Regional anesthesia
introduction
Anesthesia is generally a condition in which no pain can be felt.
This state is required, for example, in the context of operations.
As a rule, the anesthesia, i.e. the insensibility or painlessness, is brought about by an anesthetist, a specially trained doctor.
When it comes to anesthesia, a distinction is made between general anesthesia and regional anesthesia.
General anesthesia is also known as general anesthesia and differs from regional anesthesia in that, in addition to inhibiting pain perception, it also causes a loss of consciousness.

Regional anesthesia, also known as local anesthesia, is instead characterized by a loss of pain sensation while remaining conscious.
Depending on the type of procedure or operation, either general anesthesia, regional anesthesia or both procedures can be used to induce insensitivity and painlessness.
Which procedure is chosen depends on the one hand on the duration of the procedure and on the severity of the procedure.
The anesthetist has the task of advising the patient and informing them about which procedure is possible and recommended for him.
The decision as to whether general or regional anesthesia should be performed before the procedure is made by the patient and the doctor together.
Procedure of regional anesthesia
Regional anesthesia is a local form of anesthesia, i.e. an inhibition of pain perception in a specific region of the body while maintaining consciousness.
In order to achieve local anesthesia in a region of the body, the anesthetist injects a drug into the immediate vicinity of a nerve, which normally ensures that pain can be felt in that region of the body.
The medication interrupts the transmission of information from the nerve to the brain and pain can no longer be felt at this point.
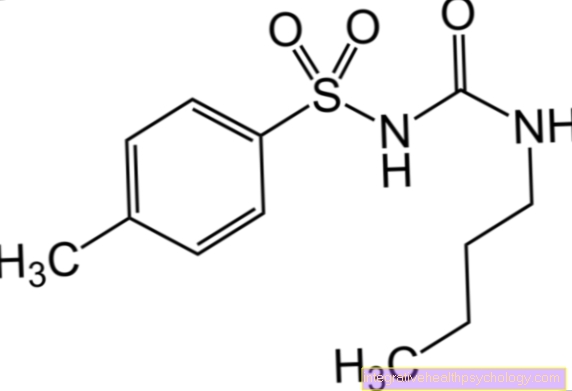
The drugs used in regional anesthesia are called local anesthetics.
Important representatives of this group are lidocaine, ropivacaine and bupivacaine.
The drugs are applied using thin needles or special cannulas. It is important that the puncture site is first thoroughly disinfected so that no pathogens can penetrate.
What is regional venous anesthesia
Venous regional anesthesia is a procedure that is particularly used in outpatient treatment. It is a procedure in which the local anesthetic is injected directly into the vein and from there it is distributed throughout the tissue. Since the local anesthetic must never get into the systemic bloodstream, the blood supply is blocked.
First the arm or leg is raised and the blood is pressed out of the vessels through tight bandages. When the desired area is almost bloodless, a blood pressure cuff or tourniquet is attached to the top to prevent further blood flow. The local anesthetic is then injected into the veins and takes about fifteen minutes to take full effect. The duration of the procedure is limited to less than an hour, as the arm or leg must then be supplied with oxygen-rich blood again.
Venous regional anesthesia is considered a procedure with few complications. A commonly reported side effect is the pain when the blood supply binds. In rare cases, the local anesthetic enters the systemic bloodstream and can cause serious complications such as seizures, cardiac arrhythmias, and respiratory paralysis. This happens especially when the blockage is not tight enough or is released too early. Venous regional anesthesia should not be used for known vascular diseases.
What is peripheral regional anesthesia
The word peripheral generally means removed from the trunk of the body. Peripheral regional anesthesia therefore encompasses all procedures that apply to individual nerves or nerve plexuses away from the spinal cord. These include the foot block, finger block, plexus anesthesia and many other procedures.
The word plexus anesthesia is derived from the Latin word plexus, the plexus of nerves. In the context of a plexus anesthesia, a whole network of nerves is numbed, which can be visited beforehand using a nerve stimulator. Such nerve plexuses are found on the arms, in the lumbar region and on the tailbone.
Read more on the topic: Brachial plexus anesthesia
The underlying system is always the same. The local anesthetic is injected near a supplying nerve and the signal transmission is interrupted at this point. This interruption point can be in the immediate vicinity of the operating area, as in the case of Oberst's finger block, or also well away from this area, as in the case of plexus anesthesia in wrist operations. In the second variant, the operating area is on the wrist and the anesthesia is placed at the level of the armpit or neck.
A very common procedure is surface anesthesia. Here, the numbing drug, the local anesthetic, is applied to the skin in the form of a spray (For example, to facilitate the placement of indwelling cannulas in hospitals) or on mucous membranes (for example with painful inflammations in the mouth and throat area) and numb the smallest superficial nerves.
Another form of regional anesthesia is infiltration anesthesia, which is used in particular by dentists. The local anesthetic is injected into the tissue, for example into the oral mucosa, with the help of a fine needle. The active ingredient then gradually mixes with the tissue and numbs the fine nerves inside.
The local anesthetic can be given as a single injection or through a catheter. The catheter allows for easy re-injection of medication if the procedure takes longer. Peripheral regional anesthesia is associated with fewer side effects than spinal anesthesia and general anesthesia.
Implementation on the arm
Regional anesthesia can be performed on the arm at different levels. The planned site is disinfected and the anatomical structures are visited. An ultrasound device can be used to support this. The cannula is inserted through the skin near the nerve and the local anesthetic is injected. Before the injection, the plunger of the syringe is pulled back a little and the doctor tests whether blood flows back. After about fifteen minutes, the desired area should be numb and no longer feel pain.
What is a hand block
The hand block is a regional anesthetic procedure in which all relevant nerves in the hand above the wrist are numbed. The hand becomes completely numb, but some muscle functions are retained. The nerves responsible are the radial nerve, the ulnar nerve, and the median nerve, so three separate injections are required. The hand block is used for small operations or for wound care of the hand and fingers. The hand block starts to work after just a few minutes and lasts for around two hours.
What is regional anesthesia near the spinal cord
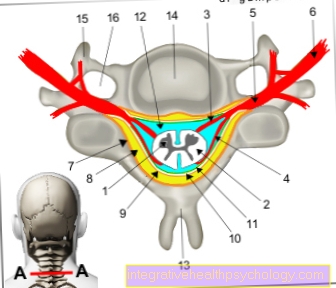
In anesthesia procedures close to the spinal cord, the local anesthetic is injected into the vicinity of the spinal cord and takes effect directly on the nerve roots. A distinction is made between epidural anesthesia, also called PDA, in which the drug is injected over the hard skin of the spinal cord, and spinal anesthesia, in which the drug is injected directly into the liquor space.
The two procedures differ in the depth of penetration into the so-called spinal canal. The spinal cord is located in the spinal canal, where it is embedded in nerve water. Over this spinal canal there is a layer of connective and fatty tissue, which is known as the epidural space.
In spinal anesthesia, the cannula penetrates to the spinal canal and the local anesthetic is introduced there. In the spinal canal, the local anesthetic mixes with the nerve water, numbing the entire lower half of the body.
With epidural anesthesia, the needle only penetrates into the epidural space. Here the local anesthetic mixes with the fatty tissue and mainly causes an anesthetic of the nerve roots at the level of the puncture point of the cannula.
The great advantage of epidural anesthesia is that a longer catheter can be used for postoperative pain relief.
The spinal anesthesia has a faster onset of action. The two methods can also be combined. Examples of operations under epidural anesthesia are gastrointestinal tract operations, hip implant changes and obstetrics. The latter takes advantage of the fact that different types of nerves react differently to local anesthetics. The pain is already switched off while the muscles are still working.
Spinal anesthesia is used, for example, for caesarean sections, pelvic operations and foot operations. Depending on the duration of the operation, different local anesthetics such as bupivacaine or mepivacaine are used.
Read more on the topic:
- Complications of epidural anesthesia
- Complications of spinal anesthesia
- Spinal anesthesia during a caesarean section
What is a saddle block?
The saddle block is a special form of spinal anesthesia. The sacral segments of the spinal canal are particularly affected. A distinction is made between the real saddle block, also called breeches anesthesia, and the extended saddle block, which also reaches the lumbar segments. The real saddle block is used in proctology, gynecology and obstetrics, as well as urology, as it numbs the anus, perineal area, pelvic floor muscles and the external genitalia. Operations on abdominal organs are only permitted with the extended saddle block. It is a relatively safe procedure with side effects similar to normal spinal anesthesia, but these side effects are mostly mitigated.
Further information on this topic can be found at: Saddle block - a special form of spinal anesthesia
Ultrasound-assisted regional anesthesia
The exact position at which a local anesthetic should be injected is not always easy to find. With an ultrasound device, the anesthetist can assess exactly where the nerves and blood vessels are. This increases the safety of regional anesthetic procedures, as the local anesthetic is less likely to get into the blood vessels and the nerves can be anesthetized better. The ultrasound device is most often used for regional anesthesia in the groin region or on the arm plexus, since there the nerves are relatively deep in the tissue and a lot of other tissue can be in the way.
Read more on the topic:
- Brachial plexus anesthesia
- Femoral catheter
Regional anesthesia despite anticoagulation?
Anticoagulation always increases the risk of bleeding and can lead to increased bruising after injections of any kind. However, since these drugs are an important prophylaxis against strokes, heart attacks and similar diseases, discontinuation should always be carefully considered.
Particularly with spinal or epidural anesthesia, anticoagulants can cause serious complications. There are many different active ingredients that are classed as anticoagulants. The risk is different depending on the drug. Some anticoagulants only need to be stopped for a few hours prior to regional anesthesia. These include heparins and argatroban. ASS does not have to be stopped at all.
Withdabigatran, rivaroxaban, danaparoid and other drugs, discontinuation is necessary for a few days.
Some anticoagulants must be paused a week before the procedure. These include, for example, clopidogrel and ticagrelor.
Even after the procedure, certain minimum times must be observed before anticoagulation can be started. Basically, anesthesia procedures with anticoagulation remain individual decisions and depend on many factors.
Complications
Complications in regional anesthesia procedures are very rare these days due to modern techniques and hygienic standards.
Side effects that can occur in the context of regional anesthesia are in particular one Drop in blood pressure.
The patient is having an operation with a monitor connected, which can continuously record blood pressure values and heart actions.
In the event of a drop in blood pressure in the context of regional anesthesia, the anesthetist can react immediately and counteract this with the help of medication.
In some cases, the area where the medication used to numb the nerve or plexus was injected with a needle may become too Bleeding or to Formation of bruises come.
In addition, in rare cases it can be too Infections come with different pathogens.
In rare cases, the injected drug itself can also cause side effects. These include dizziness, inner unrest, Cardiac arrhythmias or Seizures.
Due to the further development of the drugs used in regional anesthesia, there is also another side effect that allergic reaction, become rare.
However, if there is an allergic reaction to the injected drug, it is a absolute warning signal for the anesthetist, as there is a risk of a allergic shocks consists.
Allergic shock is a medical emergency.
The allergic shock can cause discomfort in different parts of the body, such as skin, respiratory tract, or the Cardiovascular system cause and is potentially life threatening.
If an allergic shock occurs as part of regional anesthesia, the pain-relieving drug must be administered interrupted immediately and measures are taken to stabilize the patient's circulation.
There is also the possibility that the needle or cannula could damage the nerve directly.