Circulatory disorders
Synonyms in a broader sense
Perfusion disorder
English: circulatory disorder, impaired circulation, circulation disturbance, disturbance of (the) blood supply
definition
Circulatory disorders are an obstruction to blood flow, which means that the tissue behind the affected area is not adequately supplied with oxygen and nutrients.
Since oxygen is vital for each of our organs, performance is more or less reduced by a lack of oxygen. The brain can only survive a few minutes without oxygen, whereas the kidneys or liver can survive for a few hours without oxygen without suffering permanent damage.
Circulatory disorders can arise when a vessel is blocked or even narrowed. Since the vessels lose more and more elasticity with increasing age, it is understandable that circulatory disorders develop primarily in old age. In addition, there are various risk factors that become more and more noticeable with increasing age.

Epidemiology
The occurrence of circulatory disorders becomes more and more likely with increasing age. Up to the age of 45, only about 2% of the population suffer from a circulatory disorder, around one in ten of the 60 to 70 year olds is affected by this disease, with men about 4 times as likely to get the disease as women of the same age. However, these data only apply to the western world; in other countries, especially in developing countries, there are far fewer people affected, which is mainly due to lifestyle and the associated risk factors (see below).
causes
There are many causes for circulatory disorders, of which only the most important are described in more detail here.
The reasons include above all narrowing or occlusion of arteries, which can result from hardening of the arteries (arteriosclerosis), vascular occlusions (embolisms) or the formation of blood clots within the artery. Other causes include inflammation of the blood vessels (vasculitis), cramps in the muscles of the blood vessels (vascular spasms), blood pressure that is too low (arterial hypotension) or sudden bleeding (for example cerebral hemorrhage).
Probably the most common cause of a circulatory disorder is hardening of the arteries (e.g. calcified carotid artery), which is a systemic disease. Various vessels can become calcified, e.g. with increasing age, the likelihood of arterial calcification increases. In the context of arteriosclerosis (literally translated: connective tissue hardening of the arteries), deposits occur on the inside of the vessels. Initially, small injuries in the vessel wall are probably responsible for this. In response to these injuries, the body switches on the immune system.
A number of complicated biochemical processes then come into force, resulting in blood cells, blood lipids, connective tissue and, in some cases, also lime deposits being deposited in the vessels. These substances are often referred to as "plaques". In principle, these deposits can occur anywhere in the arterial system. However, since flow conditions play a role in the formation of plaques, arteriosclerotic occlusions are preferably found where vessels branch and the uniform flow is impeded.
Read more on the topic: arteriosclerosis
As a rule, circulatory disorders do not arise immediately. The deposits grow more and more over time, whereupon the diameter of the arteries steadily decreases. So the body has a lot of time to react to the vascular changes. So it happens that on the one hand smaller blood vessels now mainly take over the blood supply, which previously played a subordinate role and on the other hand so-called bypass circuits are formed (Collateral circuits) around the affected areas. This is why symptoms often only show up when the arteriosclerosis has progressed massively and the blood flow is extremely restricted as a result.
An embolism occurs when a vessel suddenly becomes blocked, namely by the fact that a blood clot, which may have arisen in a completely different, more distant place in the vascular system, is carried away and gets caught in a mostly smaller vessel and closes it. This embolism is usually triggered by a blood clot (thrombosis), but it can also result from the scattering of tumor tissue, amniotic fluid or even air.
Risk factors
Risk factors for the development of circulatory disorders are high blood pressure, diabetes (diabetes mellitus), obesity, increased blood lipid levels (for example in Hypercholesterolemia and Hyperlipidemia) and sedentary lifestyle. Circulatory disorders are often triggered by smoking. Unfortunately, all of these conditions are not uncommon these days, but almost the rule of our western lifestyle.
Read more on the topic: Circulatory disorders caused by smoking
Symptoms
The symptoms that occur with circulatory disorders vary widely. They are primarily dependent on the location and extent of the circulatory disorders. Many people suffer from cold hands and feet, which is often a mild form of circulatory disorder. A good blood circulation is important so that all organs can be adequately supplied with oxygen and can perform their function in an adequate manner. Since an occlusion usually creeps up on it, regardless of the location of the occlusion, it is characteristic that those affected usually perceive little or no discomfort in the early stages.
Also read the article on the topic: You can recognize a circulatory disorder by these symptoms
Initially, the symptoms often only occur during physical exertion, as this leads to an increased blood requirement. In the case of high-grade vascular occlusions, the symptoms also occur at rest if the occlusion is too strong. Tissues with insufficient blood supply can be seriously damaged if therapy is not carried out. Circulatory disorders in the brain, heart and legs are the most common.
Symptoms on the head
If there is a lack of oxygen as part of a circulatory disorder, this leads to damage to the brain cells, which then die. With regard to the symptoms and the consequences of a circulatory disorder, a distinction is made between short-term and long-term circulatory disorders.
A short-term circulatory disorder in the brain triggers a transient ischemic attack (TIA). As a rule, the associated symptoms last between two to 30 minutes. In the longest case, the symptoms persist for 24 hours and then subside again. Temporary blindness of one eye (amaurosis fugax) is characteristic. The symptoms depend on the affected brain area. Often double vision, indistinct speech, drowsiness, balance disorders, fainting, one-sided paralysis and numbness occur. Such an attack does not correspond to a stroke, but it should be perceived as a warning signal as the likelihood of suffering a stroke in the future is increased. Irreversible circulatory disorders can lead to a stroke. In terms of symptoms, the stroke resembles the transient ischemic attack. However, the symptoms persist for more than 24 hours and in some cases do not resolve at all.
It is also true that the symptoms depend on the affected brain area that is no longer supplied with oxygen. This can lead to paralysis, numbness in arms and legs, speech or vision disorders, ringing in the ears or dizziness. A sudden drooping of the corner of the mouth is typical and noticeable to outsiders. Often the patients are also noticeably confused.
That might be interesting for you too: What are the symptoms of circulatory disorders in the brain?
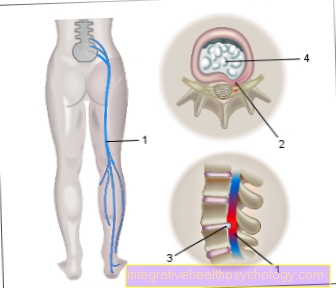
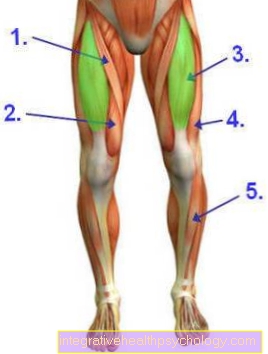
Symptoms on the legs and feet
If there is an acute circulatory disorder in one of the extremities, sudden and severe symptoms follow. Characteristic are the appearance of six different symptoms, the so-called six "Ps". These include: Loss of pulse, pain (pain), paleness and coldness (paleness), sensory disturbances and numbness (paraesthesia), muscle weakness and symptoms of paralysis (paralysis) as well as shock symptoms (prostration) in the sense of palpitations and clouding of consciousness.
If the vascular occlusion is not cleared in time, the leg can die, resulting in amputation. Most of the time, however, the symptoms are rather insidious and then take a chronic course. In this case, one speaks of peripheral arterial occlusive disease (PAD), also known as intermittent claudication. The name intermittent claudication comes from the fact that those affected often have to take breaks from walking due to the chronic circulatory disorders and then often linger in front of shop windows. The term "claudicatio intermittens" is also used for the symptoms, it describes a recurring limping of the patient, since the muscles hurt after a short time when stressed.
Based on the symptoms, PAD can be divided into four stages (according to Fontaine). In the first stage there are vascular changes, but no symptoms appear. In the second stage, pain occurs when exercising. If the pain-free walking distance is longer than 200m, one speaks of stage IIa. If it is shorter than 200m, stage IIb is present. In the third stage, the symptoms also appear at rest, especially at night when the legs are up. In the last stage, stage IV, the circulatory disorders are so severe that tissue damage occurs. Ulcers and wounds heal poorly due to the lack of oxygen and blood components that are responsible for wound healing.
Open legs develop and in extreme cases the tissue dies completely - what is known as a smoker's leg is present, as PAOD usually occurs in heavy smokers. As a rule, both legs are affected, although the symptoms in one leg can also be less pronounced. In diabetics, the symptoms are often different because they perceive the pain later due to disease-related nerve damage, which is why PAOD is often only diagnosed in stage IV. Instead of pain, they often experience a burning sensation.
The symptoms described so far related to the occlusion of arteries. But veins can also be closed or partially closed. This condition is known as venous thrombosis. Depending on the level of the vein occlusion, the whole leg, calf or foot swells because the blood builds up and can no longer be pumped back to the heart. The section under the closed jar turns blue.
PAD (peripheral arterial disease)
The abbreviation PAVK stands for peripheral arterial occlusive disease. This disease describes the narrowing or partial or complete closure of arteries. The severity of the disease is divided into four levels, as the PAD can have very different forms: Both a symptom-free form is possible, which is usually noticed as an incidental finding, as well as great pain when walking, up to the death of certain body parts due to the long-term undersupply of blood and oxygen.
Find out more about the topic at: PAD (peripheral arterial disease)
The most common cause of the development of PAOD is existing arteriosclerosis, i.e. stiffening and narrowing of the arteries due to deposits in the vessel walls. Atherosclerosis occurs particularly with increasing age, but does not necessarily have to lead to PAOD. Other risk factors for arteriosclerosis and PAD are, for example, high blood lipid levels (hypercholesterolemia), smoking, lack of exercise, obesity and diabetes mellitus. In order to treat PAD, it is advisable to change your lifestyle to eliminate the risk factors mentioned above. In addition, drugs that have an anticoagulant effect can be given.In later stages, surgery to treat PAD, such as bypass surgery, can be considered.
Symptoms on the hands
Circulatory disorders can also be limited to the fingers (and toes). In many women in particular, the blood flow to the hands and feet is restricted due to low blood pressure, which manifests itself in cold hands and feet. A typical syndrome of insufficient blood flow to the hand is Raynaud's syndrome. Circulatory disorders occur due to cramping of small vessels, usually as a result of stress or cold. A typical sequence of symptoms occurs.
At first the fingers turn white due to the lack of blood flow. This is followed by a blue coloration due to the lack of oxygen. As soon as the fingers are supplied with blood again, they turn red. One also speaks of the tricolore phenomenon. This process is rarely accompanied by pain. Other symptoms that may occur are a burning sensation in the fingers, tingling, and numbness. Sometimes the symptoms persist for hours and can lead to tissue damage. Raynaud's syndrome can usually be classified as harmless, but it can also occur in the context of other diseases such as collagenoses or autoimmune diseases. Mostly women are affected.
Read more on the topic: Circulatory disorders of the hands
Heart symptoms
If there are circulatory disorders in the heart, one speaks of coronary artery disease (CHD). In CHD, the coronary arteries are affected by the circulatory disorders, so that parts of the heart muscle are no longer adequately supplied with oxygen and nutrients and the heart can no longer work properly. Typical symptoms are pain and tightness in the chest, which is often accompanied by a feeling of anxiety. Sometimes there is also nausea. These symptoms are referred to as angina pectoris, or in extreme cases, if the coronary arteries close completely, they are compatible with a heart attack. Chest pain is burning or cutting in nature, and the tightness in the chest is often described as having a heavy weight or an elephant on the chest. The pain usually radiates from the chest to the left arm, but can also radiate to the neck, jaw and back area. This is usually accompanied by shortness of breath. If there is no acute occlusion, these symptoms occur in the context of an angina pectoris attack only under heavy stress. Provoking stress can be vigorous physical activity, high stress potential and cold.
In contrast to a heart attack, the symptoms of an angina pectoris attack disappear again relatively quickly when the exercise is stopped. As a rule, the symptoms stop after a maximum of ten minutes. Like PAD, angina pectoris can be divided into different classes based on the symptoms. In class 1, the symptoms only appear after long and heavy exertion. In class 2, the complaints already occur with everyday stress such as climbing stairs, walking uphill or in cold weather and psychological stress. Class 3 is angina pectoris that occurs even with light physical exertion, such as normal walking. Class 4 is reached when the symptoms appear while resting.
Symptoms around the eyes
Without an adequate blood supply, the retina can no longer fulfill its function. There are severe visual impairments up to blindness. Circulatory disorders of the retina can be chronic or acute. If there is a chronic disturbance of the blood circulation, the eyesight gradually deteriorates. This can be triggered by various diseases, such as what is known as diabetic retinopathy, in which an underlying sugar disorder damages the blood vessels that supply the retina. High blood pressure can also lead to mostly temporary blindness. If there is an acute circulatory disorder, the affected eye suddenly goes blind without warning signs. The whole eye does not always have to go blind, it can also lead to severe visual impairment or to failure of parts of the visual field, so that areas are only perceived as black spots. All processes are painless. If the blood-carrying veins of the retina are blocked (retinal vein occlusion), this results in a painless deterioration in visual acuity. Blurred vision occurs. Often this is described as a veil in front of your eyes. The problem with a venous circulatory disorder is that the symptoms appear relatively late. The symptoms often occur at night, as the blood pressure drops at night and at the same time the pressure in the eye veins increases due to the lying position. In the morning, those affected notice a deterioration in vision, which can improve again over the course of the day. A blockage of the carotid artery can also lead to insufficient blood supply to the retinal vessels. However, there are also accompanying symptoms, similar to a stroke.
Please also read our article on this Clogged carotid artery (carotid stenosis)
Symptom of cold hands and feet
The blood has a variety of tasks in the body: It not only distributes oxygen and nutrients throughout the body, but is also an important regulator in the heat balance. As the blood is warmed up in the trunk of the body during its circulation through the body's vascular system, it helps to transport the temperature to the arms and legs and thus to maintain it in the extremities. In the case of circulatory disorders, this mechanism is now disrupted:
Not enough warm blood comes from the torso through the arteries to the extremities, which cools them down. Hands and feet - or fingers and toes - are particularly at risk, as there is a relatively long way ahead of them that the blood has to cover and on which further heat is already lost. Cold hands and cold feet can therefore occur even with minor circulatory disorders. Particular caution is required if there is evidence that the circulatory disorder affects a larger area, such as an entire lower leg. Such a more serious circulatory disorder should be clarified as soon as possible and as an emergency.
diagnosis
A first suspected diagnosis of circulatory disorders can usually be made based on the typical symptoms. However, there are a number of examination methods that can confirm this suspicion and determine the exact severity of the disease.
The comparative blood pressure measurement of the two halves of the body is very banal, but also very meaningful. For example, if the blood pressure on the right arm is significantly lower than on the left, this is a very strong indication of a vascular change in the right extremity. You can also determine the blood pressure values on both upper arms and both ankles and then compare them with one another. If the ratio of the measured pressures is below a certain value, this also indicates a circulatory disorder.
In addition, so-called angiography can be helpful. During this examination, the patient is injected with an X-ray contrast agent into an artery (attention: a contrast agent allergy must be excluded beforehand!). The vascular interiors filled with contrast agent stand out clearly from their surroundings on the X-ray image. With the help of this method, the location of an obstruction can be determined quite precisely.
There are also the so-called provocation tests, which are mainly used in the diagnosis of PAD. For example, the doctor may ask the person concerned to walk a certain distance and then find out the severity of the disease based on the steps taken without pain.
Where can circulatory disorders occur?
Circulatory disorders in the leg
A circulatory disorder in the leg often results from an existing arteriosclerosis or a thrombosis in the leg.
One then speaks of a peripheral arterial occlusive disease (short: PAOD).
Depending on the level at which the closure of the vessel is located, a distinction is made between a thigh type, pelvic type or peripheral type. The most common type of femur is the femoral type, in which the femoral artery is severely calcified and eventually becomes narrowed enough to cause symptoms. The leg is pale and feels cold. Patients often suffer from leg pain, which increases with exercise but also occurs at rest. One speaks here of intermittent claudication. The patients can walk a short distance, but then have to take a break due to the pain until the pain improves and they can continue walking.
On the affected leg, there is often only a weak pulse or no pulse can be felt. Wounds on the leg heal much worse because of the reduced blood flow.
In the final stages of the disease, tissue can even die (necrosis). The lack of oxygen leads to massive destruction of the cells.
Read more on the topic: Circulatory disorder in the legs
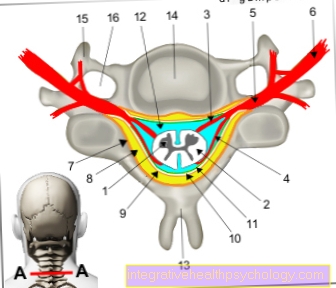
Circulatory disorders in the brain
Circulatory disorders in the brain can be due to poor vascular status or a suddenly blocked vessel due to a thrombus.
If there is arteriosclerosis, calcifications can also be found in the vessels of the brain. But the blood supply can also suddenly be disrupted by a detached thrombus from another region of the body.
The reduced supply of brain areas with oxygen can develop into a life-threatening situation. The circulatory disorder can lead to a stroke, which manifests itself as a sudden paralysis, usually on one half of the body.
The patients lose the feeling in the affected extremities and can no longer move them properly. Often there are also signs of paralysis on the face, such as a drooping corner of the mouth. Those affected can no longer communicate properly in the acute situation. They can also lose consciousness.
The stroke is an emergency and requires immediate treatment, otherwise the consequences can be severe and the symptoms may no longer subside. In the case of circulatory disorders, the vascular status of the brain should therefore always be taken into account so that a stroke does not occur.
Read more on the topic: Circulatory disorders in the brain
Circulatory disorders in the eye
Serious circulatory disorders in the eye usually result in partial loss of vision. Caution and urgency are therefore required here: If a sudden deterioration in vision or a point-like failure is noticed that begins over a few hours, an ophthalmologist or an eye clinic should be consulted as soon as possible. Treated quickly, eyesight can then be restored. A circulatory disorder in the eye is usually localized in the retina because the vitreous humor of the eye is not supplied with blood vessels. However, since the visual signals are recorded and processed on the retina, a circulatory disturbance that occurs here endangers the eyesight acutely.
Circulatory disorders in the eye occur particularly in the context of a fundamental disease such as diabetes mellitus or high blood pressure.
In diabetes mellitus, retinal vascular occlusions are referred to as retinopathy. However, a blood clot that has washed ashore can also block the arterial or venous vessels.
A closure means that the eye is poorly supplied with oxygen and important nutrients. This is followed by a gradual but increasing deterioration in vision.
Patients often report a gray haze in the field of vision. The occlusion of a venous vessel can go unnoticed for a long time, while the arterial occlusion is often associated with sudden painless loss of vision. In the case of a papillary infarction, the optic nerve is damaged as a result of a disturbance in blood flow.
Here, too, there are failures in the visual field. The circulatory disorders in the eye should be treated immediately. The ophthalmologist can use an ocular fundus to assess the vessels and nerves and initiate the appropriate therapy to avoid permanent vision loss.
Read more on the topic: Circulatory disorders in the eye
Circulatory disorders in the ear
Sudden hearing loss, also known as sudden hearing loss in medical terminology, can have various causes.
In addition to stress, constant noise pollution and infections, the blood vessels can also be damaged.
As a result, the structures of the ear that are important for hearing are supplied with insufficient oxygen and nutrients that are important for the cells. The sudden hearing loss can manifest itself in different ways.
Affected persons can perceive the noises as if through cotton wool, hear additional noises like a hissing noise. A feeling of pressure in the affected ear can also be part of the symptoms. Last but not least, the reduced blood flow results in lower blood pressure in the vessels of the ear. This can also be a possible cause of the suddenly onset of unpleasant tinnitus.
The patients then often hear a loud whistling tone on one side, which is permanent. Causes of a circulatory disorder in the ear are coagulation disorders, embolisms or clots that have washed up, or also calcified vessels caused by arteriosclerosis that spreads over the entire organism.
Stress is also one of the risk factors for sudden sudden hearing loss or tinnitus. Both diseases have a high spontaneous healing rate, but the disease should be clarified if symptoms appear for the first time. A thrombus carried into the ear can also trigger a stroke.
Read more on the topic: Circulatory disorders in the ear
Circulatory disorders in the heart
Circulatory disorders in the heart occur in the context of a coronary heart disease, briefly CHD on. These are constrictions or closures of the heart vessels that supply the heart and especially the thick muscle layer with blood and nutrients.
Find out more about the topic: coronary artery disease
The vessels are often heavily calcified due to arteriosclerosis and plaques are found in several places. These can increase in size to such an extent that they ultimately lead to a complete closure of a vessel. The characteristic symptoms of a heart attack occur.
These include sudden chest pain that can radiate into the arm and back, shortness of breath, nausea and also cardiac arrhythmias.
These symptoms are alarming and a life threatening situation that should be treated immediately. Patients with a known CAD can often experience seizure-like chest pain (Angina attack) suffer, which then go hand in hand without an acute heart attack, but which represent a serious warning.
Read more on the topic: Circulatory disorders in the heart
Circulatory problems in the fingers or toes
The fingers and toes are pervaded by many small and fine blood vessels. Because of the small size of these vessels, it can more easily lead to circulatory disorders. Even in the cold, the vessels often contract so much that the fingers or toes appear bluish. This is already a form of circulatory disorder, but of course it is reversed as soon as it gets warmer.
However, if symptoms such as numbness or tingling are perceived regularly and independently of external influences, this can indicate a more complex disorder of the blood or circulation. Therefore, in such cases, a doctor should be consulted to clarify the exact cause.
Read more on the topic: Circulatory disorders in the finger
Circulatory disorders caused by smoking
Smoking or nicotine consumption is the most serious and most common cause of circulatory disorders of all kinds. On the one hand, smoking constricts the blood vessels, so that blood flow to finer vessels such as in the hands, feet and face is poorer. On the other hand, smoking changes the composition of the blood to the extent that the proportion of solid blood components is increased in relation to the liquid proportion (plasma): Firstly, tobacco smoke makes a small part of the red blood cells unusable due to the carbon monoxide content.
So new red blood cells have to be reproduced without breaking down those that are not functioning.Second, the biochemical stress that nicotine causes in the body also increases the relative number of platelets in the body. This ultimately increases the risk of circulatory disorders such as thrombosis.
Read more on the subject at: Circulatory disorders caused by smoking
Circulatory disorders in the knee
If a part of the body is not properly supplied with blood for a long time, the body cells in this area can die. In medical terms, one then speaks of necrosis. If this necrosis has arisen without the influence of an infection, for example due to a circulatory disorder, it is also called aseptic necrosis. Circulatory disorders in the knee can result in necrosis, for example of the bony components.
In medical terms, this is called Ahlbäck's disease. In contrast to a “simple” circulatory disorder, the early symptoms are severe pain in the knee. In any case, appropriate therapy should be provided that supplies the part threatened by the necrosis with oxygen and eliminates or excludes the circulatory disorder as a possible underlying cause.
Find out more about the topic: Ahlbäck's disease
Circulatory problems in the hip
The hips are generally well supplied with blood vessels, so that in the event of circulatory disorders, “substitute routes” usually develop. Due to the proximity to the body trunk, many of the blood vessels located here are also relatively large; in the event of a circulatory disorder, such vessels are usually only affected later. In the case of an advanced chronic (i.e. permanent) circulatory disorder, an insufficient supply of certain areas can occur if the so-called capillaries (thinnest blood vessels that border the cells to be supplied) are affected.
As described above for the knee joint, such a shortage of supply can affect the bone of the hip joint. The bone cells can then die. One then speaks of aseptic femoral head necrosis, since the death is caused by the circulatory disorder and not by an infection. For treatment, a change in lifestyle should first be made: Smoking, sedentary lifestyle and a high-fat diet should be eliminated as risk factors. In addition, drugs can be used that reduce blood lipid levels in the long term. In more advanced stages, vascular surgery can also restore blood flow to the area.
For more information, see: Femoral head necrosis
Circulatory disorder in the ankle
Similar to the knee and hip joint, the ankle joint can also be affected and damaged by a circulatory disorder in the leg. This can lead to what is known as osteonecrosis, i.e. the death of the bone cells in the joint, which are dependent on oxygen supply from the blood. One then speaks of osteonecrosis dissecans.
Such a condition can be serious as it is often associated with severe pain at rest and movement, as well as difficulty walking. However, it is a rare disorder because the ankle - like most parts and regions of the body - can be supplied with blood through several vessels. So the circulatory disorder in the legs must already be at an advanced stage so that the ankle bones are undersupplied with oxygen for a long time.
Find out more about: Osteochondrosis dissecans ankle
Treatment options for a circulatory disorder
Circulatory disorders can have a variety of causes and must therefore be treated differently. The most common cause of a circulatory disorder is a narrowing of the arterial blood vessels. To remedy this, a lifestyle change should definitely be made to avoid risk factors. Smoking should be given up and blood lipid levels should be kept low. This can be ensured through a low-fat and balanced diet and sufficient exercise. If that is not enough, blood lipid lowering drugs can be prescribed, which must then be taken regularly - even if the blood lipid levels have reached the normal range.
Read more on the topic: Therapy of circulatory disorders
Any existing diabetes mellitus (“diabetes”) should also be treated correctly, since the body's sugar and fat balance interact closely and diabetes mellitus is therefore also a risk factor for the development of vascular diseases and circulatory disorders.
If the circulatory disorder persists and there is a threat of permanent damage to an area, operations can be performed to restore the blood supply to the area in question. On the one hand, this includes stents, i.e. fine wire frames that are placed into the vessel from the inside and push the vessel wall apart at the narrowed point. Furthermore, a bypass can be set, i.e. a vessel from your own body that functions as an artificially created bypass route for the blood flow. The lifestyle should also be adjusted accordingly during the follow-up of such interventions, not least to avoid future circulatory disorders.
Medication
In order to treat a chronic, i.e. permanent, circulatory disorder with medication, medication usually has to be taken over a long period of time. Usually two classes of active substances are prescribed: First, the so-called aggregation inhibitors (“blood thinners”) such as ASA. These substances prevent the platelets from sticking together and thus prevent blood clots from occurring. Such blood clots can block smaller blood vessels and cause acute circulatory disorders such as a heart attack, an embolism or a thrombosis.
Another class of active ingredients that are often used for chronic circulatory disorders are blood lipid lowering drugs (“statins”). These lower the cholesterol level in the long term, which protects the vessel walls from further deterioration in blood flow. Because a circulatory disorder is usually based on arteriosclerosis, which in turn is very often caused by chronically high cholesterol in the blood. Drug treatment should only be given if a change in lifestyle cannot be carried out or is insufficient to reduce the risk.
Read more on the topic: Medicines for circulatory disorders
surgery
More serious circulatory disorders that threaten the oxygen supply to a specific part or area of the body can also be treated surgically. Depending on how acute the circulatory disorder is and how large the area at risk is, different vascular surgery interventions come into question. A sudden blockage of a blood vessel usually has to be cleared either with medication or with a stent so that the affected area is not damaged in the long term.
Read more on the topic: Stent
A stent is a small, tubular mesh of wire that is inserted into the vessel and deployed around the narrowed or blocked area. As a result, it keeps the vessel wall open at this point, so that blood flow is guaranteed at this point. The access route is usually via a vessel in the groin. Here a fine, special plastic wire is inserted into the vascular system and pushed forward to the appropriate point.
Another method of treating a circulatory disorder surgically is bypass. For this purpose, a piece of vein is removed - usually from the lower leg - which is not absolutely necessary for the blood supply, and used as a bypass route for the point where the blood circulation is disturbed. During the operation, surgery is carried out in two places: at the point where the vein was taken and at the place where it was used.
Find out more about the topic: bypass
These home remedies can help
In principle, any home remedy that increases the blood flow helps against a circulatory disorder. This can be, for example, warmth in the form of a footbath, which expands the vessels in the feet and thus contributes to better blood circulation in the legs and feet. Pulse warmers can ensure blood flow to the hands and fingers by holding the blood vessels in this area wide.
Another strategy is to use substances that are naturally sharp or may burn. Brandy vinegar, horseradish, or chilli can make a good basis for poultices or pastes that, when applied to the skin, help ensure blood flow to the part of the body. In addition, Gingko contributes to vasodilatation, especially of the smaller vessels, and thus to better blood circulation. Gingko extract is available in compressed tablets or capsules and can be taken daily. The most important thing, however, is still - if not already done - a change in lifestyle in the sense of more exercise, a balanced diet and, above all, not smoking.
Which doctor treats circulatory disorders?
A circulatory disorder can be treated by different doctors due to its diverse causes. A specialist in angiology has specialized in vascular diseases and can therefore be consulted. Even a cardiologist only deals with the heart, but also with the circulatory system and can treat a circulatory disorder.
Doctors in vascular surgery can also offer treatment concepts for a circulatory disorder. Surgery does not necessarily have to be in the foreground as a treatment method: The vascular surgeon should generally be able to provide information about all treatment options for vascular diseases. In addition, there are of course also highly acute circulatory disorders such as a stroke, a heart attack, a pulmonary embolism or a thrombosis, which accordingly require emergency medical care.
Read more on the subject at: Which doctor treats a circulatory disorder?
prophylaxis
In order to avoid circulatory disorders, you should eat a healthy and balanced diet and make sure you get enough exercise. In combination, these two measures also represent the most important points of attack to reduce any existing excess weight. In addition, one should stop smoking or, ideally, not even start and treat or have any underlying diseases associated with a circulatory disorder (such as diabetes mellitus, lipid metabolism disorders or high blood pressure) treated or treated.
How can you prevent circulatory disorders?
Circulatory disorders can occur due to various causes and risk factors.
First of all, they can be avoided by reducing the risk factors.
- Do not smoke (please refer: Circulatory disorders caused by smoking)
- healthy eating
- a normal weight
- regular exercise and
- adequate alcohol consumption
can have a positive effect on the vascular status in the entire organism.
The vessels can also be examined as part of an examination using sonography. During the examination, the carotid arteries are often scanned, which can then provide information about the vessels in the entire organism.
If there is arteriosclerosis, it can initially be treated conservatively by switching off noxious substances such as smoking. Depending on the severity, patients may need to take blood-thinning medication for life. They ensure the blood supply to all important structures, such as those in the heart, despite the presence of constrictions in the supplying vessels.
Read more on the topic: Medicines for circulatory disorders
This can prevent strokes or a heart attack. If symptoms such as numbness, tingling or general pain appear in the course of the disease, the constrictions can be removed during a minimally invasive procedure.
Plaques or arteriosclerotic vessels can be expanded again by means of a balloon or an insert of a stent. The application of nets over the plaques is intended to prevent them from peeling off and ultimately avoid a heart attack or stroke due to a flooded thrombus.
forecast
The prognosis of circulatory disorders is very variable depending on the extent and location. It all comes down to whether or not there is a way to completely cure the underlying disease. For example, vascular damage caused by arteriosclerosis can never be regressed; one can only try to prevent further progression.
However, if the disease is not stopped, it can lead to the life-threatening complications of a heart attack or stroke. If the circulatory disorder in one limb (arms or legs) is at a very advanced stage, amputation may sometimes be necessary. However, this can usually be avoided by taking appropriate preventive measures.
Summary
Circulatory disorders can be acute or chronic. It can arise suddenly or from another underlying disease (diabetes, hypercholesterolemia). A circulatory disorder can appear anywhere in the body and become symptomatic. Although these different factors result in a very heterogeneous clinical picture, many similarities can be identified.
The result of circulatory disorders is always the reduced supply of oxygen to the organ supplied by the constricted / closed vessel, regardless of whether this is the heart, the brain or the muscles. This inadequate supply becomes noticeable through a functional impairment and usually also through pain. Depending on the area affected, of course, a specific treatment follows.
However, the reduction of risk factors has a positive effect on all types of circulatory disorders, including smoking, lack of exercise, high blood pressure, an unhealthy diet resulting in obesity or the widespread disease diabetes mellitus. So if you generally do something actively for your body and your health, you can never completely rule out the possibility of a circulatory disorder, but you can significantly reduce the risk.