Liver transplant

The liver is one of many vital organs in humans. In addition to many important metabolic functions, their tasks also include detoxifying the body.
If the patient becomes terminally ill, a healthy liver transplant is often the only way to save the patient's life.
In liver transplantation, the diseased liver is removed and a healthy liver from a deceased organ donor or parts of a liver from an organ donor are used. The goal of liver transplantation is that the newly inserted liver can take over all functions.
In Germany, around 900 liver transplants are performed each year.

What are the requirements for a liver transplant?
There are requirements that must be met in order to be eligible for a liver transplant.
First of all, the liver must be so diseased that the liver cannot regress.
The liver disease can be congenital or acquired.
Liver disease must require a liver transplant.
If a liver transplant has already taken place in the past, there must be chronic transplant failure in the long-term in order to be placed on the waiting list for a transplant again.
The liver diseases that make a liver transplant necessary are often advanced liver diseases that
- cause liver cirrhosis (primary biliary cirrhosis, primary sclerosing cholangitis, alcohol-toxic liver disease, chronically active viral hepatitis, etc.),
- malignant liver tumors,
- congenital malformations of the liver (extrahepatic bile duct atreisie),
- Metabolic disorders (Wilson’s disease)
- or acute liver failure due to viral hepatitis, poisoning or medication (e.g. paracetamol poisoning).
How do you get on the waiting list?
In order to be placed on the waiting list for a liver transplant, the above requirements must be met.
The affected person has to suffer from a non-reversible disease of the liver, which makes a liver transplant necessary.
The treating hepatologist makes the decision to be added to the waiting list. A hepatologist is a specialist in internal medicine, more precisely in gastroenterology, who specializes in the liver and biliary tract.
The hepatologist usually discusses the liver transplant with the performing liver surgeon and the patient.
This means that a specialist from a transplant center takes care of putting the person on the waiting list.
Transplant centers can be found in various hospitals across Germany and they specialize in various organ transplants.
The doctor gives the necessary patient data to the Eurotransplant (ET) agency.
Eurotransplant evaluates the data and decides whether a transplant is considered necessary.
The evaluation of the transplantation is based on a number of different criteria that apply equally across Europe.
What does a liver transplant cost?
The cost of a liver transplant is paid for by the recipient's health insurance company.
This includes the costs for the surgical procedure as well as the pre- and post-treatment.
The cost of a transplant can be up to 200,000 euros.
Indication - factors that may make liver transplantation necessary
The most common reason for a liver transplant in Germany is a previous chronic disease of the liver, liver cirrhosis. This is mainly triggered by:
- Alcohol abuse
- Chronic viral hepatitis
- Autoimmune hepatitis
- Primary biliary cirrhosis
- Primary sclerosing cholangitis (Inflammation of the bile ducts)
- Metabolic diseases
- Liver cancer
- Fulminates Liver failure e.g. after poisoning
Children may also need to Liver transplant exist e.g. at:
- Congenital biliary obstruction (most common cause in children)
- Congenital liver fibrosis (scarring of liver tissue)
- Hereditary metabolic diseases
Contraindications - factors that speak against a transplant
- Blood poisoning
- Severe concomitant cardiopulmonary diseases
- Persistent alcohol consumption (if a patient needs a new liver due to alcohol abuse, it must first be dry for at least 6 months before it can be considered for the operation)
- Tumors in other organs
Can a liver transplant be performed in the event of metastases?
There are tumors that cause metastases in the liver.
Colon cancer, for example, more often leads to the development of inoperable daughter tumors in the liver.
However, a liver transplant comes with risks.
It is a major operation that involves suppressing the immune system (immunosuppression) to prevent rejection of the organ.
Whether a liver transplant makes sense in the case of metastases must be discussed individually with the attending physician.
Read when and where immunosuppressants are still used and what side effects they have: Immunosuppressants - Areas of Use & Side Effects
Is there an age limit for a liver transplant?
There is no age limit for a liver transplant.
This means that older people and children are basically also eligible for a liver transplant.
Nevertheless, the same conditions apply to older people as to younger patients.
However, the German Transplantation Act states that the prospect of success must be taken into account for inclusion on the waiting list.
Among other things, this means the survival of the organ recipient, long-term liver function and the change / improvement in quality of life.
Survival is influenced by comorbidities.
If there is pronounced heart failure, this can have a negative impact on life expectancy.
Older people are relatively more likely to suffer from comorbidities than younger patients.
Can you have a liver transplant on a baby?
There are babies born with a congenital malformation of the liver and bile ducts.
You can have a liver transplant on babies.
There is the possibility of a living donation and an external donation.
With a living donation, a piece of liver tissue from a relative is surgically inserted into the sick baby.
In the case of an external donation, the child is transplanted with a donor liver from a deceased person.
For a liver donation, the blood group and anatomical conditions must match.
Nowadays, the chances of success in newborns and infants for liver transplantation are good.
There are pediatric transplant centers capable of transplanting necessary organs to the smallest newborn.
procedure
If the indication for Organ transplant the patient is placed on a waiting list for a donor organ. The waiting time can vary widely, often it takes months to years until a suitable donor organ is available.
Once a donor organ has been found, it is important that the operation be performed transplantation takes place as quickly as possible, as the functionality of the removed organ deteriorates quickly. The liver must be implanted in the recipient within 16-24 hours of removal from the donor.
Selection of donors
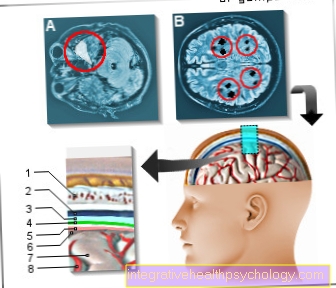
In Germany, organ donation is only permitted after documented brain death and the donor's consent (e.g. by a Organ donor card) allowed (Transplantation Act 1997). In Europe, the Eurotransplant headquarters in the Netherlands handles the transplant assignment. The donor organs are distributed to the patients according to urgency, the decisive factor here is how high the remaining functionality of the diseased liver is. Accordingly, patients with fulminant liver failure or intensive therapy receive the highest level of urgency.
The operation

In contrast to e.g. Kidney or pancreas transplants, liver transplants are so-called orthotopic transplantwhich means that the new organ will be put in place of the old diseased organ.
First, a large abdominal incision is made, thus opening up the abdominal cavity for the surgeon. The first thing to do is to remove the old liver. To do this, the liver is carefully detached from the surrounding tissue and the supplying and draining vessels are exposed. Next, the bile duct is cut as close as possible to the liver.
In the next step, the blood vessels in the liver are clamped off. The liver is well supplied with blood and receives its blood through the Portal vein (a large blood vessel that draws all of the blood from the digestive organs to the liver). The blood is passed through the liver and leaves it again via the inferior vena cavawhich carries the blood to the heart. The liver also has its own blood supply via the hepatic artery. These 3 vessels (portal vein, inferior vena cava and hepatic artery) have to be clamped off in order to remove the old liver and avoid losing any blood.
If the 3 blood vessels are clamped, the liver is separated from the bloodstream and can be removed. To do this, the surgeon cuts the clamped vessels at the level of the liver. The liver is now exposed and can be removed from the body.
Then the donor organ is started to replace the old liver. For this purpose, the donor liver is connected to the patient's blood vessels (portal vein, vena cava and hepatic artery). First, the vena cava of the new liver is connected to the clamped vena cava of the patient, then the portal vein and hepatic artery as well.
If all vessels are well adapted to one another, the previously clamped vessels can be released again, so that the liver is supplied with blood again. Now that blood is flowing through the liver again, it is important to pay attention to whether there is any small bleeding anywhere, especially in the newly connected vessels.
When all bleeding has stopped, the last thing that is connected is the bile duct of the donor organ with that of the recipient.
At the end of the operation, before the abdomen is closed again, drains are placed in the area of the newly operated Vascular connections used. These are used to drain blood, pus or wound secretion from the abdominal cavity into a container outside the body in order to promote wound healing.
Duration of the operation
In a liver transplant, the abdomen is opened, the diseased liver is removed and the new liver is implanted.
The operation takes between four and eight hours.
The duration of the operation can vary, as certain circumstances and complications can complicate or prolong the operation.
With cirrhosis of the liver, portal hypertension and coagulation disorders can prolong the procedure.
If there is a misunderstanding of the size of the transplanted bile ducts between the donor and recipient, surgical techniques that are more time-consuming may be necessary.
With an operation lasting four to 8 hours, a liver transplant takes on average longer than a heart or kidney transplant.
forecast
After a successful operation, it must be seen whether the body accepts the donor organ or recognizes it as foreign and then rejects it. The average length of stay in acute facilities after a liver transplant is around 1 month. To prevent rejection of the newly transplanted liver, immunosuppressive therapy (Immunosuppressants) necessary, which means that you can medicate the body's own immune system suppressed to give the body time to get used to the new liver. Even after a successful transplant, lifelong immunosuppressive therapy is necessary.
The survival times after liver transplants are increasing steadily. In the early 1980s, around 70% of liver transplant recipients were still alive, today it is over 90%. And even after 5 years, the survival rate is still around 75%, but this is heavily dependent on other diseases of the patient in addition to the liver disease and the cooperation and compliance with the strict therapy scheme.
How long does the entire healing take?
The patient spends the first few days after the procedure in the intensive care unit.
Often the patient can get up after 3 to 5 days.
Early mobilization is good for the person concerned.
After observation in the intensive care unit, the patient remains in the normal ward for one to two weeks.
This is usually followed by a stay in a rehabilitation clinic.
Immunosuppressants are taken so that the immune system does not attack the new organ.
The liver will be checked closely in the first few weeks and months after the procedure.
After all, the new liver should begin its tasks and functions in the first few months after the transplant.
The entire healing process takes several months and depends on the patient's condition and concomitant diseases.
What is the life expectancy with a liver transplant?
Life expectancy is getting better and better for liver transplant recipients.
Most people who need a liver transplant will have had a long history of illness at the time of the transplant.
Most of those affected have severe liver insufficiency before the transplant and are therefore dependent on frequent visits to the doctor and hospital stays.
A liver transplant means taking certain precautions and continuing medical care.
Life expectancy is significantly better when patients accept the new liver as their own.
The technology and research in immunotherapy are constantly improving.
This means that life expectancy is getting better and better.
Today, the one-year survival rate for liver transplants is greater than 90%, the 5-year survival rate is greater than 80%, and the 10-year survival rate is greater than 70%.
This means that a liver transplant is generally associated with a very good life expectancy.
The survival rates are nevertheless strongly dependent on the underlying disease and the overall condition of the patient.
Concomitant and secondary illnesses can have a negative impact on life expectancy.
Quality of life after liver transplant
Most patients who get through the operation and the months after it without Rejection reaction or uncontrollable infections, achieve full rehabilitation.
Studies have shown that approx. 85% of the survivors of a liver transplant can be easily reintegrated into everyday work. In addition, numerous cases have already been documented in which women became pregnant after a successful liver transplant and gave birth to a healthy child on time.