Hepatic insufficiency
definition
Under one Hepatic insufficiency one understands a restriction of the metabolic functions of the liver. The liver insufficiency thus represents the result or the condition of many diseases or organ damage that can impair the metabolic function of the liver. Seen in this light, it is difficult to strictly separate liver insufficiency from liver failure.

The Liver failure represents the maximum extent and thus the most severe condition of the liver insufficiency. Liver insufficiency occurs very often in the framework chronic liver disease again alcoholic cirrhosis of the liver or more chronic Viral hepatitis but can also be an expression of acute, for example toxic, damage to the liver.
- Liver failure
- Functions of the liver
causes
If the hepatocytes (cells of the liver) are structurally damaged or the blood supply to the liver is impaired, liver failure occurs. The causes can be very different. The most common cause of chronic liver damage in Germany is alcohol abuse. Chronic alcohol consumption leads to alcoholic liver cirrhosis via various intermediate stages. At this stage, the damage to the liver can no longer be reversed (irreversible) and liver insufficiency which is also irreversible results.
In addition to alcohol-toxic liver damage, liver damage from viral hepatitis should also be mentioned. ly the hepatitis viruses B, C and D lead via various transmission routes to chronic or acute viral hepatitis, which can be accompanied by mild to severe liver insufficiency. In the worst case, viral hepatitis also leads to cirrhosis of the liver with irreversible liver failure.
Other causes of liver failure are other inflammatory diseases such as PBC (primarily cheap cirrhosis), PSC (primary sclerosing cirrhosis), Autoimmune hepatitis and parasitic diseases (leishmaniasis, schistosomiasis, malaria). The toxic causes include non-alcoholic fatty liver diseases and various toxins, such as the poison of the death cap mushroom, but also drugs such as methotrexate, amiodarone and paracetamol.
A number of diverse metabolic diseases can also be the cause of liver insufficiency and, if left untreated, sometimes also treated, are regularly associated with this.
These include, for example.
- Wilson's disease (copper storage disease)
- hemochromatosis (iron storage disease)
- the alpha-1 antitrypsin deficiency
- Glycogen storage diseases
and - cystic fibrosis. However, this clinical picture is very rare.
Last but not least, diseases of the vascular system such as cirrhosis cardiaque, Budd-Chiari syndrome and Osler's disease are to be cited as the cause of liver failure.
Read more about the rare liver disease at: Budd-Chiari Syndrome
Symptoms

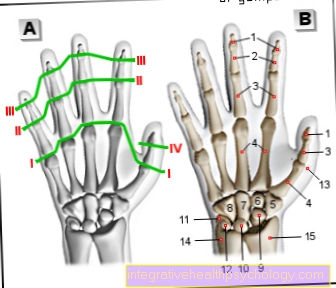
With liver insufficiency, unspecific symptoms such as fatigue or upper abdominal discomfort occur. Diffuse itching and jaundice (skin and scleric terus) can occur. The cause of the itching is not yet fully understood. Due to the deposition of metabolic products of bilirubin (a breakdown product of the blood) in the skin and the sclera, it turns yellow. In the case of underlying liver cirrhosis, the typical liver skin signs such as palmar and plantar erythema (rashes on the palm or back of the hand), spider naevi (fine vascular drawings) or the caput medusae (expansion of veins in the area of the navel) appear. However, these hepatic skin signs are not mandatory for hepatic insufficiency.
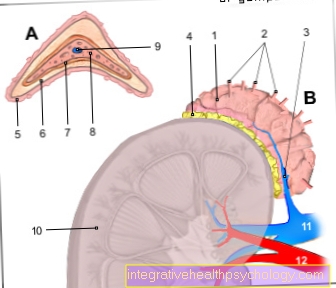
The liver failure leads to a limitation of important metabolic functions of the liver. There is a coagulation disorder in the sense of an increased tendency to bleed, as fewer coagulation factors are formed in the liver. In addition, there is an albumin deficiency, which leads to edema and ascites (Ascites) leads. Furthermore, increased pressure (portal hypertension) in the liver vein (Portal vein) to the formation of esophageal varices (expansion of veins in the esophagus) and sometimes to life-threatening bleeding up to volume deficiency shock. Such portal hypertension results, for example, from cirrhosis of the liver that has existed for years.
In addition, liver insufficiency leads to a mismatch between testosterone and estrogen, so that gynecomastia (feminization) and a loss of secondary hair in the sense of balding stomach and chest can occur in men. These changes are due to a decrease in the hormonal effects of testosterone. In women, this disproportion leads to amenorrhea (lack of menstrual bleeding).
Both sexes are affected by libido and erectile dysfunction. In the case of liver insufficiency, the liver no longer performs important tasks, such as detoxifying ammonia, so that this metabolic product is increasingly deposited in the body. In the context of hepatic encephalopathy, this can lead to impaired consciousness and even hepatic coma. There are various restrictions of consciousness, a hand tremor (tremor) and in the worst case to a coma. Another complication of hepatic insufficiency is the hepatorenal syndrome, in which there is acute kidney failure with a decrease in urine output. The mechanism responsible for its formation is not yet fully understood.
diagnosis
In addition to the physical examination, the diagnosis of liver insufficiency includes laboratory diagnostics and the examination using apparatus. The physical examination may show signs of liver failure or indications of the underlying cause (e.g. cirrhosis of the liver). In the inspection (Observation), for example, skin and sclerenic terus (yellowing of the eyes), an increase in abdominal circumference due to ascites or classic liver skin signs such as a Palmar erythema (Rash on the palm) or Spider naevi (fine vessel drawings). However, these characters can also be missing.
The liver may be enlarged and palpable under the right costal arch (see also: swollen liver) and has a bumpy structure. In the final stage of liver cirrhosis, however, the liver is even reduced in size, in the sense of a shrink liver.
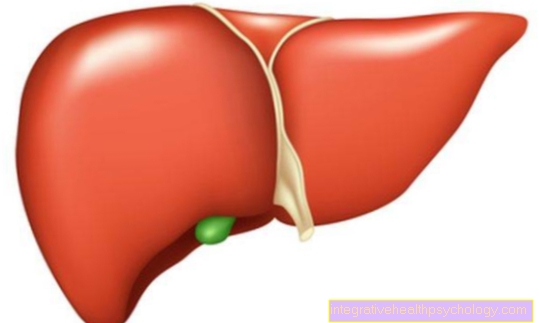
Laboratory diagnostics and imaging using sonography are more important than the physical examination. A blood sample is necessary for the laboratory, with the help of which one can infer the type and extent of the liver insufficiency via the increase / decrease of certain liver values and synthesis parameters (see section laboratory values). In the ultrasound examination (Sonography) can impress an enlarged organ. The liver contour is bumpy and the angle of the liver is rounded. The shape of the organ can be described as plump and biconvex. The tissue structure is inhomogeneous, which means that there are lighter and darker areas in the organ. This inhomogeneity can be very strong but also very subtle. In the advanced stage of liver cirrhosis, the organ is reduced in size by ultrasound findings. These descriptions are clearer if one compares a picture of a healthy liver with a picture of a liver with hepatic insufficiency. If the findings are unclear or to clarify a suspicious mass, e.g. a tumor, a CT of the liver can be performed. In exceptional cases, if the cause is unclear, a liver biopsy is performed to clarify the cause.
therapy
The treatment of liver insufficiency depends on both the cause and its severity. Sometimes there are acute events such as poisoning that can be remedied by an antidote or measures such as blood plasma separation. However, alcohol abuse in the context of alcohol-toxic liver damage or even alcoholic liver cirrhosis is very often to blame for the liver failure. Then the top priority is alcohol abstinence as a therapeutic measure.
Other causal diseases require special therapeutic measures. In hemochromatosis, for example, the bloodletting (draw a large amount of blood) in the first place, one treats Wilson's disease with Chelating agents (form non-absorbable complexes with the toxic copper). It is therefore important to treat the underlying disease.
Just as important is the clinical and outpatient management of the consequences and symptoms of liver insufficiency and the reduction of influences that can damage the liver. Medicines such as amiodarone or other hepatic influences (alcohol) must be reduced or, if necessary, discontinued. A balanced diet is also necessary. Contrary to the old doctrine, a protein restriction is not necessary. If there is a lack of coagulation factors, these can be substituted or vitamin K given. Ascites and other edema are treated with diuretics. If there is a pronounced lack of albumin, albumin can be substituted. If portal hypertension (high blood pressure in the hepatic vein) has occurred in the context of liver insufficiency, this can be reduced with a beta blocker (e.g. propanolol). This is important to the formation of bypass circuits that are too Esophageal varices (Varicose veins in the esophagus) can lead to prevention.
With complications like one hepatic encephalopathy (Damage or dysfunction of the brain due to severe liver damage) either outpatient or inpatient measures are necessary. That depends on the severity of the encephalopathy. Hepatic encephalopathy is brain damage caused by ammonia deposits. Circulatory stabilization, the avoidance of liver-toxic factors and the administration of Lactulose (Laxatives) are in the foreground here.
A hepatorenal syndrome, in which kidney failure occurs, requires intensive medical care and the administration of terlipressin and albumin. In the case of acute liver failure in the sense of the maximum form of liver insufficiency, intensive medical care is necessary.
If the liver insufficiency cannot be reversed by the above measures and the disease has progressed to the point that long-term liver failure occurs, only a liver transplant is curative. Replacement procedures such as liver dialysis can be used to bridge the time to organ transplantation. However, this is not a permanent solution.
These articles might also interest you:
- The diet in cirrhosis of the liver
- Liver transplant
Laboratory values / blood values
The determination of various laboratory parameters is essential for the diagnosis and therapy planning of liver insufficiency. First of all, a distinction is made between parameters that indicate liver tissue damage and those that detect a synthesis disorder (production of enzymes and proteins) in the liver. In addition, other blood values are used to assess the severity of the clinical picture.
Find out more about this topic here: The change in blood values.
1. Liver tissue damage
To assess the tissue damage to the liver, the so-called transaminases (GPT and GOT), the GLDH, the alkaline phosphatase, the gamma-GT, as well as the bilirubin and ammonia are determined. These parameters can be increased to different degrees and partially provide information about the cause of the liver failure. The gamma-GT is increased in the case of alcohol damage, for example, whereas an increase in alkaline phosphatase can be an indication of the presence of biliary cirrhosis. The standard values can be found in your laboratory results, as these are included as standard.
2. Synthesis performance
To assess the synthesis performance of the liver, the Quick value and INR, the albumin and total protein as well as the cholinesterase are determined. The Quick value and the INR are parameters for clotting in human blood. In the case of hepatic insufficiency, the Quick value may be reduced and the INR increased. These changes come about because the clotting factors are synthesized in the liver. In the case of liver insufficiency, they are reduced. The albumin is also reduced, since this is no longer sufficiently produced in the insufficient liver. Cholinesterase serves as a progression parameter in chronic liver diseases and is also reduced in liver insufficiency.
Find out more about the topic here: Cholinesterase deficiency
3. Other parameters
In the blood count, for example, cirrhosis of the liver can lead to a reduction in platelets (Thrombocytopenia) and one anemia (For example Vitamin B 12 deficiency) come. In the case of hepatic encephalopathy, special attention is paid to the determination of ammonia, glucose and electrolytes (e.g. potassium). In hepatorenal syndrome, there is an increase in serum creatinine.
More information can be found here: Bilirubin
Child-Pugh
The Child-Pugh criteria are used to assess the prognosis of liver cirrhosis. They are used to adjust the therapy and to better estimate the survival of the patient. There are five categories. For each of the categories between one and three points are awarded. The result is a maximum value of 15 and a minimum value of 5. The individual categories that are evaluated are the albumin concentration in serum (g / dl), the bilirubin concentration in the serum in mg / dl, the Quick value in% and that Presence and severity of ascites (water in the abdomen) and hepatic encephalopathy.
The albumin, bilirubin and the Quick value are a measure of how well the liver fulfills its metabolic and synthetic functions. In the case of hepatic insufficiency, the quick and the albumin are decreased and the bilirubin increased.
Ascites and hepatic encephalopathy are the consequences of liver failure and also indicate how severely impaired liver functions are. There are three stages of the Child-Pugh classification, namely Child A (5-6 points), Child B (7-9 points) and Child C (10-15 points). The higher the score, the worse the patient's prognosis.
Read on below: Stages of cirrhosis of the liver
Coagulation disorder
In the context of liver insufficiency, for example due to liver cirrhosis, an acquired coagulation disorder occurs. This tendency to bleed is called a hemorrhagic diathesis. This is due to the fact that important clotting factors are formed in the liver. If the liver does not perform well in its synthesis, there is a lack of coagulation factors.
These are primarily the coagulation factors II, VII, IX and X, which are formed in the liver as a function of vitamin K. This greatly increases the bleeding tendency. This can be particularly dangerous if esophageal varices are also present.
These are very common in people with cirrhosis and can cause life-threatening bleeding if they burst. Such a coagulation disorder is monitored with the help of the laboratory parameters INR and Quick value and treated by substituting coagulation factors.
Further information is available under our topic: Coagulation disorder and Xarelto®























.jpg)