Prolapse of the uterus
definition
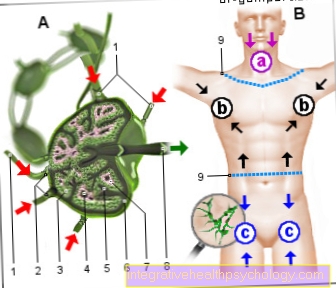
The prolapse of the uterus (also called uterine prolapse) describes a change in the positional relationship of the female genital organs to one another, which usually occurs after the menopause. Usually the uterus is at the end of the vaginal vault and is tilted back slightly.
However, when the uterus prolapses, it turns inside out through the vagina. You can then see a vaginal tube that is turned outwards and contains part of the uterus. It thus represents a particularly pronounced form of uterine subsidence (Descensus uteri).
Read more about the topic here: Uterus subsidence

Symptoms
The symptoms that a prolapsed uterus produces vary from woman to woman. Depending on whether it is a total incident (uterine prolapse) or just a lowering of the uterus (Descensus uteri), either an everted vagina and uterus itself can be seen or you can only make yourself noticeable at the gynecologist with an abdominal press.
Common general symptoms in both forms are abdominal and back pain. Many affected women also describe a foreign body sensation in the vagina. They often have the feeling that something is moving out of the abdomen through the vagina. As a result, the legs are often crossed or positioned close together.
Read more about the topic here:
- Uterine pain
- What are the symptoms of a uterine sagging?
Pain
The pain of a prolapsed uterus is particularly localized in the abdomen and back. They are often described by the patient as pulling. The back pain occurs in the area of the sacrum and tailbone.
Furthermore, pain can occur during sexual intercourse and this can be difficult. The displacement of neighboring structures by the uterus and vagina can also cause pain when urinating or defecating.
Uterine prolapse after childbirth
Women who have had multiple natural births are at greater risk of a prolapsed uterus.
During childbirth, the pelvic floor muscles and the holding apparatus are greatly stretched. This can cause direct damage to the muscles. In addition, branches of nerves can be damaged by stretching. Often these nerves regenerate in the first three months after giving birth. However, damage can also remain, which can lead to a prolapse of the uterus in later years.
Traumatic births usually cause even greater damage, so that the muscles are no longer as contractible as they were before the birth.
Read more about the topic here: Uterus subsidence after birth
therapy
Conservative
The treatment of a prolapsed uterus depends on many factors. An important point is the age of the patient and the question of whether they still want to have children. Furthermore, a distinction is made between different degrees of lowering or of the incident.
A total prolapse naturally requires a different therapy than a slight, asymptomatic lowering of the uterus. At this point, another important aspect becomes clear: Does the patient have complaints / symptoms as a result of the depression or the incident?
All of these points together form the basis for the individual therapy selection. The first stage in the treatment of uterine subsidence involves pelvic floor training. These are specific exercises that train and strengthen the pelvic floor muscles and ligaments in particular. In the case of slight forms of uterine subsidence, this can already be promising; In the case of severe forms or a prolapse of the uterus, these exercises should be carried out in conjunction with the therapy.
In addition, drugstores offer special cones for pelvic floor training, which women can insert into the vagina and only try to hold with the muscles of the pelvic floor. This also leads to a strengthening of the respective muscles. Many women are not even aware of which muscles they have to tense for pelvic floor exercises. In this case, professionally supervised training, e.g. with a physiotherapist, bring clarity.
For affected women who are already in their menopause, there is another symptom-relieving option with hormonal treatment.
Read more about the topic here: Menopause
Creams containing estrogen
Special estrogen-containing creams or suppositories (estrogen is the female sex hormone) that are introduced vaginally can also help treat uterine subsidence. Vaginal rings that continuously secrete a certain amount of estrogen can also be used.
Another non-invasive therapy option that is particularly suitable for older patients is the pessary. This is a mechanical support for the uterus and thus the pelvic floor.
Also read our topic on the pessary: GyneFix® copper chain
Operational
In particularly severe cases of uterine subsidence or prolapse, surgery is usually the method of choice (see also: OP of a uterine lowering). It takes about an hour and is performed under general anesthesia. The doctor can often operate through the vagina so that there is no externally visible scar.
Sometimes, however, an abdominal incision is necessary, which is usually about 5 cm long and is made across the lower abdomen. The aim of the operation is to move the lowered or even everted abdominal organs back to their original place and to fix them there.
There are various possibilities. So-called vaginal plasty (Kolporrhapie) is most frequently used: the anterior plastic for a bladder and vaginal sagging and the posterior plastic for a lowering of the rectum and vagina. Here, the pelvic floor muscles are gathered and the bladder or rectum pulled up and sutured.
For women who no longer want to have children, removal of the uterus (hysterectomy) is a frequently used treatment option. During this operation, the entire uterus is removed through the vagina. What remains is the sutured vaginal stump, sometimes with the cervix.
To prevent a new incident, it is fixed to the pelvic bone using special strips of tissue (vaginosacropexy). Another surgical method is the TVM (transvaginal mesh method), in which the surgeon implants a mesh between the pelvic floor and the bladder. This procedure can also be carried out vaginally and is therefore a good option for treating uterine prolapse from a cosmetic point of view.
In some patients, however, the prolapse is also accompanied by urinary incontinence (uncontrolled leakage of urine). In this case, an operation method should be chosen that focuses on the function of the urinary pathways. No serious complications are known for any of the therapy methods mentioned. As a rule, patients remain in the hospital for about 3-4 days for inpatient control after the operation.
Read more about the topic here: General anesthesia - procedure, risks and side effects
Risks of the operation
When the anterior vaginal wall is gathered, it is removed from the bladder and individual ligaments that are connected to the bladder wall are gathered up.
This causes the bladder to stand a little higher after the operation than before. This change can lead to what is known as stress incontinence. This is urinary incontinence, which is caused by the fact that the bladder and urethra are too steep to each other and thus continence is no longer fully guaranteed.
As with any surgical procedure, there is still the risk that structures in the operating field can be injured and that further subsidence occurs.
Use of a pessary
Older patients who cannot be operated on due to their general condition are often recommended to use a pessary. This is a medical product that is inserted into the vagina in front of the cervix by the gynecologist.
Today most pessaries are made of silicone, porcelain or plastic and can be ring, bow, cube or bowl-shaped. With this treatment method, however, it should be noted that the pessary does not treat the cause of the prolapse of the uterus, but merely counteracts any further sagging of the pelvic floor.
To prevent intravaginal inflammation or pressure sores, the pessary must be changed and thoroughly cleaned at least every eight weeks. In many cases it has been found useful to apply estrogenic vaginal creams or suppositories while using the pessary. However, the prerequisite for using a pessary is that the perineum muscles are intact.
For slightly younger patients there are also pessaries that you can change yourself. These are only worn during the day, so that the vaginal environment has the opportunity to regenerate at night.
homeopathy
It is impossible to restore an already sunk pelvic floor or a prolapsed uterus with homeopathic remedies alone. However, the field of homeopathy offers remedies that can positively influence a cause of the incident.
Is the uterine prolapse, e.g. If there is a weak connective tissue, taking Silicea D3 several times a day (four globules each) should strengthen the connective tissue again.
Some affected women also report that homeopathy relieves their symptoms.
Some homeopaths are of the opinion that there are also remedies that work directly against the prolapse of the uterus. Aesculus, Aletris farinosa, Lilium tigrinum and Podophyllum are mentioned here.
In any case, however, a doctor should be consulted, who can then decide together with the patient to what extent a homeopathic therapy can be useful for her.
causes
Basically, the cause of a prolapse of the uterus is a weakening of the pelvic floor. This is made up of ligaments and muscles and can lose function and stability through overloading. A connection with vaginal births is found particularly frequently.
The birth process as well as the pressing (abdominal press means an increase in pressure within the abdominal cavity) results in a pronounced strain on the pelvic floor, which then rarely regenerates completely.
The constant bulging of the vagina can also change the vaginal environment. The otherwise very damp mucous membrane can dry out, which can often lead to inflammation. Some women also notice an increased, partly even bloody vaginal discharge. Depending on whether the prolapsed uterus affects the urinary bladder, problems urinating can also occur.
In this case, a weakened stream of urine is often noticed. In some women, urination is also made significantly more difficult by what is known as pollakiuria. Pollakiuria means frequent urination, but only very small amounts of urine can be excreted.
You get the uncomfortable feeling that there is always residual urine in the bladder. In the event that the lowered uterus pushes back on the rectum and rectum, problems with bowel movements (constipation, pain) can also arise.
A high birth weight
A high birth weight of the child can also be a risk factor for a prolapse of the uterus after birth.
It has also been observed that multiparous women observe uterine subsidence more often than women with no or only one vaginal birth.
But there are other reasons that weaken the pelvic floor. E.g. Even heavy physical exertion carried out over a number of years can overload the ligaments and muscles.
Obesity or chronic cough also mean an increase in pressure in the abdomen and thus also on the pelvic floor.
diagnosis
In most cases, a prolapsed uterus can be diagnosed quickly through a consultation with a doctor and a pelvic examination. Affected women often notice after going to the toilet that something is protruding from their vagina, which can be pushed back quite easily with the finger.
However, if the pressure in the abdomen is increased (e.g. by pressing, sneezing, coughing), another incident occurs. This description usually gives the doctor sufficient information for the suspected diagnosis of uterine prolapse.
The next step is the specular examination (speculum means vaginal mirror) on the gynecological chair. An existing uterine prolapse can be clearly identified here. In any case, a short rectal palpation examination is also carried out, during which the doctor can feel possible protrusions of the rectum into the vagina.
Finally, an ultrasound examination is carried out to assess the urinary bladder. In extreme cases, the uterus can even affect the urinary bladder.
forecast
Therapy for a prolapse of the uterus merely involves combating symptoms.
The cause, namely a weakness of the pelvic floor, usually remains untreated. This means that another organ prolapse cannot be ruled out. However, there is a way, with pelvic floor exercises, to reduce the chance of another incident.
As a prophylaxis, it is also advisable to avoid excessive physical strain in order to keep the pressure in the abdomen as low as possible. Weight reduction in overweight patients is also an important measure in avoiding a prolapse of the uterus.
Read more about the topic here: Pelvic floor training