Subarachnoid hemorrhage
introduction
Subarachnoid haemorrhage, or SAB for short, describes bleeding into the so-called subarachnoid space in the skull due to a ruptured blood vessel. It is a medical emergency that should be treated immediately by a doctor.

Symptoms
The skull cannot expand due to the bones, so any increase in pressure leads to massive symptoms, as the brain has little opportunity to evade the pressure and the meninges cannot stretch. The increased pressure in the brain can lead to rapid death by compressing important circulatory centers in the brain stem.
About 50% of those affected report severe headaches, which can probably be explained by the stretch-induced irritation of the extremely painful meninges.
Another symptom is unconsciousness, which can result from the increasing pressure inside the skull and on the brain structures. Another reason for unconsciousness and death is the secondary occurrence of massive reactive vasospasms, which lead to an insufficient supply of the brain structures with blood (and thus vital oxygen). This causes areas of the brain to die off (ischemia).
Neck stiffness and vomiting are further indicators of a search archanoid hemorrhage, but a differential diagnostic work-up (is it really an SAB or can the present symptoms also suggest other diseases?) Is essential.
According to Hunt and Hess, SAB (search archanoid hemorrhage) is divided into severity grades 1 to 5 (I to V), which can be used to determine the severity.
For more information, also read: Symptoms of a cerebral haemorrhage
therapy
If SAB (subarachnoid hemorrhage) is diagnosed, the patient is immediately transferred to the intensive care unit and treated there with medication (medication against brain swelling and vascular cramps).
To avoid recurrence of bleeding (recurrent bleeding), surgical treatment is given:
- Clipping: the aneurysm is closed with a clamp
- Coiling: obliteration of the aneurysm by inserting a platinum coil (the following coagulation processes lead to obliteration)
Read more on the topic: Therapy of a cerebral hemorrhage
Therapy for high blood pressure
In addition to acute treatment through coiling or clipping, it is also important to treat so-called risk factors. High blood pressure is one of these factors. However, the problem is that the treatment of high blood pressure can sometimes cause blood pressure to be too low. After the previous bleeding, this can lead to a narrowing of the vessels and thus to a reduced blood flow (ischemia).
Therefore, many doctors are not entirely in agreement from which blood pressure values a blood pressure therapy should take place. A common drug here is, for example, Urapidil.
forecast
About 1/3 of all those affected survive such bleeding without major physical or mental restrictions.
The other 2/3 of the patients unfortunately retain damage to the brain or die mainly from the compression of vital centers in the brain stem (respiratory center, circulatory center) or oxygen deficiency (ischemia) of vital brain areas due to vasospasms.
Read more on the topic: What are the chances of recovery after a cerebral hemorrhage?
causes
This is a hemorrhage into the space that lies between the spider tissue (arachnoid) and the soft meninges (pia mater) and is filled with liquor.
Such bleeding usually results from a suddenly ruptured blood vessel (in this case: artery). The reason for this tear (med. Rupture) is usually a so-called aneurysm.
An aneurysm describes a bulging of the blood vessel wall, the main complication of which is that it can tear at any time. Until then, such a bulging usually remains asymptomatic, so the patient has no complaints.
Aneurysms can be acquired or congenital. Acquired aneurysms usually arise as a result of pathological changes in the arterial wall in the form of calcium deposits, which is referred to as atherosclerosis (also: arteriosclerosis).
If such a vascular bulge tears, blood from the artery enters the subarachnoid space. Due to the high pressure in the arterial blood vessels, the blood is pumped in at high pressure, so a lot of blood flows out of the vessel into the subarachnoid space in a very short time.
diagnosis
Since subarachnoid hemorrhage is a very acute clinical picture with potentially serious complications, it is crucial to ensure a quick diagnosis. Therefore, computed tomography is primarily performed, as this procedure quickly confirms the diagnosis in most cases. In some cases, an MRI can also be helpful. A so-called digital subtraction angiography (DSA) can be used for visualization and localization, in which a catheter is usually pushed through a vessel in the groin to the point of suspected bleeding and the vessels are made visible in the X-ray image with contrast media. The advantage of this procedure is the possibility of being able to treat directly on site under certain conditions.
If the CT (computer tomography) does not produce a result, a lumbar puncture can be performed if necessary. Nerve water (Liquor) taken from the subarachnoid space. A visual diagnosis can then be used to determine whether there is blood in the CSF. As with any procedure, there is a certain risk for the patient, and on the other hand, the location of the bleeding in the head cannot be determined.
CT
Computed tomography is the most sensitive form of diagnosis for subarachnoid hemorrhage. This means that approx. 95% of the bleeding can be detected on the CT. The reason for this is that the CT is particularly good at showing acute bleeding, which is usually the case with subarachnoid haemorrhage.
In this form of imaging, many slice images are made. It must be noted that a CT, compared to other imaging methods, involves a comparatively high level of radiation exposure. However, given the great advantage of rapid diagnosis, this plays a subordinate role.
MRI of the brain
Occasionally, brain CT does not adequately exclude whether the haemorrhage is subarachnoid or otherwise. In this case, magnetic resonance tomography can help. The advantage of this cross-sectional imaging method is that so-called subacute bleeding can be recognized. So if there is no heavy bleeding that acutely leads to neurological impairment, but "only" a small bleeding that continues to bleed slowly over several days, for example, this can be easily recognized in the MRI.
Classification according to Hunt and Hess
The classification according to Hunt and Hess is based on the symptoms of the patient and is divided into grade 1 to grade 5. Grade 5 is the most severe form and is associated with a high probability of death. Patients with a grade 1 according to this classification are quite inconspicuous and usually only have a slight headache. Patients classified in grade 5, however, are in a coma. The classification according to Hunt and Hess is more common than that according to Fisher.
Classification according to Fisher
One possibility to classify the subarachnoid hemorrhage is the classification according to Fisher. This is based on the CT images. There is an old and a modified variant, whereby the modified variant is divided into grade 0 to grade 4. The width of the bleeding and the bleeding into the ventricle, which is filled with nerve water, play a role as criteria. Grade 4 describes the most severe form, for example, a subarachnoid hemorrhage that is wider than 1mm and has bled into a ventricle. These days, the Fisher graduation is no longer used by default.
Subarachnoid Hemorrhage or Stroke - What Are the Differences?
A stroke is generally a circulatory disorder in the brain. This can be caused by reduced blood flow (Ischemia) and excessive bleeding. The latter bleeding is often subarachnoid hemorrhage. These are the cause of around 10% of all strokes.
Subarachnoid hemorrhage is always a bleeding into the subarachnoid space filled with nerve fluid, which can result from a vascular sac or an accident with head injury.
Occurrence in the population (epidemiology)
The subarachnoid hemorrhage is one of the clinical picture of Stroke (Apoplexy, stroke), it accounts for about 5-10% of the causes of strokes.
The incidence (occurrence) in industrialized nations is around 15: 100,000; men and women between the ages of 40 and 60 are most frequently affected.
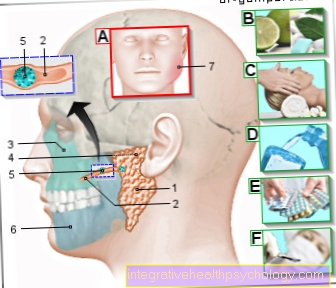
Anatomical foundations of the human skull
To understand the localization, the meninges should be briefly discussed here:
Meninges & cleft spaces
The outermost layer of the human skull is the so-called "scalp", or the scalp. It is visible from the outside and is usually covered with hair. The skull bone (skull cap) lies under this rind.
This is followed by the hard meninges (dura mater, also: pachymeninx = thick meninges) on the inside. By definition, it consists of 2 leaves, the outside of which is fused with the cranial bone.
The leptomeninx (thin or soft meninges) lies against the inside of the hard meninges.
It consists of 2 parts: arachnoid (spider tissue) and pia mater (soft meninges). The pater mater lies directly against the brain.
So from the outside in there are the following meninges:
- Dura mater with two leaves (hard meninges)
- Arachnoid (cobweb skin)
- Pia mater (soft meninges)
Although one would think that there are small gaps between all these skins, this is usually not the case in the brain.
A space between the skullcap and the outer leaf of the dura mater (epidural space, “epi” - Greek: above, ie “space above the dura mater) only arises when there is a bleeding from a blood vessel.
The same applies to the space between the inner sheet of the dura mater and the arachnoid (subdural space, “sub” - Latin: under, thus: “space under the dura mater).
An exception is the space between the arachnoid and pia mater (subarachnoid space, ie "space under the arachnoid"). It is always present and contains the cerebrospinal fluid (liquor cerebrospinalis), which washes around the brain and spinal cord (i.e. the parts of the central nervous system).

























.jpg)
