The CSF loss syndrome
definition
The CSF loss syndrome is an increasingly common disease that is mainly presented by a so-called orthostatic headache. This is characterized by the fact that the pain increases significantly when standing, but becomes much milder or disappears completely when lying down. The cause of these symptoms is the loss of nerve water, which irritates the meninges. There are many different other names for this condition such as low CSF pressure syndorm, hypoliquorrhea, spontaneous intracranial hypotension, etc. that focus on different aspects of the condition.
The frequency of the disease is given as 5 out of 100,000 newly infected patients and is therefore not as rare as many doctors suspect. Women are affected about twice as often as men on average.

The symptoms
The main symptom of CSF loss syndrome is the so-called orthostatic headache, which is characterized by worsening pain when standing. This occurs, albeit with varying intensity, in all patients in the course of the disease. The intensity of this pain ranges from a light to moderate pulling in the neck to a severe traveling headache and neck pain.
In addition to the pain, other symptoms can occur, depending on the severity of the disease. These include nausea, dizziness, sensitivity to light and noise, but also more severe neurological deficits such as impaired vision or hearing impairment. If there is no rapid treatment of the CSF loss, this can ultimately lead to a loss of consciousness.
The headache in CSF loss syndrome
The headaches that occur as part of a CSF loss syndrome are described as orthostatic and thus show a dependence on the position of the body. While there are almost no complaints when lying down, the intensity of the pain increases significantly when standing or sitting.
This phenomenon is due to the increased loss of CSF while standing upright. Since the brain and spinal cord normally “swim” in this CSF, a loss of this fluid causes the tissue to sink. However, since the meninges are fixed to bony structures, a tensile force occurs, which is perceived as a severe headache. The pain usually affects the entire head and often spreads to the neck.
Find out more about the topic here: The headache.
The reasons
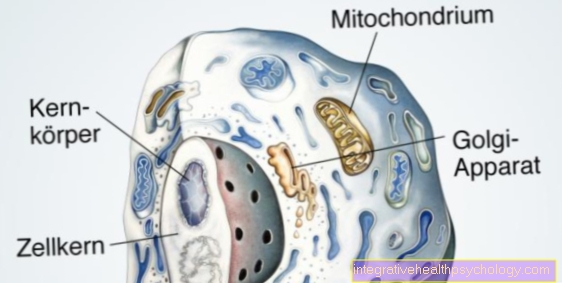
Our brain and spinal cord are constantly surrounded by nerve water, the so-called liquor. Above all, this has a protective function, as it can prevent pinching or pressure effects on the tissue.The formation and breakdown of this liquor is an ongoing process. Around 500ml of this liquid is formed and broken down again every day. The nervous system and the liquor are surrounded by the closed system of the meninges.
A CSF loss syndrome occurs when large amounts of this fluid are lost through a so-called CSF fistula. The term liquor fistula refers to all defects that allow liquor to escape from the surrounding meninges. Often these occur in the form of small tears on the meninges of the spinal cord, which then leads to loss of CSF. This loss is now intensified, especially when standing, as gravity pushes the liquor downwards and it can therefore increasingly drain out of the small crack. There is no such pressure when lying down, which is why only very small amounts can flow off.
The loss of the cerebrospinal fluid now leads to a subsidence of the brain tissue, which leads to tension in the meninges, which is perceived as a headache. The strongly varying strength of this headache is largely dependent on the size of the crack. If this is only 1 millimeter in size, those affected only report mild headaches that get worse when standing. In the case of large defects, on the other hand, patients can often no longer stand up or lift their head in pain.
Find out all about the topic here: The nerve water.
The diagnosis
The clinical picture of the disease alone can give the examining physicians a clear indication of the presence of a CSF loss syndrome. Depending on the extent of this loss, in addition to severe headaches, impaired vision or impaired consciousness can occur. In most cases, this clinical picture leads to a rapid implementation of an imaging procedure, usually an MRI.
With the help of this examination, on the one hand the leaked liquor, but also the "sagging" of the brain can be shown. In addition, the inner cerebrospinal fluid spaces of the brain are clearly narrowed.
However, it is often more complicated to look for the crack. This is often very difficult to visualize in imaging and requires an experienced radiologist and often the use of other diagnostic measures such as ultrasound or a lumbar puncture.
MRI of the lumbar spine
As part of the diagnosis of CSF loss syndrome, an MRI of the lumbar spine (lumbar spine) is performed in almost all cases. If the disease is present, some groundbreaking signs can be displayed. On the one hand, an accumulation of liquor outside the meninges can often be detected, which makes the presence of a liquor fistula very likely. A congestion of the veins of the meninges is also often detectable.
In some cases, the liquor fistula can also be shown, even if other imaging methods are usually used.
Find out more about the topic here: MRI of the lumbar spine.
The treatment
The treatment of the CSF loss syndrome is a so-called step-by-step scheme. In most cases, a conservative, wait-and-see treatment attempt with bed rest for 3 days is carried out first. It is not uncommon for the CSF fistula to close spontaneously during this period.
If this is not the case, a so-called lumbar blood patch is carried out in the next step. In this procedure, a mixture of autologous blood and radiopaque contrast agent is injected into the space around the membranes of the spinal cord (epidural space). This accumulation of fluid now presses on the causal open defect of the skin of the spinal cord and in many cases leads to a complete regression of the symptoms. The correct position of the injected liquid is ensured by means of an X-ray. Performing this procedure is usually simple and can be carried out on the ward.
In cases in which this treatment option has not been able to achieve freedom from symptoms, surgical intervention is now available as the last treatment option. This is usually performed microsurgically and the tear is closed with a seam or adhesive. In very severe cases of CSF loss syndrome and symptoms that are already severe at the beginning, surgery can be used as the first treatment option. In most cases, symptoms can be expected immediately after the operation.
When do you need a blood patch?
Blood patches are always used when, after adequate bed rest, the CSF fistula has not spontaneously closed. This procedure is often given preference over surgical measures due to its simple implementation and extremely low complication rates. A mixture of autologous blood, taken from the vein, and X-ray contrast medium serves as a blood patch. The latter enables a subsequent position control of the blood patch.
The claim rate for this form of treatment is around 85%. In case of non-response, the procedure can be repeated several times. In addition to the lumbar blood patch, in which the entire epidural space (gap in the spinal cord) is filled, a more local application of this therapy is possible. However, this requires an exact localization of the defect.
The duration
The duration of CSF loss syndrome can vary significantly. While patients with minor effects due to the mild symptoms do not seek to see a specialist until after a few days, the disease is much more acute in many patients, which often results in hospitalization. In most cases, the clinical picture is diagnosed quickly and the necessary treatment measures are sought.
Depending on the response to the various forms of therapy, the average duration of the illness is between 3-5 days. If left untreated, the course of the disease can be significantly longer and the symptoms become more and more pronounced.
Prognosis
The prognosis for CSF loss syndrome is very good. Various operative and non-operative therapy options are available in the treatment of the disease, which show good to very good claim rates.
Furthermore, the complication rates of the treatment options are to be assessed as low and symptoms are often cleared quickly after responding to therapy.