Inflammation in the shoulder - causes, symptoms & treatment
definition
The shoulder is one of the most flexible joints in our body and is particularly stressed by tennis players but also in various professions such as craftsmen.
Inflammation in the shoulder can have many causes, but it is always associated with pain and decreased mobility. Therefore, an inflammation in the shoulder should always be treated by a qualified doctor.

Causes of shoulder inflammation
Inflammation in the shoulder occurs primarily in older patients, but it can also occur in younger patients due to severe stress.
There is a bursa in the shoulder area to enable the arm to move freely. This enables the muscles to slide together smoothly with every movement, but especially when we stretch the arm upwards. This movement is known as elevation. Only through the bursa in the upper area of the shoulder under the palpable protrusion of bone, the acromion (Subacrominal bursa), we can do this movement without pain.
If the bursitis now becomes inflamed, the patient feels severe pain from this type of shoulder inflammation. Bursitis is usually caused by overloading the arm and raising the arm too often. This can lead to small tears in the bursa, which then ensure that bacteria reach the bursa and cause painful inflammation there.
However, one usually speaks of a shoulder inflammation when the shoulder joint itself is inflamed. In medical jargon, shoulder inflammation is also known as shoulder arthritis or omarthritis. The shoulder inflammation can be bacterial, i.e. infectious, or it can develop non-infectious due to a rheumatic disease.
The cause of rheumatic shoulder inflammation is often based on a so-called autoimmune disease. This means that the body, like after an infection with rubella or another disease, forms antibodies which then fight the infection and, in the best case, contain it.
Read more on the topic:
- What is an autoimmune disease?
- Tendinitis in the shoulder
- Inflammation of the shoulder blade
Inflammation of the shoulder from rheumatism
In the case of rheumatoid arthritis, which can lead to shoulder inflammation, antibodies are directed against the synovial membrane and damage it. In addition to the shoulder, other joints are usually affected, such as the finger joints or the knee.
In addition to pain, patients also complain of swelling of the joints and restricted mobility.
Inflammation of the shoulder due to tendinitis
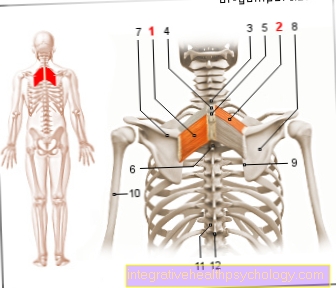
Since the shoulder consists not only of the actual shoulder joint but also of ligaments and muscles, tendinitis can occur in the area of the muscles, especially in the case of the supraspinatus muscle, whose tendon pulls over the shoulder joint and is constricted by the protruding bone, the acrominon . The supraspinatus muscle arises from the upper part of the shoulder blade (Scapula) and pulls from here over the shoulder to the humerus (Humerus).
When the muscle contracts, we can stretch the arm up sideways, as if we wanted to fly with our arms. An inflammation in the shoulder occurs when the insertion tendon of the supraspinatus muscle is inflamed; it is called tendinitis.
Excessive exercise in particular often leads to inflammation, for example if the patient very often sleeps with his arms raised. In addition to the supraspinatus tendon, the tendon of the biceps muscle (the prominent biceps on the upper arm) can become inflamed. The causes of this inflammation in the shoulder are the same as with the supraspinatus tendon - including overload in the shoulder movement area.
Read our articles on this
- Tendinitis in the shoulder
- Tendinitis in the upper arm
Bursitis on the shoulder
Bursitis of the shoulder is usually the bursa under the roof of the shoulder (acromion), the so-called subacromial bursa. This ensures that the thigh bone does not touch the roof of the shoulder when the arm is raised and that it causes pain with every movement.
However, if the bursa is inflamed, it can cause sharp pain. The inflammation usually arises from stress such as overhead movements of the arms. The pain can initially be felt when lifting the arms over the shoulder level. If the shoulder is not spared in the further course, the pain can become stronger and occur even at rest. The shoulder can also become tender and cause pain at night.
Swelling and reddening of the shoulder joint are rare. The shoulder should always be examined by a doctor; imaging examinations such as ultrasound, X-ray or MRI may be necessary.
Bursitis is usually treated with cold compresses, anti-inflammatory pain medication such as ibuprofen or sports ointments. In addition, physiotherapy can accelerate healing. If, despite these therapies, there is no healing and persistent pain that restricts everyday life, an operation may be necessary.
Find out more at: Bursitis of the shoulder
Appointment with a shoulder specialist

I would be happy to advise you!
Who am I?
My name is Carmen Heinz. I am a specialist in orthopedics and trauma surgery in the specialist team of .
The shoulder joint is one of the most complicated joints in the human body.
The treatment of the shoulder (rotator cuff, impingement syndrome, calcified shoulder (tendinosis calcarea, biceps tendon, etc.) therefore requires a lot of experience.
I treat a wide variety of shoulder diseases in a conservative way.
The aim of any therapy is treatment with full recovery without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
You can find more information about myself at Carmen Heinz.
Symptoms of an inflamed shoulder

An inflammation in the shoulder causes the patient primarily severe pain. Especially when he moves his shoulder and puts weight on it.If the bursa becomes inflamed, elevation, i.e. the arm movement away from the body, is particularly difficult because it is associated with severe pain. In addition, there may be a slight swelling in the area of the shoulder joint.
If the inflammation of the bursa in the shoulder is bacterial, so-called B symptoms may also occur, which are typical of bacterial inflammation. These include night sweats, fever, body aches and general malaise with accompanying fatigue.
In the case of classic shoulder inflammation, however, the patient usually has inflammation in other joints in addition to the inflammation in the shoulder. Most of the time, the pain gets better after some time of movement, as the joints are then warmed up.
With this type of inflammation in the shoulder, it is typical that symptoms appear equally with each type of movement. So it makes no difference whether the arm is lifted to the side, forwards or backwards. Every time there is weight on the shoulder it creates pain.
The patient should also mention when the symptoms appear. If the patient complains of pain in the shoulder area due to inflammation, this indicates rheumatic omarthritis. In addition to the pain due to the inflammation in the shoulder, there can often also be a loss of function, in which the patient can practically no longer use the shoulder and, accordingly, can only use the arm to a very limited extent.
With tendinitis, the patient often complains of general pain in the shoulder area, but the pain is worst when the patient tries to lift the arm in the extended position only to the side (i.e. neither forwards nor backwards). Typically, the patient can raise the arm up to a 90 degree angle, anything above that causes him severe pain due to the inflammation of the tendon that he cannot bring the arm up any further.
You might also be interested in: Shoulder Neck Pain - What You Should Know About It
In order to be able to distinguish an inflammation in the shoulder from a capsule tear in the shoulder area, it is recommended to deal with the following topic: Capsule tear in the shoulder
Treatment of inflammation in the shoulder
Therapy for inflammation in the shoulder depends on the cause of the disease.
In the case of bursitis, i.e. an inflammation of the bursa in the shoulder, the primary focus is on immobilizing the joint, since the inflammation in the shoulder in this case is caused by overloading the shoulder. In addition, the patient should take non-steroidal anti-rheumatic drugs (NSAIDs for short) to counteract the inflammation in the shoulder and thus also the pain.
In addition, the patient can treat the inflammation in the shoulder with heat or cold therapies (for example with cold compresses or with heat pillows, as required), depending on how they feel. The patient can simply pay attention to this. whether the cold helps him against the pain or whether warmth provides relief.
If the inflammation in the shoulder bursa does not heal, the doctor can also inject glucocorticoids directly into the patient's shoulder.
In the worst case, if the symptoms persist, the bursa must also be removed (Bursectomy) be considered. However, this should be the last form of therapy, as removing the bursa from the shoulder also reduces a certain mobility.
If the bursitis is bacterial, it is also important to keep the shoulder still. This alone is not enough, however, and the patient must also take antibiotics to eliminate the bacteria that are responsible for the inflammation in the shoulder. In addition, the inflamed secretion can be released from the bursa.
In the case of classic shoulder inflammation (omarthritis), basically the same therapy is carried out as for rheumatoid arthritis. However, since the shoulder is usually only restricted in the late stage, only an operation in which the shoulder joint is (partially) replaced and renewed often helps.
Nevertheless, the patient should try to minimize the inflammation in the shoulder and the associated pain as much as possible by means of physiotherapy before undergoing an operation. Therapy for omarthritis is usually very tedious and not always promising.
In the case of tendinitis of the muscles of the shoulder, it is important to protect the affected muscles and to rest the shoulder as much as possible. Usually the tendinitis should go away on its own after a while. In addition, you can apply an anti-inflammatory cream to the shoulder to help the affected muscles heal.
The cold also helps most patients to relieve the pain and at the same time to contain the swelling that often occurs with tendonitis. In more difficult cases, the doctor can prescribe a cream containing cortisone or inject the cortisone directly into the affected shoulder area.
Surgery is only necessary in rare cases.
Home remedies for the sore shoulder
Cold compresses and curd compresses should be used for acute inflammation. Cold compresses can be wrapped in a cloth in the form of cooling packs or ice cubes on the affected shoulder. The cooling should not take longer than 15 to 20 minutes. A break until the next cooling should be observed for at least two hours.
Ginger tea can also be used against inflammation and shoulder pain. The tea can be drunk two to three times a day. Freshly grated, cooked ginger can also be wrapped in a cotton towel and placed on the affected shoulder.
Castor oil is also anti-inflammatory. As a remedy for the inflammation in the shoulder, a cloth can be soaked in castor oil and placed on the shoulder joint for 30 to 40 minutes.
Dried willow bark tea can also help reduce inflammation. Since willow bark has a blood-thinning effect, it should not be combined with blood-thinning medication.
Homeopathy for an inflamed shoulder
Homeopathic remedies can be used to support home remedies, drug therapy or physiotherapy. Taking homeopathic globules can help alleviate the symptoms of shoulder inflammation.
In general, if you have shoulder pain, you can take 5 globules of Bryonia (bryony), Rhus toxicodendron (poison oak) or Ruta (rue) three times a day. Arnica globules can also have a positive effect on inflammation in the shoulder.
Schüssler salts for an inflamed shoulder
Schüssler salts contain mineral salts in homeopathic doses. They can also be used to help heal inflammation of the shoulder.
The Schüssler salts No. 3 Ferrum phosphoricum D12 and No. 4 Kalium chloratum D6 are recommended as tablets or ointments in the case of inflammation of the joint. For movement-dependent pain in the shoulder, in addition to Schüssler Salt No. 3, No. 5 Kalium phosphoricum D6 can also be used.
It should be used three to six times a day with one to three tablets each time.
Does warmth or cold help with an inflammation of the shoulder?
Heat should not be used in acute inflammation. A heat treatment causes the blood vessels to dilate, which increases blood flow and allows immune cells to migrate into the tissue. This can lead to faster joint destruction and permanent discomfort. It is therefore important to cool the shoulder in the event of acute inflammation. This causes the vessels to constrict, the pain is relieved by the cooling and swelling can decrease.
A cold application can be carried out using cooling packs or quark wraps. Cooling should therefore take place in the case of bacterial or acute attacks of rheumatoid arthritis, tendinitis, bursitis or activated osteoarthritis.
Heat treatment helps if the pain has caused muscle tension by relieving the shoulder. The tension can be loosened with warmth. Chronic pain caused by rheumatism can be treated with moist heat, for example with a cloth dipped in moist, warm water.
Duration of an inflamed shoulder
The duration of the inflammation depends on various factors. It is important to carry out therapy early and to take care of the shoulder. If therapy is carried out in good time, long-term damage can be avoided.
- Bursitis should be healed after a few weeks with adequate therapy and protection.
- Bacterial inflammation should heal after four to six weeks of antibiotic therapy.
- Because rheumatoid arthritis is an autoimmune disease, the inflammation will come back in flares and cannot be cured by medication. Nevertheless, adequate therapy is necessary to delay joint wear and tear.
Ultimately, any joint inflammation can cause damage to the joint and cartilage and thus lead to permanent pain. These can then only be alleviated through medication, physiotherapy and gymnastics. The destruction of the joints can also lead to osteoarthritis in the shoulder, which can repeatedly cause discomfort.
Prophylaxis: How do you prevent an inflamed shoulder?
In order to counteract inflammation in the shoulder, it helps above all not to permanently overload the shoulder and to ensure good posture and sufficient exercise. Anyone who frequently suffers from inflammation in the shoulder should consider physiotherapy, where the physiotherapist can provide information about any improper posture that may have been trained.
Diagnosis of inflammation in the shoulder
An inflammation in the shoulder is often based on the anamnese, the doctor-patient conversation. If the patient complains of increasing pain in the shoulder and restricted mobility, the situation is often clear. In addition, the Scan (Palpation) the pain can be localized more precisely and Signs of inflammation (Overheating of the shoulder joint) can be determined. In addition, a blood sample should always be taken so that you can see whether the inflammation in the shoulder is a bacterial inflammation or rather an overload of the shoulder. The doctor often takes additional samples Synovial fluid to detect inflammatory cells here as well. In rare cases, the shoulder becomes additional x-rayed or it becomes one Magnetic Resonance Tomatography (MRI of the shoulder) performed.
Forecast of inflammation in the shoulder
In general, inflammation in the shoulder has a good prognosis. Especially with bursitis and tendinitis, the patient can usually be helped very easily and very easily. The situation is different with omarthritis. This can lead to protracted therapies and the patient often has to live with a certain residual pain or with a certain restriction in the shoulder area. It is all the more important that the patient undergoes long physiotherapy in order to achieve the best possible results.
Special form of inflammation (humeroscapular periarthritis)
- definition
The inflammation of the shoulder joint is usually referred to as the frozen shoulder.
This comes from English and means: frozen = frozen, stiff and shoulder = shoulder.
There are a variety of causes for this very painful condition, which affects the soft tissues, muscles, and tendons near the joint. Usually it is degenerative diseases in the shoulder joint that lead to the pain and stiff shoulder.
The technical term for shoulder joint inflammation is Humeroscapular periarthritis. The first part of the name is made up of the Greek words peri (around), Arthrosis (joint) and -itis (inflammation) together. The second part of the word means that there is inflammation between the humerus (humerus) and the shoulder blade (Scapula) acts.
- Symptoms
Inflammation of the shoulder joint causes shoulder pain and restricted mobility. Most people only have one joint affected, but every third person has both shoulders inflamed.
Both active and passive movement are severely restricted. If no previous damage or an accident can be determined, one speaks of the so-called primary frozen shoulder. (engl. and means stiff / “frozen” shoulder).
In the primary form, there are three different phases of the disease. There are characteristic symptoms at each stage:- Phase 1: The pain mainly occurs at night. Affected people wake up when they turn from side to side. Pressure on the diseased shoulder joint also causes pain. The joint then stiffens more and more - also due to the fact that the sick almost no longer move their arm in order to keep the pain as low as possible.
- 2nd phase: Here the pain becomes less and rather fades into the background. In return, the mobility of the joint is steadily reduced. Due to the lack of movement, the shoulder muscles also degenerate. In order to prevent the pain, most patients adopt a bad posture, which then causes further pain, for example in the neck.
- 3rd phase: Here the frozen shoulder slowly recedes. Often the inflammation does not heal completely and there are often considerable restrictions on movement.
- root cause
Inflammation of the shoulder joint usually comes from a degenerative change in the shoulder girdle such as bursitis (Bursitis), tendinitis (Tendonitis) or the impingement syndrome (Bottleneck syndrome - For example, thickening of the soft tissues can reduce the space under the roof of the shoulders, resulting in a bottleneck - there is not enough space to provide enough space for all structures running there.)
Torn tendons or calcifications can also lead to inflammation. Immobilizing the joint also quickly leads to a frozen shoulder.
- therapy
First and foremost, the therapy always depends on the cause, the duration and the severity of the pain. In most cases, conservative treatment methods are used. This means that no surgery is necessary.
The effective alternative methods are primarily understood as physiotherapy and treatment with medication, and very rarely radiation therapy or acupuncture. With the alternative treatment methods, an improvement in the symptoms takes a few weeks to months. In physiotherapy, it is important that the exercises do not overload the shoulder joint, especially at the beginning, and do not place incorrect stress on the shoulder joint. The exercises should be well adapted to the pain so as not to worsen the condition of the shoulder.
In addition to manual therapy and physiotherapy, electrotherapy or heat and cold treatments are often used.
The form of treatment depends very much on the stage of frozen shoulder. In the first stage it is important that mobility is maintained and that the pain is alleviated. In the 2nd stage the pain does not become much more severe, but the joint becomes more and more rigid. Here pain relief and relaxation come first. In the last phase there is a decrease in pain and here again the focus is on mobility training. You should always stay on the ball, as the treatment of a shoulder infection is very tedious. In very rare cases an operation is necessary if the cause cannot be combated otherwise or if there is no improvement after approx. 6 months.
- diagnosis
In the case of inflammation, a medical examination is usually successful, in which the doctor takes a comprehensive anamnesis and can thus find out any accidents. Since the shoulder causes pain, the doctor may induce tenderness during the examination. During the ultrasound examination (Sonography) you will find mainly muscle tears and the resulting joint effusions. He can also best control the tendons and ligaments here. Magnetic resonance imaging is mainly used before an upcoming operation. Arthroscopy is rare (Jointoscopy) where the doctor can examine the lead structures and treat the cause a little. In some cases, a previous accident also leads to joint inflammation.
- prophylaxis
It is hardly possible to prevent shoulder joint inflammation, but it is very advisable to see a doctor at the first signs and to start therapy very early.It is also important to take the pressure off the shoulder and largely avoid stressful sporting activities and work with the shoulder.
Recommendations from the editorial team
You might also be interested in:
- shoulder
- Impingement syndrome
- Bursitis shoulder
- Inflammation of the rotator cuff
- Rotator cuff syndrome