Maxillary sinus infection
Anatomy of the maxillary sinus
The maxillary sinus (lat. Maxillary sinus) is counted among the paranasal sinuses and is located within the bony upper jaw (lat. Maxilla).
In humans, it is closely connected to the middle nasal passage, which is why pathogens can easily pass from the nasal cavity into the maxillary sinus, where they multiply and cause infections. The narrower the drainage routes for the secretion, the higher the likelihood of sinus inflammation.

In summary, all inflammation in the sinus area is considered to be Sinus infection (sinusitis) designated.
In the special case of an infection of the maxillary sinus, the resulting disease is called Maxillary sinus infection (Maxillary sinustitis).
Maxillary sinus inflammation is a change in the mucous membrane in the area of the paranasal sinuses caused by the harmful effects of bacteria and viruses. Basically one differentiates between one acute and one chronic Course of this inflammatory disease.
Is Sinus Infection Contagious? Find out more at How contagious is a sinus infection?
Acute maxillary sinus infection
An acute, sudden and one-off inflammation of the maxillary sinus often occurs in the course of a Runny nose or another Cold infection.
Due to the penetration of the pathogens (bacteria or viruses) it can increase within the sinuses Swelling of the mucous membranes, these swellings narrow the natural drainage channels and thus trigger inflammatory processes.
Most of the known cases are specific Viruses for triggering the acute Maxillary sinusitis responsible, bacterial infection is also possible, but much less common.
The maxillary sinus infection is that most common Shape of acute sinus infection, nevertheless, it can be through the above blocked Secretion drainage also leads to inflammation of the Frontal sinus and / or the Ethmoid cells come (see also: Inflammation of the ethmoid cells).
In extremely rare cases, the Sphenoid sinus However, this is a rather rare form of sinus infection.
Acute maxillary sinus infection usually goes with it high fever, Feeling of pressure in the head area, a headache and in general malaise hand in hand.
In most cases, the pathogen's entry point is the Nasal mucosa, the acute forms of sinus infections are caused by a Droplet infection transfer.
Read more on this topic at:
- Sphenoid sinusitis
- Frontal sinusitis
Risk of contagion
Sinusitis can potentially be caused by both Viruses, as well as through bacterial pathogens to be triggered. In general, however, it can be assumed that the majority of affected patients Oral, nose and throat bacteria are causative.
The classic pathogens of the maxillary sinus inflammation are usually via a so-called Droplet infection spread. This means that an inflammation of the maxillary sinus through the air (aerosol or droplet nuclei) or the formation of droplets when speaking can lead to infection.
Many patients mistakenly assume that inflammatory processes in the maxillary sinus are not contagious and therefore do not take any special precautions. This assumption, however, is a fatal mistake. An inflammation of the maxillary sinus can be contagious because their bacterial pathogens are both at Sneeze, as well as with Cough into the air can be released.
In addition, it should be noted that these germs insufficient hand disinfection stick to doorknobs and other surfaces and thus the maxillary sinus infection through Contact infection contagious can be (indirect contact infection).
Chronic maxillary sinusitis
Under the chronic Form of maxillary sinus inflammation is understood to be a disease that lasts longer than two to three months persists. Inflammatory processes in the maxillary sinus, which occur several times within a very short time, are also part of the chronic form of this disease.
In most cases, chronic maxillary sinusitis is the direct result of an acute illness; this can happen if an acute inflammation does not heal or heals insufficiently. Also one Antibiotic resistance can lead to the development of chronic maxillary sinusitis.
In addition to the maxillary sinuses, the Ethmoid cells to be affected.
Other possible causes are Allergies, Curvature of the nasal septum, Nasal polyps or Tooth root inflammation.
The symptoms of a chronic form of this infectious disease include long-lasting loss of smell (Anosmia), stronger, thinner Nasal discharge (Rhinorrhea), Secretion flow in the throat, strong Sensations of pressure in the head area (especially the paranasal sinuses and eye socket) and a headache.
Symptoms
The most commonly reported symptoms of antritis include the occurrence of moderate to severe a headache and a dull throbbing Feeling of pressure in the head area (especially on the Cheeks and under the Eye sockets).
It can be seen that the perceived pain worsens significantly when trying to bend the head towards the chest.
If the maxillary sinus is inflamed, the pain is usually felt most clearly in the area of the cheeks. In addition, some patients complain of severe Toothachewhich is due to the fact that for many people the root the molars of the upper jaw extend into the maxillary sinus.
Usually an inflammation of the maxillary sinus becomes from a severe Runny nose (Rhinitis), in which purulent, yellowish-green secretion flows from the nostrils. This also results in an impairment of normal nasal breathing.
The organism reacts with very strong inflammatory processes high fever and a general feeling of Exhaustion.
In addition, it may become temporary due to the pressure in the eye socket Visual disturbances come.
Also severe swelling of the cheeks and / or the development of a Inflammation of the roots the molars of the upper jaw are possible in the course of an inflammation of the maxillary sinus.
Toothache with an inflammation of the maxillary sinus
Lots of people working at one a flu-like infection With
- to cough
- sniff
- Sore throat and headache
suffer, notice the simultaneous Occurrence of toothache. What is striking in this context is the fact that cold-associated toothache is usually exclusively in the area of the upper jaw arise. The teeth of the Lower jaw are not affected in the majority of cases. The reason for the simultaneous occurrence of maxillary sinusitis and toothache is the close anatomical proximity between the oral cavity and the maxillary sinus.
In addition, both the Maxillary sinus, as well as the Tooth roots of the maxillary teeth mostly supplied by a common nerve branch. Inflammatory processes in the area of the Sinuses (for example in the maxillary sinus) thus practice one painful stimulus which continues via these very nerve fibers to the teeth.
A second explanation for toothache related flu-like infections is the fact that it is common too Accumulations of secretions comes in the sinuses. As a result, the pressure in the sinus area increases significantly and the person affected gets toothache.
Generally it is not necessary to see a dentist when toothache and upper respiratory infections occur at the same time. Help most patients Inhalations with table salt or mint to increase the outflow of secretions and effectively relieve toothache in this way. In pronounced cases you can Painkiller how Paracetamol® or Ibuprofen be taken. However, symptoms should not subside for several days or fever occur, a doctor should be consulted for one if necessary antibiotic therapy to initiate. Otherwise there would be a risk that the acute maxillary sinus inflammation could lead to toothache if the appropriate treatment was neglected chronic form transforms.
Sinusitis without a runny nose
There can be many different reasons for an inflamed maxillary sinus to develop. Because of this, many patients suffer from maxillary sinus infection without it at the same time accompanying symptoms such as runny nose or watery eyes to specify.
In these cases you can bacterial pathogens, for example from the Oral cavity have entered the bony maxillary sinus. A particular risk for the development of a maxillary sinus infection without a runny nose poses the Removal of molars (Molars) of the upper jaw.
In a large number of adults it can be observed that precisely the Posterior teeth of the upper jaw a close connection to Maxillary sinus (Maxillary sinus) exhibit. For some patients, these are enough Tooth roots even right into the maxillary sinus. It comes now because of a necessary Tooth extraction (Tooth extraction) to one Opening of the maxillary sinus, that's how a direct connection to the oral cavity.
Bacterial pathogens can, in Failure to use a suitable closure method, simply migrate into the sinus and provoke an maxillary sinus infection without a runny nose. In everyday clinical practice, however, this happens relatively seldom, since the maxillary sinus can now be opened easily through the Closure of the gums and the targeted intake of a Antibiotic can be treated.
diagnosis

The most important step in diagnosing antritis is taking a detailed doctor-patient discussion (anamnese), in which the person concerned gives the practitioner all symptoms as extensive as possible should portray. Play in this context recent dental treatments (e.g. Tooth extractions or Tooth root treatments) play a crucial role. Should be in the affected patient a short time before symptoms appear If such a dental treatment has taken place, the likelihood of an inflammation of the maxillary sinus is particularly high.
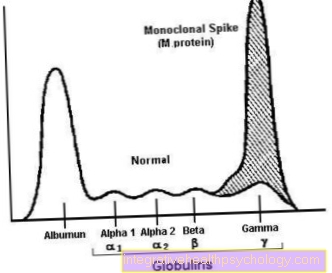
Be during the subsequent physical exam both halves of the jaw pounded. In this way, the diagnosis can usually be made through the Appearance of pain stimuli harden on the affected half of the jaw. As in the course of the inflammatory processes in the area of the sinus specific inflammation mediators are detectable, can also be a Blood test Can be used to diagnose antritis.
In the case of an inflammation of the maxillary sinus increases for example the number of white blood cells and the so-called C-reactive protein (CRP) clearly. If no reliable diagnosis can be made even after these steps, it is advisable to carry out a Nasoscopy (Rhinoscopy). In this examination method, the nasal passage is widened by using a nasal spreader or a flexible tube. An apparatus with a built-in light source and camera (Nasal endoscope) into the inside of the nose.
During this process, the specialist primarily assesses the condition of those lining the nose Mucous membranes. In addition, existing nasal secretions can be assessed and checked purulent residue be checked. However, it is much easier to carry out a Ultrasonic- or X-ray examination. (In everyday clinical practice, making a diagnosis using ultrasound is preferable to making an X-ray, as it is no radiation exposure brings with it.)
In this way, accumulations of secretions and inflammations in the area of the maxillary sinus can be represented visually quite easily.
In the case of chronic forms of sinusitis, despite the relatively high radiation exposure, it is also possible to carry out a Computed Tomography (short: CT) be useful. Inflammation of the maxillary sinus can be seen Thickening of the wall structures and Fluid build-up easy to recognize.
therapy
Basically, the treatment of maxillary sinus inflammation does not differ from that of a common cold.
The affected patients should be in bed for a few days and much liquid, especially water and tea.
In addition, help warm baths and or Hot water bottles over the first few days of illness. Also can saline nasal sprays or Nasal drops help to reduce the swelling. Advantage of saline solutions compared to commercial ones Nasal sprays is the gentler influence on the nasal mucous membranes. However, salt sprays should not be used for more than a week.
Affected patients should try to avoid the sinus area during the illness cool, because in some studies it was found that cooling has a rather hindering and unfavorable influence on the healing process.
Warmth, on the other hand, helps to positively influence the course of the disease and accelerate the healing of the inflammatory processes.
It should also be used to relieve pain if necessary Painkiller be taken.
If the maxillary sinus infection is caused by bacteria, in most cases the attending physician will consult antibiotic prescribe. This should be taken in full, even after the symptoms and complaints have subsided, as directed by the doctor.
In the case of inflammation caused by anatomical reasons (Curvature the nasal septum) or through Polyps surgical treatment may be necessary. Straightening the nasal septum or removing the polyps may be enough to minimize the risk of recurrence. This is because the best possible drainage of the secretion minimizes the likelihood of inflammatory processes developing within the sinuses.
When should an antibiotic be taken?
Antibiotics should only be used under certain conditions in the case of an inflammation of the maxillary sinus. You contribute bacterial inflammation, not with viral inflammation or against fungi. According to this, an antibiotic is not useful for every sinusitis.
Medication and, if necessary, antibiotics should be individually tailored to the cause of the maxillary sinus infection, general condition, age and individual factors. For example, one purulent, bacterial inflammation With fever an antibiotic indicated. Antibiotics can also be useful for bacterial-related complications. Targeted antibiotic therapy can help people with a weakened immune system if they have a bacterial maxillary sinus infection.
Some sufferers initially use herbal remedies, such as Myrtol or Cineole. However, if this does not provide relief or if it gets worse, an alternative and, if necessary, an antibiotic should be considered together with a doctor. In addition, antibiotics are often used after five days of taking decongestants and anti-inflammatory agents such as Diclofenac or Ibuprofen, no improvement or even worsening has occurred.
If the own immune system fails to fight the bacteria, suitable antibiotics can be useful - but only if it is a bacterial inflammation. It is used before any antibiotic therapy Antibiogram recommended. This is a laboratory test that looks at how sensitive or resistant the pathogen is to the antibiotic. Then a suitable antibiotic can be selected in a targeted manner, taking into account the individual risk of side effects.
What to do if the antibiotic does not work
If an antibiotic doesn't help with antritis, you should see your doctor again. It is important, do not stop taking antibiotics on their own or to try something else at random. This could lead to so-called Antibiotic resistance and worsening of the disease. The causes and diagnosis should be thoroughly checked by a doctor. If an allergy is suspected, an allergy history and an allergy test are advisable.
An examination with an endoscope and a laboratory test of the fluid can also provide information, including whether or not it is a bacterial infection. If not yet X-ray or Computed Tomography have taken place, these can be carried out before further measures are considered. These examination methods help to secure the diagnosis and to get an overview of the exact extent. If the diagnosis of bacterial inflammation is confirmed, it may well be that the correct antibiotic has not been selected, as these preparations are responded to individually.
A suitable conversion must be made accordingly. How this is implemented most sensibly should be discussed with the doctor. In the case of inflammation of the maxillary sinus caused by an allergy, antibiotics are usually not helpful, but temporary cortisone. Fluticasone, may be advisable in some cases. When the mushroom Aspergillus caused the sinus infection, antibiotics won't work either. Instead, an anti-fungal agent called an antifungal is recommended
When is an operation necessary and how is it performed?
If the diagnosis is confirmed and the maxillary sinus infection does not heal through conservative measures, including antibiotic therapy, it is possible that a chronic maxillary sinusitis has developed. In this case, surgery is often recommended.
A cyst originating from a tooth also limits the function of the maxillary sinus. A cyst is a cavity filled with fluid. Surgical removal of this cyst is advisable.
Has a previous one Upper jaw surgery leads to an open connection between the oral and maxillary sinuses and subsequent maxillary sinus inflammation, surgical intervention is also recommended. Moreover, must foreign bodythat got into the maxillary sinus and caused inflammatory processes are surgically removed. As a rule, this operation is carried out according to the principle of "Keyhole surgery“With the help of one endoscope, one microscope or one Magnifying glasses. The aim is to keep incisions and scars as minimal as possible.
In some cases, widening the openings in the maxillary sinuses is sufficient to allow fluids and mucus to drain away. The entrance to the maxillary sinus is cleared out. The entire mucous membrane is seldom cleared out, as was done earlier in the classic radical surgery of the maxillary sinus. This is followed by a follow-up treatment, which includes, for example, local removal of secretions and bark in order to prevent tissue growth in the nose.
Certain medications called coticoids are often recommended to prevent re-inflammation of the maxillary sinus. After the operation, check-ups should take place at short intervals over a period of several weeks.
Maxillary sinusitis after a wisdom tooth operation
The isolated maxillary sinusitis mostly arises from tooth root processes. As part of a wisdom tooth operation in the upper jaw, the maxillary sinus mucosa can, under certain circumstances, be injured. This allows bacteria to enter the maxillary sinus and trigger an inflammatory reaction.
In addition, the tooth roots extend to the maxillary sinus so that when a wisdom tooth is removed, the Maxillary sinus opened can be. In this case, this would also be the gateway for bacteria. A connection can arise between the oral and maxillary sinuses. This is called a so-called oroantral fistula.
In order to prevent this and thus an inflammation of the maxillary sinus, this area is treated with a so-called Rehrmann plastic locked by the dentist. After the operation, regular checks will be carried out by the dentist or oral surgeon.
How long does an maxillary sinus infection last?
The duration of an maxillary sinus infection is very individual. The maxillary sinuses are different in every person and, accordingly, their ways of combating inflammation are different. In general, it takes longer for maxillary sinus infections to heal in immunocompromised people than in people with an average or strong immune system.
As a rule, an uncomplicated, acute maxillary sinus infection lasts about 2 weeks. However, the symptoms should subside after a few days after adequate treatment. If the maxillary sinus infection is caused by an allergy, the symptoms should decrease as soon as the allergy-causing substances are avoided. If the maxillary sinus infection lasts longer than 2 weeks or if it returns repeatedly, it may be chronic maxillary sinusitis act. In this case, other methods of treatment are required and the duration is lengthy.
Why is maxillary sinus infection unilateral?
Since the maxillary sinuses are paired, one can differentiate between unilateral and bilateral maxillary sinus infections depending on the cause and entry portal. A so-called odontogenic maxillary sinus inflammationthat occurs in the context of dental problems or tooth extraction in the upper jaw is usually one-sided. Usually the cause is a tooth in the upper jaw on one side. This gives the bacteria one-sided entry into the maxillary sinus on the corresponding side. Bacteria and viruses can also pass unilaterally through the nose into the maxillary sinus, for example as part of a cold.
If the entry point for the pathogen is the nose, unilateral or bilateral maxillary sinus infections can develop. With unilateral maxillary sinus infections in children should also foreign body be thought. Furthermore, a one-sided closure of one of the two rear entrances to the nasal cavity, the so-called choans, could be the trigger for the one-sided complaints. This disorder, known as choanic atresia, can cause unilateral sinus inflammation, among other things.
Furthermore, one-sided chronic maxillary sinus inflammation must always be a tumor disease, a so-called Malignancy be thought. A one-sided maxillary sinus inflammation is noticeable unilateral tenderness in the Cheek area and unilateral head-, and tooth- and sometimes earache.
prophylaxis
One possible measure to prevent sinusitis is this regular flushing the nasal passages with water (for example with the help of a Nasal douche).
Can you fly with an inflammation of the maxillary sinus?
From a medical point of view, there is no reason not to fly for patients suffering from acute maxillary sinusitis. Nevertheless, those affected should note that at normal flight altitudes a much higher pressure load acts on the body.
Since there is already a high pressure in the maxillary sinus in the course of the maxillary sinus infection, it can lead to a Increase in symptoms come. Many patients describe one above all else stronger pain perception while flying. To be able to counteract this phenomenon at least partially, it is recommended before flying Nasal spray apply and at regular intervals Pressure equalization perform. This can be done by moving the TMJ or while flying Breathe against the blocked nose happen.