Cortisone therapy for joint diseases
Synonyms
Cortisone syringe, corticoid crystal suspension, intra-articular cortisone injection, risks of intra-articular injection, betamethasone, dexamethasone, triamcinolone
introduction
Glucocorticoids, also known colloquially as "cortisone", are very effective drugs in the treatment of all types of inflammation and the pain associated with it. In the case of inflammatory joint diseases, they are injected directly into the joint in the form of so-called crystal suspensions.

Cortisone therapy
In cortisone therapy in the joint, for example in degenerative diseases such as Knee osteoarthritis, the active ingredient quickly gets to where it is needed, fights the inflammation and quickly makes the patient pain-free and mobile again.
Side effects of cortisone therapy
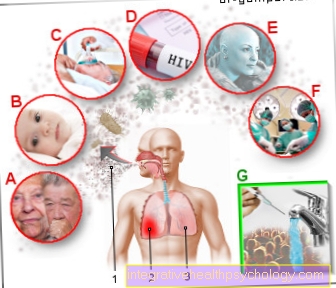
In principle, there is a risk of bacterial infection (septic arthritis) with every injury to the body, even with a joint injection. Therefore, your doctor will only perform the procedure under strict hygiene measures. If carried out correctly, the risk of infection is low.
Depending on how easily the area to be treated is accessible to the syringe, injuries to the surrounding tissue cannot be ruled out. Blood vessels can also be injured, as can nerves, tendons and cartilage surfaces.
It can also happen that the syringe misses its target and the injection is given in surrounding areas. For example, injecting cortisone directly into tendon tissue or fat tissue is harmful, as the affected structures can recede. When injecting into tendon tissue, there is a risk of tendon rupture. In addition, it is conceivable that the injected active substance is distributed from the joint through the puncture channel into the surrounding tissue and causes undesirable side effects there. Therefore, the joint should rest after the procedure!
Occasionally skin changes appear around the puncture site.
Sometimes a single treatment is not enough to relieve pain. However, if you inject again with cortisone, the risk of side effects increases. Therefore, especially in older patients, multiple applications should only be carried out after carefully weighing the benefits and risks.
Compared to systemic therapy with cortisone, topical therapy in the form of injections has a lower risk of side effects.
In systemic therapy, the cortisone is usually taken as a tablet or administered intravenously. The cortisone is then absorbed via the digestive tract and reaches all parts of the body via the blood. Therefore, side effects can then occur in a generalized manner, i.e. anywhere on the body.
When cortisone is injected into a specific part of the body using a syringe, the dose is usually low and its distribution into the surrounding tissue is limited. This also reduces the risk of suffering side effects. However, if cortisone injections are used frequently at high doses, this can ultimately lead to systemic effects.
In severe cases, the systemic effects can cause the body to appear bloated and the body fat to be redistributed. A full moon face and thin skin can also occur (also known as Cushing's syndrome). However, these systemic side effects are only to be feared at high and frequent doses.
At lower doses, as occurs with local syringes, slight systemic side effects such as An increase in blood sugar levels, a feeling of warmth and flushed cheeks occur.
Read more on the topic: Taper off cortisone
Areas of application
Inflammation of the joint apparatus (knee, hip, etc.) can have various causes. They can be caused by overexertion, improper exercise, age-related wear and tear (degeneration), autoimmune diseases (the body destroys its own tissue) or bacterial infections.
Depending on the type of illness, your doctor will try to improve the symptoms by resting and relieving the pressure on the joint, physiotherapy, the administration of anti-inflammatory drugs (so-called non-steroidal anti-inflammatory drugs, or NSAIDs for short) and, if necessary, painkillers.
Only if the causal treatment does not lead to a significant reduction in inflammation and pain should one consider using cortisone injections. However, they must not be administered to treat acute bacterial inflammation!
It is important to know that the administration of cortisone does not eliminate the cause. However, the resulting inflammation is fought effectively and pain is quickly relieved. This gives the sick person back freedom of movement and quality of life. The injection (injection) of cortisone (cortisone) can be done either directly into the synovial fluid or at tendon attachments, in tendon sheaths, bursa, etc., depending on where the inflammation is active. The use of a cortisone injection may be considered in the following diseases:
- stubborn inflammatory joint disease for which causal therapy does not provide significant relief
- non-infectious joint inflammation (rheumatoid arthritis)
- inflammatory relapses in joint diseases caused by wear (activated knee arthrosis, hip arthrosis), e.g. B. triggered by abraded cartilage
- inflammatory conditions at the junction between tendons and bones (e.g. tennis elbow, heel spur)
- Non-bacterial tendinitis (tendovaginitis)
- Non-bacterial bursitis (e.g. shoulder bursa: subacromial bursitis)
- Joint capsule inflammation (synovitis)
Cortisone injection in the knee
In most cases, a cortisone injection into the knee is given into the joint. Mostly inflammatory diseases of the knee are treated in this way, which could not be treated with other treatment methods. For example, rheumatoid arthritis, osteoarthritis, joint capsule inflammation or (non-bacterial) inflammation of the bursa (bursitis) can be treated with cortisone.
Cortisone therapy in the joint is usually not the doctor's first choice at the start of therapy. This is because cortisone therapy (even when applied topically) can have side effects.
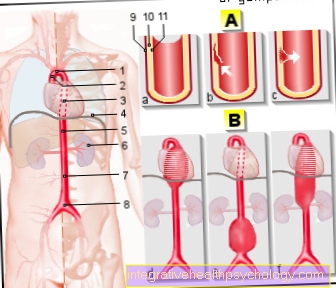
If the practitioner nevertheless decides in favor of cortisone therapy, he will first disinfect the skin over the affected joint. This is very important to prevent skin germs from getting into the wound. Then the needle is pierced through the disinfected skin and the cortisone is injected into the affected area (e.g. joint gap or bursa).
If the joint is difficult to reach (such as the hip joint), an X-ray machine or an ultrasound machine can be used. These are used to provide a better overview of the needle guide and show the practitioner exactly where the needle is in the joint.
The puncture through the skin is accompanied by a slight, sharp pain, comparable to a vaccination. During the injection, you may feel pressure in the knee joint. After the syringe, pressure is applied to the puncture site with a sterile swab to stop the bleeding. The symptoms should now subside after a few hours.
Sometimes the pain may initially worsen within the first two days. This is because the crystalline structure of the cortisone can irritate the tissue. Cooling or pain medication can help combat these symptoms.
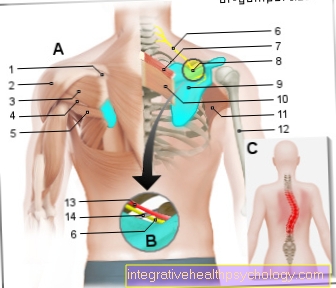
Cortisone injection into the shoulder joint
The shoulder joint can also become inflamed and then pain and be restricted in its mobility. Tendonitis caused by chronic irritation is often responsible for this. One example is impingement syndrome. Tendons (especially of the supraspinatus muscle) or parts of the joint capsule are pinched in the joint space.
These inflamed soft tissues can be treated with cortisone therapy. The irritated and inflamed tendons heal through cortisone. It is important, however, that the shoulder is spared in order to ensure that the damaged soft tissue structures heal. Bursitis or rheumatoid arthritis can also be treated with cortisone injections.
The cortisone has an anti-inflammatory effect in the shoulder joint and thus ensures a reduction in pain and increased mobility. The process of the cortisone injection is usually the same as the injection into other joints.
Advantages of the cortisone injection in the joint

Treatment with cortisone (cortisone) can be carried out in tablet form via the bloodstream (systemic). But especially in the case of joint diseases, giving a cortisone injection is the more effective solution for combating local inflammation.
The active ingredient is injected directly where it is needed to effectively fight the inflammation. So the risk is on side effects common to cortisone to fall ill, considerably less than when taking tablets, where the active ingredient first has to be transported through the whole body.
So-called crystal suspensions are used for injection (“syringe”). The special thing about it is that the active ingredient is present in an alcoholic solution in the form of tiny crystals (<10 μm in diameter). Injected into the diseased region, they decompose only slowly and thus work over a longer period of time. This "depot effect" ensures long-lasting freedom from pain. In this way, the cortisone injection enables the patient to move painlessly again, increases their mobility and improves their quality of life. However, care should be taken to ensure that the sudden freedom from pain does not lead to excessive strain on the joint. The underlying disease could recur or worsen.
Read more about this under Cortisone injection
How often should an application be made?
For many patients, a single application is sufficient to resolve the symptoms. Depending on the preparation, the anti-inflammatory effect lasts for 3 weeks. If the inflammation has not completely subsided after this, further cortisone infiltrations should not be carried out too close together. No more than 4 applications per year should be used per joint.
When should a cortisone injection not be used?
A cortisone infiltration must never be carried out if a beakterial infection is suspected!
If you are planning to have a vaccination or have been given a vaccination, you must not be given any cortisone infiltration 8 weeks before or 2 weeks after.
Active ingredients
The most common glucocorticoids that are used as crystal suspensions for joint diseases are:
- B.etamethason
- Dexametasone
- Triamcinolone
and - Prednisolone.
They differ in their strength and duration of action. Prednisolone has the shortest duration of action and is therefore no longer preferred. The choice of active ingredient is based on the severity of the disease and the desired anti-inflammatory effect.
Betamethasone (including Diprosone® Depot)
Betametasone is an artificially produced glucocorticoid that has an anti-inflammatory effect 25 times stronger than the body's own cortisol. The above-mentioned preparation contains betametasone in two forms, one as betamethasone diproprionate and one as betamethasone dihydrogen phosphate. Both dissolve at different rates. The latter dissolves more quickly and takes effect after a few hours over a period of up to 4 days. Betametasone diproprionate dissolves much more slowly and is therefore responsible for the long-term effect of the preparation of up to 6 weeks. The dosage to be used depends on the size of the joint.
Dexamethasone (including Lipotalon®, Supertendin®)
Dexamethasone is one of the long-term glucocorticoids. It is also manufactured artificially and has an anti-inflammatory effect 30 times stronger than the body's own cortisol. It is commercially available as a solution for injection, among others. as dexamethasone acetate and dexamethasone palmitate. The latter is the active ingredient of Lipotalon®, a preparation in which the microcrystalline active ingredient is packed in fat globules.
Triamcinolone (including Lederlon®, TriamHEXAL®, Volon® A)
Triamcinolone is used in the form of triamcinolone acetate, which has an anti-inflammatory effect 5 times stronger than the body's own cortisol. Its duration of action after injection into the joint is approx. 3 weeks.