Heart transplant
synonym
The abbreviation HTX is used in the medical sector. In the English-speaking world, one heart transplant spoken.
introduction
A heart transplant is the transplantation of an organ donor's heart into a recipient. In Germany, only a person who has been definitely diagnosed as brain dead can serve as an organ donor. In order to decide whether you would like to be considered as a donor after your death, you can record it in an organ donor card.
The world's first heart transplant was performed in Cape Town in 1967, but the patient died shortly after the operation. The first heart transplant in Germany took place two years later in Munich. But this transplanted patient also died a few hours after the operation.

It was only when a new immunosuppressant (ciclospoprin A) was developed to suppress the immune response that a new attempt at a heart transplant was attempted. That was in 1961. This time it was long-term success. For some years now, 300 to 400 heart transplants have been performed in Germany each year. The number of patients who are registered annually for such a transplant, i.e. who are on the heart transplant list, is almost twice as high. Accordingly, almost 1,000 seriously ill patients are currently waiting for a donor heart. The waiting time for a new heart is 6 to 24 months, however, well below the waiting time for a new kidney (4-5 years). There are currently almost 8,000 patients on the waiting list for a kidney.
After a successful heart transplant, the one-year survival rate is around 80%, after five years around 60-70% of the transplanted patients are still alive. The 10-year survival rate these days is around 40-50%.
indication
The indication for a heart transplant is Heart failure (Heart failure) in stage IV (4) NYHAthat can no longer be positively influenced conservatively (i.e. without HTX). Numerous criteria are included in the assessment of the need for a heart transplant, and contraindications must also be excluded. The heart failure is after New York Heart Association (NYHA) divided into 4 stages. A patient with stage NYHA I did not experience any symptoms, a patient with NYHA II complained of shortness of breath (Dyspnea) and weakness under heavy exertion, a patient with NYHA III already has such symptoms during light physical exertion and a patient with NYHA IV needs a lot of air even at rest and is no longer resilient. Heart failure is a symptomwhich can be triggered by various diseases. By far the most common causes are the coronary heart disease (CHD) and the Cardiomyopathy (Heart muscle disease). Also Valvular heart disease are not a rare cause of heart failure.
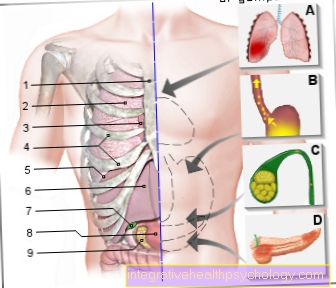
Illustration heart

- Right atrial -
Atrium dextrum - Right ventricle -
Ventriculus dexter - Left atrium -
Atrium sinistrum - Left ventricle -
Ventriculus sinister - Aortic arch - Arcus aortae
- Superior vena cava -
Superior vena cava - Lower vena cava -
Inferior vena cava - Pulmonary artery trunk -
Pulmonary trunk - Left pulmonary veins -
Venae pulmonales sinastrae - Right pulmonary veins -
Venae pulmonales dextrae - Mitral valve - Valva mitralis
- Tricuspid valve -
Tricuspid valva - Chamber partition -
Interventricular septum - Aortic valve - Valva aortae
- Papillary muscle -
Papillary muscle
You can find an overview of all Dr-Gumpert images at: medical illustrations
procedure
Patients who are on the waiting list for a heart transplant must practically always be available, as a donor organ is not infrequently available very suddenly, for example in the case of organ donors who have fallen victim to an accident. There is not much time then to explant the organ and implant it in the recipient. As a rule, no more than four - a maximum of six - hours should elapse between explanting the heart on the donor and implanting it on the recipient.
The actual operation takes place using a heart-lung machine, which - as the name suggests - takes over the function of the heart and lungs for a short time and thus enables the new heart to be implanted. A small part of the atria is left of the actual patient's heart, to which the new heart is then "connected", then the new heart is connected to the aorta and the pulmonary artery (pulmonary artery). The operation takes about 2 to 3 hours.
After the operation, the patient is monitored in the intensive care unit. Shortly before the transplant, immunosuppressive therapy is started, which is supposed to ensure that the recipient's body does not reject the foreign heart. Usually, it starts with a triple therapy with ciclosporin, prednisolone and a third immunosuppressant. Immunosuppressive therapy must be continued for life.
After a few days in the intensive care unit, the freshly transplanted patient can usually be transferred to a normal ward if there are no complications. It is not uncommon for patients who are waiting for a heart transplant to have their hearts too weak to survive the waiting period. Cardiac support systems, so-called VADs (ventricle assist devices), are used.
How long does a transplanted heart last?
How long a transplanted heart lasts and how long the life expectancy after the transplantation is very different. Three years after a heart transplant, around three out of four patients are still alive. After a successful transplant, the heart can last as long as it does in a comparable healthy person. How long the donor heart remains healthy also depends largely on the patient's lifestyle. In addition to regular follow-up care, a healthy lifestyle and sufficient physical activity according to your own resilience are important. In addition, people who have had a heart transplant have to consistently take medication that inhibits the body's immune system for life. This counteracts rejection of the donor organ. However, as a result, there is also a higher risk of getting infections. Therefore, patients must pay particular attention to hygiene and should, for example, avoid injuries and take more vaccinations (e.g. annual flu vaccination).
Read more on the topic: Organ transplant
Duration of a heart transplant
The actual surgical procedure for a heart transplant now takes about four hours on average from the skin incision to the last suture. The heart function is taken over by a heart-lung machine for around two to three hours. Rehabilitation after a heart transplant is very tedious. Due to the serious intervention, strict continuous monitoring of the cardiovascular function is first necessary in an intensive care unit. If there are no complications, the patient can be transferred to a normal ward after two to seven days. In about two weeks after the operation, if the procedure is successful, you can be discharged from the hospital. Afterwards, rehabilitation lasting several weeks is necessary so that the patient becomes productive again and learns to live with the new heart. How long this rehabilitation period lasts varies from person to person and depends on accompanying factors such as age, illness and motivation.
requirements
The requirement on the part of the organ donor is first and foremost consent to the organ donation. This happens either through the presence of an organ donation card of the deceased in which he has consented to the organ removal or, in the absence of such, the consent of the next of kin. With the consent, the next step is the declaration of brain death. This is done by 2 independent doctors, each of whom has no relationship with the transplant team. A patient can only be declared brain dead if certain criteria are met. These include the presence of a coma, the absence of cranial nerve reflexes and the absence of spontaneous breathing. Furthermore, ABO blood group equality must exist between donor and recipient. There should also be a similarity in height and weight. Finally, the presence of contraindications (see below) must be excluded.
How long is the waiting time for a donor heart?
How long you have to wait for a donor heart for a heart transplant can vary widely. The average waiting time in Europe is usually between six and 24 months. The large range is mainly explained by the fact that not every donor heart is suitable for every recipient. In addition to the appropriate blood group, the size and weight of the organ must also be appropriate. The donor organs are placed through the Eurotransplant Foundation in Leiden (Netherlands). Patients in an acutely life-threatening condition are given preference. If no suitable donor heart is currently available, there is the possibility of supporting the function of your own heart through various medical measures in order to bridge the waiting time. A mechanical support system is often used to maintain the pumping function in the heart. This is also known as an artificial heart.
Contraindications
When determining the indication for heart transplantation, contraindications must be observed that exclude HTX. These include active infectious diseases such as HIVnon-curative (with the prospect of a cure) treated cancers (Malignancies), currently florid ulcers (Ulcers) in the stomach or intestines, advanced liver or insufficiency kidney, advanced chronic lung diseases, acute Pulmonary embolism, advanced cerebral or peripheral vascular disease (PAOD), certain systemic diseases such as Amyloidosis or Sarcoid, severe fixed pulmonary hypertension (pulmonary hypertension) as well as current heavy nicotine, alcohol or drug abuse. A lack of ability to cooperate (Compliance), which suggests that the responsible approach to one's own health and compliance with the requirements after the operation is not sufficiently guaranteed, is considered a contraindication.
Complications
In the case of the complications of a heart transplant, a distinction must be made between those of the actual operation, which the foreign organ can trigger, and those which can arise from immunosuppressive therapy. The surgical risks are similar to those of other operations, including bleeding, infections, thrombosis / Pulmonary embolism and, in rare cases, death of the patient.
A very important aspect of the transplantation of a foreign organ is that Rejection reactions. To avoid this, the patient is given permanent immunosuppressive treatment. However, rejection reactions can occur. A distinction is roughly made here between the acute and the chronic Rejection reaction, whereby the chronic rejection reaction occurs later and is often much less noticeable.
The acute reaction can be through among other things fever, Malaise, decreased resilience, weight gain due to water retention (Edema) and irregular heartbeat (Cardiac arrhythmias) to make noticable. Therefore, temperature, pulse and weight should be measured and noted daily. Furthermore, after the transplant, follow-up examinations often take place at the beginning, during which, among other things, blood is drawn and examinations such as EKG (Electrocardiography), Cardiac ultrasound (Echocardiography) and Heart muscle biopsy (Sampling of a small piece of the heart muscle). This allows rejection reactions to be recognized in good time and treated by adapting the immunosuppressive therapy.
The drugs that are taken to suppress the body's immune system have side effects that should not be underestimated. In particular, the risk of infection is increased because the body is prevented from reacting as strongly as it normally does to invading pathogens. Usually a triple therapy is used, which regularly includes ciclosporin and prednisolone.
Other side effects of ciclosporin include high blood pressure (hypertension) and the development of cancer over the course of a few years. Under the therapy with prednisolone it can besides the increased susceptibility to infections among other things osteoporosis, Weight gain, developing a Diabetes mellitus, Muscle weakness, depressions, Gastrointestinal ulcers, high blood pressure (hypertension), glaucoma (glaucoma) and cataracts (cataract) come.
What are the special features of children?
Heart transplantation is particularly important in children, as some heart diseases or malformations are the only therapeutic option to enable the child to survive. If the operation is successful, the children can in most cases develop normally and lead normal lives. The resilience is usually not restricted either. However, rejection reactions may damage the donor heart over time, so that in some cases a new heart transplant may have to be performed. The waiting time for a donor heart for children is on average 180 to 200 days. Heart transplantation in children is an extremely rare procedure. On average, fewer than ten such operations are carried out throughout Germany each year. About 19 out of 20 transplanted children are still alive four weeks after the procedure.
Subsequent therapy & behavioral measures

The goal of a heart transplant is to enable the patient to continue to live as normally as possible. Nevertheless, there are a few things that need to be considered. The attending physician will provide detailed information about this. Only a few aspects are listed below.
The high-frequency check-ups at the beginning should be attended regularly, at the same time the patient should record blood pressure, pulse, temperature and weight as early as possible in order to detect a possible acute rejection reaction as early as possible. Furthermore, the immunosuppressive drugs exactly as prescribed meticulously. The attending physician should be informed about the use of other medications - including those that are available without a prescription in the pharmacy or drugstore due to possible interactions.
As a rule, nothing speaks against a return to work after a phase of convalescence (Gradual restoration of health after illness). Light endurance sports such as brisk running / jogging, cycling and swimming can also be resumed or started for the first time after a few months of the break. Nothing speaks against driving a car, as long as you take sufficient breaks.
With regard to nutrition, it is important to drink sufficient fluids, alcohol should only be consumed in strict quantities. Nicotine should be avoided completely. Adequate hygiene in personal hygiene and in the household should be ensured, as the body reacts significantly more sensitively to bacteria due to the immunosuppressive treatment. Potted plants are also a breeding ground for microorganisms, so they should be avoided in the household - or at least in the bedroom.
Immunosuppressants can also make the skin more sensitive to light, so sunbathing should be avoided. Also because they lead to the development of Tumors the skin than in patients who have not been immunosuppressive. Opinions differ on keeping pets, cats in particular are due to possible transmission of the disease Toxoplasmosis not safe for the patient.
All in all, after a sufficient period of rest, a normal life should be resumed, but it should always be kept in mind that certain behavioral rules must be followed urgently for your own safety.
What is the cost of a heart transplant?
A heart transplant is an extremely complex and therefore expensive procedure. The cost of a heart transplant in Germany is around 170,000 euros. However, since the procedure is only carried out if there is a medical indication for seriously heart disease patients who cannot be treated otherwise, the costs are borne entirely by the health insurance company.
What is the age limit for a heart transplant?
A heart transplant should only be considered if, in the case of a heart disease that cannot be treated otherwise, the general condition of the patient is stable and the other organs are efficient enough that there is a prospect of a successful outcome. Therefore, an upper age limit for a heart transplant was set, which is currently 70 years. However, this is what is known as the biological age. This means that the actual signs of aging of the organs must be assessed and taken into account individually for each patient. Ultimately, when considering whether a heart transplant is an option for a patient, an individual decision on a case-by-case basis is always necessary. However, there is no lower age limit for a heart transplant. In the case of some serious heart malformations, surgery as early as possible on newborns and young children is the only chance for survival.