Spinal osteoarthritis - how is it treated?
introduction
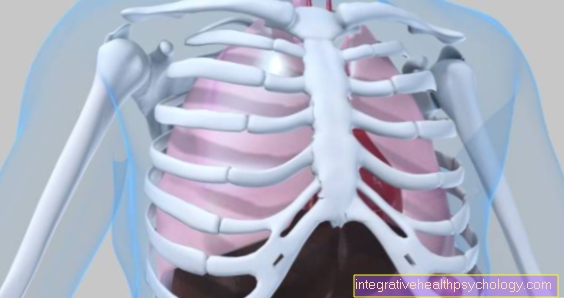
Osteoarthritis is a degenerative change in bones and cartilage.
Spinal osteoarthritis can affect the entire spine or just parts of the spine.
Usually the lower parts of the spine (lumbar spine) are more degeneratively changed than the upper parts because they have to carry a greater weight.
For example, due to a herniated disc and the loss of articular cartilage, the bone is no longer adequately protected.
Often, with pronounced osteoarthritis, bone rubs against bone, causing wear and tear of the bone substance.
Also read our related article: Facet Syndrome - What Can You Do?

What is the medical term?
There are various medical terms for spinal osteoarthritis.
If the entire spine is affected, it is also known as facet joint arthrosis.
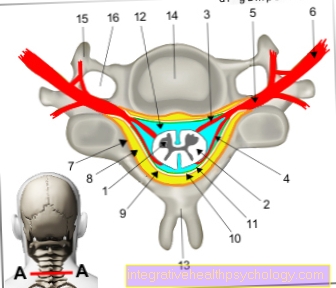
The individual vertebral bones meet at several points, and each individual joint between the bones contributes to the overall mobility of the spine.
This is why spinal arthrosis is also referred to as arthrosis of the facet joints.
The term spondylarthrosis is also used to describe osteoarthritis changes in the spine.
In addition, a classification according to localization (cervical, thoracic, lumbar spine) is possible.
If it occurs only in the lumbar spine, one speaks of spondylarthrosis of the lumbar spine.
Spinal osteoarthritis of the cervical spine
Arthrosis in the cervical spine are usually degenerative and therefore occur more frequently with age.
In addition to back and neck pain, headaches and dizziness can also occur.
It is also possible for the pain to radiate into the arms and shoulders.
The disease is diagnosed using mobility tests in the cervical spine.
Functional failures such as sensory disorders and muscle weaknesses in the arms can also be indications of spinal osteoarthritis of the cervical spine.
In order to be able to make the diagnosis certain, an x-ray is usually made, in which typical bone damage from osteoarthritis in the cervical vertebrae can be seen.
In order to rule out damage to the intervertebral discs, spinal cord and nerves, an MRI or CT scan can also be performed.
Treatment is usually done with pain killers.
In addition, many movement exercises should be performed, especially in the neck area.
Strengthening the neck muscles is also aimed at.
However, good mobility of the cervical spine is particularly important for everyday life.
An operation is usually not performed because the benefit is rather small compared to the possible complications (damage to nerves and the spinal cord with the risk of high paraplegia).
Spinal osteoarthritis of the lumbar spine
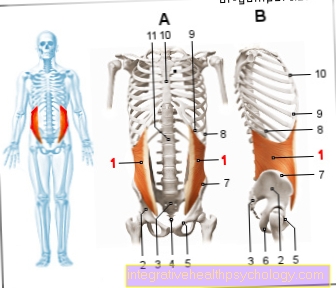
Spinal osteoarthritis in the lumbar spine is the most common of all arthrosis localizations on the spine, as the lumbar spine bears the greatest weight.
In addition, many movements that are not carried out in a back-friendly manner put a strain on the lumbar spine in particular.
Typically, pain occurs in the lower back.
They can radiate into the abdomen, buttocks and legs.
Muscle weaknesses and sensory disturbances can also be symptoms, as arthrosis can damage nerves.
Read more on the topic: pain in the back
The physical exam tests the mobility of the lumbar spine.
An X-ray is used to make the final diagnosis of the disease.
Since the lumbar spine is a very stressed area of the spine, the therapy focuses on strengthening the back muscles.
Lifting heavy objects should be avoided.
Rotational movements of the upper body against the legs also worsen the situation.
In addition, of course, appropriate pain therapy should be provided.
In comparison to the rest of the spine, the lumbar spine is operated more frequently.
Here, reducing pain is usually more important than maintaining complete mobility.
Therefore, individual vertebral joints can be stiffened.
This reduces the load on the arthritically altered vertebral bones, while still maintaining good everyday mobility.
This is how the treatment / therapy takes place
The therapy of spinal osteoarthritis is usually purely symptomatic.
A distinction is made between conservative (non-surgical) and surgical therapy.
Both treatment methods aim to reduce pain.
Conservative therapy consists of drug-based pain therapy and exercise therapy.
The pain medication is divided into three classes, which are used depending on the severity and duration of the symptoms.
The classic pain relievers such as aspirin, diclofenac, ibuprofen, paracetamol and metamizole belong to the lowest class.
They are mostly taken as tablets / drops or applied as pain relief ointments.
The next level includes the low-potency (less effective) opioid pain relievers dihydrocodeine, tilidine and tramadol, which are usually taken as tablets.
The highly potent opioid pain relievers buprenorphine, fentany, hydromorph, morphine and oxycodone are most effective.
They are also available as tablets, but pain plasters or injections are often used.
Physiotherapy is also carried out to strengthen the back muscles.
Furthermore, the goal is to create or maintain functional mobility that ensures suitability for everyday use.
Alternatively (and rarely) surgery is performed.
The pain-conducting nerve fibers on the spine are sclerosed with heat or cold.
In this way, no pain signal can reach the brain and a pain-free interval of around 2 years can be achieved.
For more information on the pain relievers listed, read the appropriate articles below Medicines A-Z.
Which exercises can help?
Although exercise is one of the risk factors for spinal osteoarthritis, it is also a great protective factor for the joints.
The decisive factor is the dose and the type of sport.
So-called high-impact sports, which are associated with many impacts, promote the development of osteoarthritis.
In contrast, most endurance sports are considered joint protection.
These include walking and Nordic walking, cross-country skiing and swimming.
Cycling and running depends on the nature of the ground and the cushioning of the bike or running shoes.
Excessive impacts on the spine have a pro-arthrotic effect.
Slight movement stimulates the bone to form better and more stable cartilage substance, which in turn protects against osteoarthritis.
In addition to swimming and cross-country skiing, where cardiovascular, endurance and back muscles are trained at the same time, back-strengthening exercises are also helpful. On the one hand, the muscles that hold the back are strengthened, which leads to less stress on the spine.
On the other hand, mobility improves, even if there is already back pain.
Movements relevant to everyday life can be specifically trained.
Anyone who works on it with a physiotherapist can also learn new movements that can be carried out painlessly and possibly replace painful movements.
As back pain is practically a widespread disease, many fitness studios offer back courses that carefully build and strengthen the muscles.
When do you need an operation?
Surgery for spinal osteoarthritis is rather rare and should only be used if conservative treatments are not sufficient.
Indications for an operation are, for example, pain that can no longer be adequately treated.
In this case, pain fibers can become obliterated so that no pain signal is heard any more.
Also nerve damage such as sensory disturbances and failure of certain muscles make an operation necessary.
In particularly severe cases, the nerve damage can also manifest itself in the form of bladder or bowel problems.
This can be an indication for an emergency operation and is more likely to occur with traumatic injuries than with spinal osteoarthritis.
This is the prognosis for spinal osteoarthritis
Osteoarthritis of the spine is a progressive disease, the progression of which cannot be stopped over the years.
However, the process can be slowed down and / or stopped temporarily.
Overall, the increasing pain usually leads to a decrease in mobility.
As a result, the quality of life decreases.
Osteoarthritis in itself does not affect the life expectancy of those affected.
However, falls due to poor mobility and cardiovascular diseases (due to years of pain-related lack of exercise) can be life-shortening consequences of spinal osteoarthritis.
Course of the disease
Spinal osteoarthritis usually develops over years before it causes symptoms for the first time.
Then comes the so-called early stage.
During this time, pain usually occurs in individual vertebral joints.
The lumbar spine is affected much more often than the cervical spine, as it bears more weight.
As a rule, a lot of protective cartilage is still preserved, but there is also slight damage to the vertebral bone.
After several years or even decades with increasing cartilage and bone damage, the disease finally comes to a late stage, in which virtually no cartilage is preserved and massive bone changes exist.
What degree of disability do you get for spinal osteoarthritis?
The degree of disability (GdB) that you get for spinal osteoarthritis depends on how restrictive the disease is.
Slight complaints without functional restrictions qualify for GdB 10.
GdB 20 to 40 is awarded in the event of slight loss of functionality.
Moderate restrictions lead to GdB 50 to 70 and functional losses and a highly progressive disease are the basis of a GdB 80 to 100.
Applying for the GdB is often tedious, the applications are usually rejected at the beginning.
Those who persistently object, however, usually have success.
Causes of spinal osteoarthritis
The term spinal osteoarthritis always describes a degenerative disease, i.e. a disease that occurs due to wear and tear.
In most cases, osteoarthritis is age-related.
However, there are also risk factors such as heavy physical work or so-called high-impact sports, in which the spine has to carry a lot of weight and has to cushion many shocks.
This leads to faster wear of the intervertebral discs.
These can no longer adequately perform their protective buffer function.
This puts a higher pressure on the cartilage layer, which additionally protects the vertebrae.
After a certain period of exposure, this is also worn off, and now the bone itself is loaded.
Therefore, after a course of several years, it usually happens that the vertebral bones themselves rub against one another because all protective layers have already disappeared.
In addition to wear and tear due to age and physical strain, injuries to the spine can also promote the development of spinal osteoarthritis. In particular, traumatic injuries in accidents that are associated with broken bones and thus possibly cause misalignments in individual vertebral joints lead to the development of spinal osteoarthritis.
Usually the joints around the affected vertebral body are arthritically changed at first, but later the osteoarthritis also spreads to the other joints, as the stress situation here also changes due to the malposition.
What accompanying symptoms are there?
The spinal osteoarthritis mainly manifests itself as pain in the spine.
In the initial stage one speaks of so-called starting pain.
These occur in the morning after getting up.
If the spine suddenly has to bear the weight of the body again, the individual vertebral bodies are pressed more closely together.
When moving, they shift against each other, which can lead to pain.
Apart from this start-up pain, affected people are usually symptom-free at rest.
The pain typically occurs with movement and strain, as the vertebral joints are particularly stressed.
If the entire spine is affected by osteoarthritis, the pain usually first manifests itself in the lumbar region, as this is where the greatest weight has to be carried.
Over time, the degenerative changes move upwards until the entire spine is causing problems.
In addition, the back pain usually leads to increased tension in the back muscles, which means that the tension-related pain spreads across the entire back.
In addition to cartilage and bone damage, spinal osteoarthritis can also affect nerve fibers.
Therefore symptoms such as shooting nerve pain can also occur.
They typically radiate from the lumbar spine into the buttocks and thighs.
From the cervical spine, the arms, shoulders, neck and back of the head are more likely to be affected.
Back pain
The back pain in spinal osteoarthritis can initially be explained by the degenerative changes.
Due to the wear and tear of the intervertebral discs and cartilage, the vertebral bones are not adequately protected, the sensitive periosteum is irritated and causes back pain that is dependent on stress.
In addition, the vertebral bones rub against each other, causing small fragments of bone to loosen.
These remain in the joint space and increase bone wear there, which accelerates the formation of arthrosis.
The back pain is not only due to the bone damage.
The initial pain leads to tension in the back muscles.
After a certain time, this tension affects the entire back, regardless of where exactly the osteoarthritis is in the spine.
This creates a vicious circle, as tense back muscles offer less protection against new impacts that further exacerbate osteoarthritis.
In spinal osteoarthritis, back pain is made up of two components: the local pain in the arthritic changes in the vertebral joints and the generalized back pain due to the reflexively tense back muscles.
Also read about the treatment options for chronic back pain:
Therapy for chronic back pain - what works best?
Nerve pain
Often the intervertebral discs or the loss of the intervertebral discs are the cause of spinal osteoarthritis.
For example, a herniated disc can lead to the vertebral bones colliding immediately and developing osteoarthritis.
At the same time, the intervertebral disc presses on the spinal cord and causes nerve pain.
Due to the arthritic changes themselves, the joint space between the vertebral bodies is reduced.
The nerves at their exit points can be pinched or irritated.
Nerve pain is typically pulling pain that radiates into the supplying areas (leg, buttocks or arm and shoulder).
This is how the diagnosis is made
The diagnosis of spinal osteoarthritis consists of a specific anamnesis and a physical examination that assesses the mobility of the spine. In addition, the functions of the nerves must always be tested.
Attention is paid to functional losses in the muscles or sensory disorders.
Imaging is also part of the diagnosis.
Usually you first take an X-ray overview.
For specific questions (for example whether a disc or a nerve is affected), CT or MRI images can also be made.