penicillin
Classification
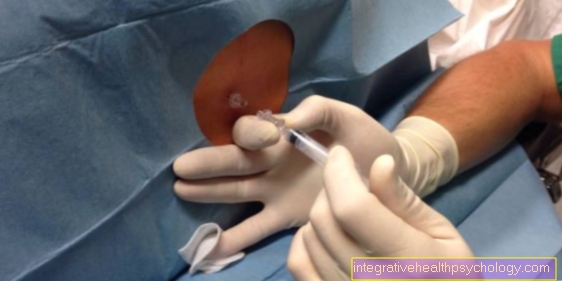
Penicillin is a very common antibiotic. It is one of the oldest antibiotics. Because of this, experience with penicillin in everyday clinical practice is very extensive. Nowadays there are many different forms of administration and variations of the original drug. The most commonly used penicillin is penicillin V and penicillin G. It is available as oral and intravenous administration. When taken orally, the drug should be taken three times a day with a duration of 5-10 days, depending on the disease and pathogen.

Side effects
Especially when penicillin is used for the first time in patients, one should be careful of allergic reactions of all kinds. These can range from minor skin rashes from the penicillin to shortness of breath, unconsciousness and death. In particular, penicillin, which is administered through the veins, should be given slowly and only under supervision for the first few minutes. Seizures have also been observed during penicillin therapy. The bacteria killed by the penicillin can also trigger a reaction in the patient (Jarisch-Herxheimer reaction), which manifests itself in chills and fever. In this case, however, penicillin therapy should be continued and accompanying symptoms treated by lowering the fever. In most cases, this response will quickly resolve.
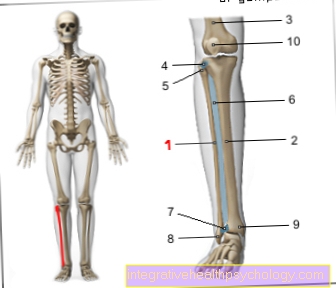
Accidental intravenous administration of depot penicillin can lead to a so-called Hoignè syndrome with anxiety and impaired consciousness, but this regresses after 15-20 minutes. If depot penicillin is accidentally administered into the artery, there is also the risk of inflammation and death of the relevant extremity (gangrene). The administration of penicillin G-potassium can lead to an unnaturally high level of potassium in the blood and resulting cardiac arrhythmias.
Please also read our article on this Antibiotic side effects
Penicillin rash
It is known that some people have an allergy to penicillin. In the case of mild courses, this leads to a rash and itching. If the course is severe, the airways can swell and breathing can be impaired, as well as anaphylactic shock with low blood pressure and a racing heart, which can lead to unconsciousness and can result in death. If reddened skin, rashes or itching occur, penicillin therapy should be stopped immediately.
There are other antibiotics available that can also be taken. If you are allergic to penicillin, the attending physician should be informed. This can also be recorded in the form of an allergy card in order to inform doctors in emergencies. The rash and itching should subside within a week at the latest after stopping the penicillin. Skin care creams and cool water on the skin have a relieving effect on these symptoms. In very severe cases, the doctor may prescribe additional soothing medication or ointments.
Read more on this topic at: Amoxicillin allergy and Amoxicillin rash
Interactions
Acid inhibitors lower the rate of absorption of penicillins and have a reduced effect when administered in parallel. Penicillins should also not be combined with other bacteriostatic drugs, as the principle of action is the same and cannot lead to any improvement in effectiveness. Beta-lactam antibiotics can inactivate antibiotics of the aminoglycoside group and should not be given in combination. The combination of penicillin with antihistamines should be weighed carefully, as the simultaneous administration can change the effect of the antihistamine. If aspirin and comparable drugs from the NSAID group are administered at the same time, the penicillin level in the patient's blood can rise due to molecular displacement, thus causing an increased effect.
The administration of probenecid prevents the excretion of penicillin and also increases the time penicillin remains in the body. Displacement with a simultaneous increase in the concentration of penicillin is also caused by the simultaneous administration of sulfonamides. Taking vitamin B1 and vitamin C at the same time reduces the effectiveness of penicillin. Penicillins inhibit the function of the blood platelets (thrombocytes). If warfarin is administered at the same time, its effect can be changed. A combined dose should only be given if precisely indicated.
Penicillin and milk
Milk and dairy products do not affect the way penicillin works. The penicillin does not enter into any connection with components of milk, so that there is no hindrance to absorption through the intestine. The drug is also widely used in pediatrics. It works very well against scarlet fever or tonsillitis (Tonsilitis), which are mostly caused by streptococci.
Due to the use of penicillin in these clinical pictures, the rheumatic fever caused by streptococci almost no longer occurs in Germany. This leads to life-threatening myocarditis (Myocarditis) with subsequent heart valve defects and kidney damage (Glumerulonephritis), avoided. It is a popular belief that antibiotics should not be taken with milk. However, this only affects certain antibiotics, namely the tetracyclines and fluoroquinolones, but not penicillin. With the other antibiotics, complex formation with calcium ions in milk results in large "lumps" that cannot be absorbed by the intestine and are excreted again without passing into the blood.
Read more on this topic at: Amoxicillin and milk - is that possible?
Penicillin and alcohol
Generally there are no interactions between penicillin and alcohol. The effect of the penicillin remains the same, it is neither strengthened nor weakened. Even so, it is often not recommended to drink alcohol while taking antibiotics. This is mostly based on the assumption that the immune system is still busy with the pathogen while taking antibiotics. Since excessive alcohol consumption damages the immune system, alcohol should be avoided if possible during a bacterial illness. In addition, both antibiotics and alcohol can hit the stomach and cause gastritis.
If alcohol is avoided while taking antibiotics, the stomach is spared and the likelihood of developing gastritis is reduced. In addition to alcohol, exercise should also be avoided during antibiotic therapy. Physical rest is recommended for infections of all kinds. Exercise during an infection can lead to insufficient healing of the disease. The pathogen sometimes even persists in the body unnoticed. This can lead to a worst case scenario Myocarditis (Inflammation of the heart muscle) or Endocarditis (Heart inflammation) come. These are both life-threatening clinical pictures and require long therapy. Sudden cardiac arrests can occur in myocarditis and valvular valve defects in endocarditis.
Read more on this topic at: Amoxicillin and alcohol - are they compatible?
Amoxicillin
Amoxicillin belongs to the group of aminopenicillins. These are a modified form of penicillins, but are also effective against most gram-positive pathogens and a few gram-negative pathogens. Aminopenicillins have the same mechanism of action as penicillin. They can also lead to an allergic reaction and must therefore not be given in the case of a penicillin allergy. Amoxicillin is also often prescribed in the form of juice for diseases of the tonsils or the throat in childhood. A peculiarity of amoxicillin exists in relation to glandular fever.
Pfeiffer's glandular fever can appear like a purulent tonsillitis. There is a reddened throat, purulent tonsils and a sore throat, possibly accompanied by a fever. Since tonsillitis is caused by streptococci, it is often incorrectly treated with amoxicillin. Since Pfeifferschem glandular fever, also known as "kissing disease" or mononucleosis, is a viral infection, amoxicillin is not effective here. A drug eruption occurs when taken. This means the affected person will get a red rash all over their body. If the rash occurs, therapy should be discontinued. There is no drug therapy for Pfeiffer's glandular fever.
Therefore, the disease must be cured with bed rest alone. It is important to know that liver and spleen swelling can occur. Therefore, no sport may be practiced, romping around with children or practicing martial arts. The swelling causes the organs to protrude from under the ribs. As a result, they are less protected and injuries with ruptures can occur. The rupture leads to life-threatening internal bleeding.
Cefuroxime
Cefuroxime is an antibiotic from the group of cephalosporins. It is usually only administered when the effectiveness against the antibiotic causing the infection has been proven. This is tested by a laboratory test. Cefuroxime is also given prophylactically during operations, as well as in the case of perforation of the appendix or contaminated wounds during the operation. A so-called enterococcal gap should be noted with cefuroxime. That means that antibiotic is not effective against gut bacteria. In addition, an existing penicillin allergy can lead to cross-reactions. If you have a known penicillin allergy, you should refrain from taking cefuroxime and use another antibiotic.
Contraindications
If you are allergic to penicillin or cephalosporin, penicillins should not be given under any circumstances, as this can lead to life-threatening complications. In children, at Breastfeeding and Pregnant women should rather be switched to alternative antibiotics. In the case of severe renal and hepatic insufficiency, careful consideration for the use of penicillins is necessary. Already exist with the patient Cramp tendencies or neurological diseases, a reduced seizure threshold with the resulting cramps must be feared when penicillin is administered.
Areas of application
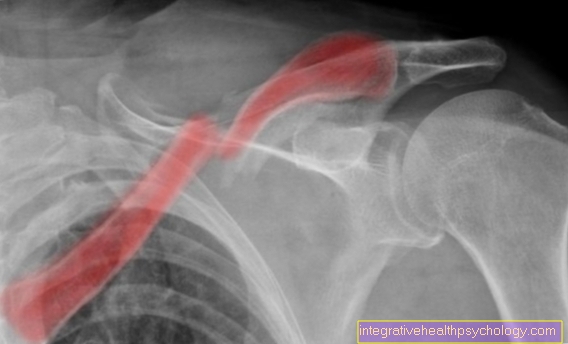
The field of treatable bacteria is large and depends on the penicillin chosen. Basically, penicillins are used in the fight against streptococci of all kinds. Pneumococci in particular (lung infection), Meningococci (Meningitis) and gonococci (syphilis) but also that Erysipelas can be treated with penicillin. Narrow-spectrum penicillins have their field of action in gram-positive germs (cocci, rods, spirochetes) and gram-negative bacteria (penicillinase-forming staphylococci). Wound infections and infections of the bones are also usually treated with penicillins.
Broad-spectrum penicillins act on enterococci and numerous gram-negative rods (Haemophilus, E. Coli).
Together with the cephalosporins and the carbapenems, penicillins belong to the beta-lactam antibiotics and represent the best-known and very frequently prescribed class of antibiotics. A distinction is made between the two groups of narrow-spectrum penicillins and broad-spectrum penicillins. The first group includes the benzyl penicillins (penicillin G and depot penicillins), phenoxypenicillins (oral penicilins = penicillin V, propicilin, azidocillin), isoxazolyl penicillins (oxacillin, dicloxacillin, flucloxacillin). The broad-spectrum antibiotics include the aminopenicillins (ampicillin, amoxicillin, bacampicillin, pivampicillin), carboxypenicillins (ticarcillin, temocillin, carindacillin), acylaminopenicillins (azlocillin, mezlocillin, apalicillin with), amidino-lacticillin, piperacillinic acid (amidin-lacticillin), apalcillicillin (amidino-lacticillin), piperacillicillin (penicillinic acid), piperacillicillin , Ampicillin + sulbactam, piperacillin + tazobactam, sulbactam).
effect
In their chemical structure, all penicillins have a so-called beta-lactam ring, a stop-shield-shaped structure that inhibits the cell wall structure of bacteria. Some bacteria have an enzyme called beta-lactamase to counteract this. This enzyme is able to split the ring of the antibiotic and so limit the effect of the drug or make it ineffective. However, some penicillins are beta-lactamase-resistant and can withstand bacterial attack. They are mainly used in the bacteria that have the enzyme. Some penicillins are acid-stable, others are not. The acid-stable ones can be administered in tablet form, as they can pass through the stomach without being dissolved and inactivated there. The non-acid stable must be administered via infusion via the blood to bypass the stomach and gastric acid. The orally ingestible penicillin G is tissue-permeable and passes into the skin, mucous membrane, liver, lungs and kidneys. It is not transported via the brain water (liquor) and should not be used in diseases of the central nervous system. It does not develop any intracellular effects and 90% of it is excreted unchanged via the kidneys.