Melanoma
definition
Malignant melanoma is a highly malignant tumor that quickly metastasizes to other organs. As the name suggests, it starts from the skin's melanocytes. Almost 50% of all melanomas develop from pigmented birthmarks. However, they can also arise "spontaneously" on completely inconspicuous skin.

Occurrence in the population (epidemiology)
Melanoma is the tumor with the highest rate of incidence in the world.
In Germany the so-called incidence increases by 8% every year. Incidence rates (melanoma / 100,000 population / year) are lowest in sub-Saharan Africa at 0.1. Australia has the highest incidence rate at 60.
In Germany the incidence is around 12 / 100,000 inhabitants / year.
Due to improved early detection, mortality could be reduced to 20% of all cases. Most melanomas are discovered between the ages of 30 and 70.
Causes of Melanoma

There are different Risk factors the development of melanoma. A malignant (malicious) melanoma can result from one that has existed for years Mole / birthmark (Nevus cell nevus) develop.
It can also arise from completely inconspicuous skin. For example, play genetic factors a role.
There is an increased risk of melanoma development in FANN repair damage (see below), or familial accumulation of melanoma. Also acquired factors, such as severe sunburn, can promote the emergence.
It is estimated that the distribution of causes is as follows:
- 30 to 70% of melanomas arise from long-standing moles
- 30 to 70% the melanomas arise on inconspicuous skin
- 10 to 20% Melanomas develop after years from a melanotic precancerous condition = cancer precursors (e.g. lentigo maligna).
In this case, a precancerous condition is a change in the skin that can possibly degenerate into a tumor. - 10% of melanomas occur in families:
In the context of familial melanomas, there are various nevi (birthmarks) that can be considered: - Clark nevus
- Familial atypical nevus and melanoma (FAMM) syndrome
Melanoma staging
Malignant melanoma is divided into 5 stages according to the so-called TNM classification. This classification is based on the following three criteria:
- The tumor thickness (T). It is important to determine how deep the tumor has penetrated the skin.The risk of metastasis is very low below one millimeter, whereas above 4 mm there is a very high probability of metastasis of the malignant skin tumor. The reason for this is the connection of the tumor to the blood and lymph vessels, which are located in the deeper layers of the skin and over which the tumor can spread.
- The involvement of regional lymph nodes (N). These are the lymph nodes closest to the tumor. Due to their location in relation to the tumor, they are the first station to be affected by metastasis and are therefore a good indicator of the stage of malignant melanoma. A distinction is made between metastases that are only visible under the microscope and metastases that have already led to a palpable or visible enlargement of the lymph nodes.
- The distant metastases (M). This means the spread of the tumor to other parts of the body. In malignant melanoma, there are no preferred organs that are metastasized, as is typical for other tumors. It can occur in the liver, lungs, brain, bones and skin. The peculiarity of the malignant melanoma is the metastasis in the heart. Since a malignant disease of the heart is very rare, this metastasis accounts for about 50% of all heart tumors.
In addition to these three main criteria, there are two additional criteria that serve to subdivide the 5 stages:
- The rates of mitosis. This criterion describes the number of cell divisions of the tumor and thus its activity. This measurand is particularly relevant for the prognosis for tumors with a thickness of less than 1 mm.
- The ulcerations. This is the characteristic of the tumor to trigger deep skin damage that resembles a wound or an ulcer. The more pronounced this process, the more advanced the tumor.
According to these criteria, stage 0 corresponds to a tumor that only grows locally and has a low mitotic rate without metastasizing. In stage I, the tumor thickness is <2mm and there are neither lymph nodes involved nor distant metastases. Stage II differs from the fact that the tumor is now> 2mm. From stage III, the lymph nodes are also involved, but there are no distant metastases. Distant metastases are only present from stage IV. The lower the stage, the better the prognosis.
The prognosis for melanoma
The prognosis of the malignant melanoma depends on its stage, as well as the metastasis and numerous other factors.
These include:
- the tumor thickness (divided according to Breslow)
- the ulceration of the tumor and
- the penetration depth (after the Clark level)
In addition, the individual subtypes of melanoma have different chances of recovery, for example lentigo maligna melanoma (LMM) has a better prognosis than amelanotic melanoma (AMM). In addition, tumor location and gender are factors in the prognosis. Men generally have a worse prognosis than women. Overall, amelanotic melanoma has a very poor prognosis, regardless of gender and location. In contrast, the darkness of the melanoma usually has no influence on the prognosis.
In general, with an early diagnosis, the chances of recovery are very good, especially if it is an "in-situ melanoma". This has not yet crossed the basement membrane (the boundary between the upper skin (epidermis) and the dermis), but it is already recognizable as potentially dangerous.
That is why it is important to have regular skin cancer checkups.
Read more on the subject at: How do you recognize skin cancer?
The reason for the good prognosis is that in this case still no metastasis has taken place. The division of the prognosis according to tumor stage is based on the 5-year survival rate. This indicates the proportion of patients who were still alive 5 years after the diagnosis.
- In stage I. the chance of recovery is> 90%. The primary tumor is a maximum of 1.5mm thick and has a Clark level of <III.
- In stage II the primary tumor is> 1.5mm thick and has a Clark level of> IV. At this stage, the 5-year survival rate is 70%.
- In stage III has the tumor already in the nearest one Lymph nodes metastasized, or new skin metastases formed. The tumor thickness and Clark level are irrelevant here. The 5-year survival rate is 40%.
- Does the tumor scattered in organs further away, so lie Stage IV and a 10% chance of survival.
The metastatic routes are in one malignant melanoma very different and can therefore occur in all organs. However, metastases are often found in liver, skin, lung, skeleton, heart or brain.
Metastases in the liver or the brain in particular have a negative impact on the prognosis. In contrast, lung metastases often grow very slowly and are therefore easier to treat. The malignant tumors of the heart in particular are very rare and are found in 40-60% of cases as a metastasis of a malignant melanoma.
Basically, only the early, complete removal of the melanoma can lead to healing. Waiting, however, significantly worsens the forecast.
Note: For this reason, regular preventive examinations and early detection measures are very important.
Types and symptoms of melanoma
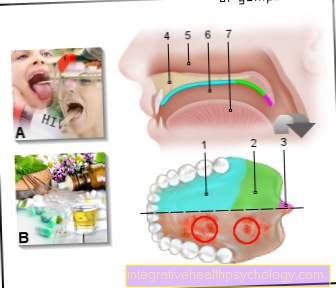
There are four classic growth forms and special forms of melanoma. All melanomas follow the ABCD rule in terms of their irregularity. The contour (asymmetry), boundary, color (coloring) and size (diameter,> 5mm) are assessed according to this rule. Symptoms may include itching and spontaneous bleeding.
The four classic growth forms are described below.
-
Superficial Spreading Malignant Melanoma (SSM)
-
Primary nodular malignant melanoma (NMM)
-
Lentigo Malignant Melanoma (LMM)
-
Acrolentiginous Malignant Melanoma (ALM)
Superficial Spreading Malignant Melanoma (SSM)

(superficial = superficial, malignant = malignant)
As described above, the melanomas in their initial phase follow a horizontal growth (growth in width) within the epidermis (epidermis). This growth phase takes about 5 to 7 years, that is for a relatively long time, which is why the early detection rate is steadily increasing.
They're getting more and more Early forms, the so-called "Melanoma in situ“, Discovered with a relatively good prognosis. The "melanoma in situ" represents an increased growth of melanocytes within the epidermis.
This growth is accompanied by the development of atypical cells. The morph (the appearance) of the ssuperficial spreitendes malignant M.elanom (SSM) is very different. It ranges from light brown to brownish-black and is initially a flat focus, which later shows nodules or lumps.
There is one in the lighter areas of the tumor Immune reaction in front.
The relative frequency of this clinical picture is 65%, whereby Areas of the skin that are often exposed to the sun (e.g. face), are particularly affected.
The mean age of onset is around 50 years.
Primary nodular malignant melanoma
(nodular = nodular, malignant = malignant)
This type of melanoma appears more aggressive to be, because this is where the vertical growth phase into the deep. That primarily nodular malignes M.elanom (NMM) consists of a fast - within months - growing node, which is usually dark brown - black, often with a piebald pattern.
The melanoma cells form this node in the dermis (sclera). Hardly any tumor parts can be found in the epidermis.
The relative frequency this clinical picture is 15%. Here too, as in superficial spreading malignant melanoma (SSM), areas of the skin exposed to the sun are particularly affected. The mean age of onset of 55 years is also close to that of superficial spreading malignant melanoma (SSM).
Lentigo Malignant Melanoma (LMM)
Under one Lentigo maligna one understands one Increase in atypical melanocytes within the epidermis (upper skin). These cells have a tendency to develop into a lentigo malignant melanoma (LMM).
Lentigo maligna can grow horizontally as a precancerous condition for years - even decades.
The transition to the vertical growth phase (deep growth) and thus to lentigo maligna melanoma is characterized by the formation of small nodules. In this area, the tumor cells expand vertically in both directions.
The forecast is because of the long horizontal growth quite good.
The relative frequency this clinical picture is 10%, especially that face and the back of Hand are affected.
The mean age of onset is 68 years, significantly higher than for Superficial spreading malignant melanoma (SSM) and Primary nodular malignant melanoma (NMM).
Acrolentiginous malignant melanoma
(Akren = hands, feet, nose ears; malignant = malignant; lentigines = spots, similar to freckles, but larger and darker)
With this one rather rare melanoma First horizontal growth comes to the fore, later described vertical growth with Formation of blackish knots. This disease is similar in appearance and growth Lentigo Malignant Melanoma (LMM).
With dark-skinned peoples that is Acrolentiginous Malignant Melanoma (ALM) the most common type of melanoma. Because their localization is not always easily accessible, ALM is often diagnosed late and therefore has one accordingly unfavorable prognosis.
The relative frequency this clinical picture is 5%. The acra = body ends are particularly affected (Hand, foot, nose, ear...) and the nail beds.
The mean age of onset is 63 years.
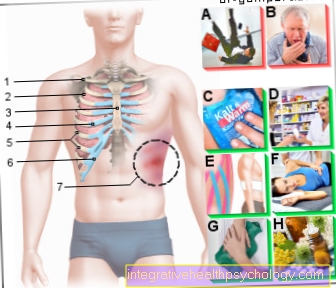
Treatment for melanoma

The first and most important measure in the case of a malignant melanoma is its complete removal, whereby a sufficient safety distance must be observed so that no residual tissue, which is not visible at first glance, remains and leads to further growth of the melanoma. Surgical removal is only avoided in elderly people in a far advanced stage of malignant melanoma with no chance of recovery. In the case of particularly large melanomas, a skin transplant may be necessary, which is possible either as a personal donation or an external donation. In addition, the so-called sentinel lymph node, i.e. the lymph node that is first in the lymphatic drainage area of the melanoma, is removed. To do this, it is marked with the radioactive substance technetium 99 and removed through a small skin incision. This is then also examined to rule out metastasis. If metastasis is found in this sentinel lymph node, the other lymph node stations are also removed and examined. If a lymph node is already enlarged, the entire lymph node region is removed without first examining the sentinel lymph node.
Further therapy depends on the stage of the disease and is determined both by the tissue examination of the surgically removed melanoma and by the examination for distant metastases.
There are several attempts to treat malignant melanoma in addition to surgical removal:
- Chemotherapy: Chemotherapy is used when distant metastases are already present. There is the option of carrying out the therapy with only one drug or a scheme of two or three different drugs. Combination therapy is only possible if the physical condition allows this increased stress. Combination therapy speaks for 25-55% of those treated. If only one drug is administered, only 14-33% will benefit from the therapy, but significantly fewer side effects are to be expected. A cure cannot be achieved with chemotherapy.
- Interferon therapy: Interferons are proteins that occur naturally in the body and are also given to the body during this therapy. They activate the natural killer cells in the body that can actively destroy cancer cells. In addition to surgery, interferon therapy is currently an effective and approved method in the treatment of melanoma.
- Radiation therapy: Radiation therapy is used for inoperable tumors and inoperable lymph node metastases. Visible tumor residues after surgical removal are also irradiated. In 70% of the cases the tumor can be kept under control, but radiation therapy is not able to cure the disease either.
- Vaccines: For treatment with a vaccine, cancer cells are removed from the patient, modified in the laboratory and then given again in a modified form. The body should destroy these modified cells and thereby better recognize and also destroy the other cancer cells in the body. So far this therapy has not led to any success.
- Antibody therapy: A new method tries to produce specific antibodies in the laboratory against surface proteins of tumor cells. These antibodies bind to the tumor cell and cause it to be broken down by the immune system. The antibody ipilimumab was found to be effective against malignant melanoma. The therapy only works in every sixth patient and is associated with many side effects. Therefore, this option for the treatment of melanoma can only be recommended to a limited extent.
- Mistletoe therapy: Mistletoe is a plant that is able to influence the immune system. This effect should be used to treat tumors, but mistletoe therapy is suspected of promoting tumor growth and should therefore not be used.
- Hyperthermic extremity perfusion: With this method, high doses of chemotherapy drugs are directed into the bloodstream of one extremity, which is tied off from the rest of the body during the treatment. In addition, this part of the body is overheated in order to destroy cells due to the high temperature. The advantage is that by separating the extremity from the body, you can choose a significantly higher dose of chemotherapy that the body would normally not tolerate. Since the separation from the circulatory system can result in an amputation of the relevant body part as a complication, this method is only used very rarely and only for certain types of tumors. This treatment option is not recommended for lymph node metastases.
- Immune stimulation: The goal of immune stimulation is to attack the body against foreign cells, especially cancer cells. The drugs levamisole and BCG tested so far are not able to target the body to the destruction of tumor cells. Therefore, the therapy is ineffective and is not recommended.
Surgical removal of the melanoma and / or therapy with interferons remain the means of choice.
Read more on the topic: Melanoma therapy
Summary

Malignant melanoma is one of the most dangerous cancers.
Melanomas are therefore malignant, rapidly metastasizing Tumorsthat of Melanocytes go out. Melanocytes are cells in the skin that make the pigment Melanin have saved. Melanin causes, among other things, the tanning of the skin.
This tumor spreads very quickly and early on via the lymphatic system (lymph) and the blood. That fact makes it so dangerous. Other skin tumors, such as this Basalioma scatter very rarely, which makes them relatively harmless in comparison.
Depending on the type of melanoma, the biological behavior of the tumors also differs. Some metastasize more often than others.
The course, however, is the same for all melanomas. They develop from a single cell clone, which is predisposed to degenerate, from which the primary tumor develops.
This first grows within the epidermis (epidermis), the so-called melanoma in situ, and later when it reaches the basement membrane skin broke through as an invasive melanoma. This growth is called vertical growth. The more superficial the melanoma in the skin is ingrown, the greater the chance of recovery.
People with sun sensitive skin are more at risk than others. Red-blonde hair and one accordingly light skin tone bring one almost five times higher Risiko with black hair with darker skin tone.















.jpg)