Breast Cancer Hereditary?
There are certain mutations in the genome that lead to a higher risk of breast cancer and are also hereditary. The best-studied mutation is the BRCA gene, also known as the breast cancer gene. This mutation is inherited as an autosomal dominant trait. Humans have two copies of each gene. In the dominant mode of inheritance, it is sufficient if the BRCA gene is only mutated on one copy so that the risk of cancer is increased. This also means that there is a 50 percent chance that someone who carries this mutation will pass it on to their children. Because it is an autosomal inheritance and not a gonosomal, the gender of the children is irrelevant.
In addition to the BRCA gene, there are a number of other genes which, if mutated, increase breast cancer or the risk of other types of cancer. A distinction is made between high-risk and moderate to low-risk genes for these genes. The BRCA gene and also the PALB2 gene are among the high-risk genes for breast cancer. Moderate to low-risk genes are also associated with Li-Fraumeni syndrome, Fanconi anemia or Peutz-Jeghers syndrome, among others.
What does terminal breast cancer look like?
The stages of breast cancer are classified based on tumor size, lymph node status and the presence of metastases. One speaks of end-stage breast cancer when there is metastasis. Metastases are cancer cells that have spread to other organs such as the lungs or bones. The size and the lymph node status are initially irrelevant for the staging. The most common metastases are in the lungs or on the lung membrane, in the bones, in the liver or in the brain.
However, end-stage breast cancer does not automatically mean that there is no longer any treatment option. A curative approach is often no longer possible, but there are also good palliative therapeutic approaches. For tumors with positive antibody receptor status (Her2-positive), the therapy of choice is immunotherapy, in some cases with two antibodies at the same time. A hormone receptor-positive tumor would be treated with hormone therapy, such as tamoxifen or an aromatase inhibitor. Chemotherapy is only given for tumors that are both Her2 and hormone receptor positive.
Find out more about the topic: End-stage breast cancer
What is breast cancer recurrence?
A recurrence in breast cancer describes a recurrence of a cancerous event after therapy. The breast cancer can reappear locally in the breast area, but it can also appear as a metastasis elsewhere.
Read more on the topic: Breast cancer recurrence
How often does this happen?
Local recurrence occurs in around 5 to 10 out of 100 patients within 10 years of breast-conserving therapy with radiation. In the case of mastectomy, the rate is 5 out of 100 patients, i.e. 5%. The risk of metastases is slightly higher. About 25% of all breast cancer patients develop metastases in the course of their lives.
What degree of disability (GdB) is there?
After a breast removal (mastectomy) you can apply for a degree of disability temporarily or permanently. The degree depends on whether one or both breasts have been removed. A GdB of 40 can be requested for a unilateral mastectomy, and 40 for a bilateral mastectomy. If the breast is reconstructed during the course, the GdB is reduced by about 10 points. A higher GdB can be granted in the event of damage caused by the operation or radiation.



















.jpg)