Genetic diseases
definition
A genetic disease or hereditary disease is a disease that is caused by one or more genes of the person concerned. The DNA acts here as a direct trigger of the disease. For most genetic diseases, the causative gene locations are known. If a genetic disease is suspected, the respective diagnosis can therefore be made through a genetic examination.
On the other hand, there are also a number of diseases whose occurrence has a genetic influence or is discussed, such as diabetes mellitus (“diabetes”), osteoporosis or depression. These are so-called dispositions, i.e. an increased likelihood of certain diseases. Dispositions are to be distinguished from hereditary diseases.

These are common hereditary diseases
In absolute terms, hereditary diseases are not common, but the hereditary diseases listed here occur frequently in comparison to other diseases of genetic cause.
-
Marfan's Syndrome
-
Sickle cell anemia
-
Hemophilia (hemophilia A or B)
-
Factor V Leiden mutation and resulting APC resistance
-
Red Green weakness
-
Glucose-6-phosphate dehydrogenase deficiency (G6PD deficiency)
-
Polydactyly ("multiple fingers", also possible as a symptom in other diseases)
-
Trisomy 21 (Down syndrome)
-
Chorea huntington
causes
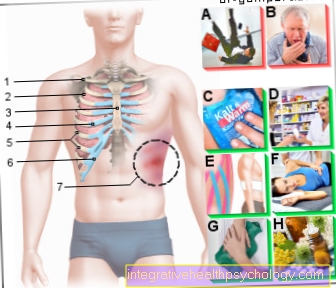
Hereditary diseases are extremely diverse in their appearance. They basically only have one thing in common: The cause for each of them lies in the DNA, i.e. in the genetic material of the person concerned. Various changes can occur here, such as mutations (exchange of DNA information) or deletions (lack of certain genetic material).
A large amount of information is encoded in the genetic material, such as the “blueprints” for various components that are important for the functioning of a body cell. These can be enzymes, electrolyte channels or messenger substances, for example. These smallest elements are then read incorrectly or not at all from the DNA, which is then missing in the sophisticated system of the body. The wrong or missing genetic information therefore causes certain malfunctions in the body. These then cause symptoms according to the functional system in which one element is now missing.
Find out all about the topic here: The genetic test.
This is how hereditary diseases are inherited
Every hereditary disease is inherited either monogenetically or polygenetically: This means that there is one or more genetic locations that have to be changed in order to lead to a disease.
Furthermore, genetic traits can always be inherited in a dominant or recessive manner: Recessive means that there must be a predisposition for this particular hereditary disease in both the paternal and maternal genes. In the case of dominant inheritance, one change (i.e. one parent) is enough to trigger the disease. It follows that with dominantly inherited diseases, the people who are carriers will also become ill - while with a recessive inheritance it is usually not even known that a corresponding genetic predisposition is present.
There are also diseases that are inherited through the sex chromosomes, such as hemophilia or red-green blindness. The facilities for this are usually on the X chromosome, since the Y chromosome is very small overall and can generally store little genetic information. One therefore speaks of X-linked inherited diseases. These usually affect significantly more men than women, as women can compensate for any incorrect information on the X chromosome with the second.
How exactly a genetic disease is inherited is usually easy to research if you are interested.
Tests before birth
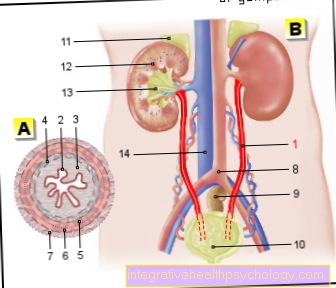
In principle, the child's genetic material can already be examined in the womb for all hereditary diseases whose causal genetic locations are known. However, genetic analyzes are time-consuming, so usually only the suspected gene location is analyzed - for this, in turn, there must be a justified suspicion of a genetic disease.
For such an examination, genetic material can then be taken from the amniotic fluid or the placenta and used for the analysis.
However, it should always be borne in mind that any invasive diagnosis also involves a risk to the life of the unborn child. Such punctures must therefore be weighed individually in each case.
There are also measurements that can indicate a genetic disease, such as the measurement of the nuchal transparency as a sign of trisomy 21. Such methods are not dangerous for the unborn child, but cannot offer absolute certainty that a genetic disease is present. So here too, an operation must be carefully considered.
Trisomy 21
The cause of trisomy 21 is chromosome 21, which is not present twice but three times in affected persons. This variant of the DNA is created when the chromosomes are distributed in the parental germ cells, i.e. the sperm or egg cells. It is therefore a "distribution error" and not a change in the actual genetic material. This explains why trisomy 21 can occur spontaneously in every family and why the probability of having a child with Down syndrome is the same in all families. Strictly speaking, trisomy 21 - like other trisomies - should not be counted as a hereditary disease in the true sense. Nevertheless, trisomy 21 is the most common DNA-related disease in newborns.
Features of the changed set of chromosomes in Down syndrome can already be seen in the unborn child in the womb: Growth delays and defects can lead to, among other things, a skull that is too small, short bones of the thigh and upper arm and heart defects. A large amount of amniotic fluid can also be an indication of trisomy 21, since affected unborn children drink or swallow relatively little amniotic fluid. However, none of these features are definitive signs of Down syndrome!
In addition to the signs of growth retardation mentioned, children with Down syndrome often also show delayed development, for example in the areas of language and motor skills. People affected by Down syndrome often show remarkable social skills, while intelligence often remains below average. However, affected people differ greatly in these characteristics; it is not uncommon for them to graduate from school after receiving good support.
Later in life, people with trisomy 21 have an increased risk of being diagnosed with certain diseases. These include Alzheimer's disease, epilepsy and cancer, particularly leukemia. Nevertheless, the life expectancy of people with Down syndrome continues to rise: In the meantime, affected people often reach the age of 60 or 70.
You can find more information on our website Down syndrom
Alpha-1 antitrypsin deficiency
Alpha-1 antitrypsin deficiency can take different forms and forms, depending on the exact genetic characteristics of the person affected. This means that not every alpha-1 antitrypsin deficiency leads to symptoms. In the following, only the clinically conspicuous type (PiZZ) of this genetically determined disease will be discussed.
The enzyme defect present in this disease causes the breakdown and remodeling of building blocks in the organ tissue in affected persons. In addition, the defective proteins are filtered out of the blood by the liver and accumulate there. This can lead to inflammation of the liver (hepatitis), cirrhosis or liver cancer. The airways in the lungs become unstable due to the lack of stable tissue and they collapse more quickly: The clinical picture of COPD (chronic obstructive pulmonary disease) develops. This clinical picture is often the first symptom of alpha-1 antitrypsin deficiency, so any person with COPD at a younger age should be checked for alpha-1 antitrypsin deficiency.
If the illness has persisted for a long time, the lungs may overinflate, as the air you breathe cannot be properly exhaled through the unstable airways and accumulates in the lungs. As a therapy, in addition to consistently avoiding cigarette smoking and regular vaccinations to prevent respiratory diseases, medicinal measures should also be taken: The missing alpha-1-antitrypsin can be administered intravenously in order to alleviate the symptoms as far as possible and to stop the course of the disease.
You can find more information on our website Alpha-1 antitrypsin deficiency
hemophilia
The group of hemophilia is also known colloquially as “hemophilia”, as this term describes the main symptom of this hereditary disease very precisely: the affected people bleed longer and, depending on the severity of the disease, more often than unaffected.
Bleeding is usually stopped by what is known as the coagulation cascade, an endogenous signaling pathway that prevents excessive blood loss. In this coagulation system, 13 factors play a role, which activate each other one after the other. This can be imagined as a series of dominoes: if you hit one stone (coagulation factor), it activates the next, and so on. At the end of this signal path or the dominoes there is blood coagulation. With hemophilia, a certain factor is missing - depending on the specific subtype of the disease: the chain reaction breaks off here.
Therapy for the disease can be carried out by determining the missing factor and adding it from outside. Affected people must therefore regularly inject themselves with a preparation with this coagulation factor so that the rest of the chain reaction can take place.
You can find more information on our website Blood disease
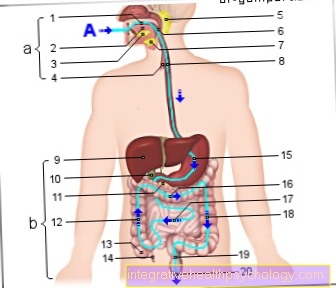
Cystic fibrosis
In the genetic disease cystic fibrosis - also known as cystic fibrosis - there is a faulty production of ion channels, more precisely of chloride channels. As a result, the composition of the body secretions (e.g. sweat, secretions from the respiratory tract and the pancreas) of the affected persons is changed: Since the lack of chloride means that less water is drawn into the duct of the respective gland, the secretion is relatively viscous.
As a result, symptoms usually develop in the digestive tract, as the secretion with the digestive enzymes cannot flow well from the pancreas into the intestine and thus damages the pancreas itself. In addition, digestive disorders such as fatty stools, diarrhea and the resulting low body weight are common.
The second large group of symptoms usually develops in the lungs: Since the mucus that naturally occurs in the lungs is more viscous than in healthy people, it is more difficult to remove it from the cilia. This can lead to chronic coughing and blockages of the bronchi (bronchiectasis). The larger amount of lung secretion also provides a good environment for the growth of bacteria, which results in frequent respiratory infections and pneumonia.
Cystic fibrosis is treated symptomatically with expectorants, digestive enzymes and antibiotics for infections.
You can find more about this on our website Cystic fibrosis
Factor V Leiden and APC Resistance
A factor V Leiden mutation involves a change in genetic information that can cause increased blood clotting. The reason for this is factor V in the body's so-called coagulation cascade: this signal path ensures that in the event of an injury, the wound is closed by the body's own "adhesive proteins" (fibrin). There are 13 factors in this signaling path, which are named with Roman numerals (it means “Factor 5 suffering”!). The factor V has a beneficial effect on the formation of a fibrin plug, but can also be inhibited by the so-called activated protein C (APC for short). This plays an important role in regulating this signaling pathway and in preventing excessive blood clotting.
The mutated factor V is present in the affected individuals but does not respond to the APC. The body lacks an important "safety device" at this point to prevent blood clotting for no reason, which may even block vessels and thereby cause circulatory disorders.
Statistically speaking, people who are affected by a factor V Leiden mutation are more likely to experience a thrombotic event (i.e. a thrombosis or pulmonary embolism), even without a history of typical risk factors. In technical terms, one also speaks of “thrombophilia”, ie a tendency to clot.
You can find more about this on our website Factor V Leiden
Gaucher disease
In Gaucher's disease, the change in the DNA information causes a defect in an enzyme involved in lipid metabolism, more precisely glucocerebrosidase: This helps break down old cell components. In the event of a defect, there can be a reduction in functionality or even a loss of functionality, and accordingly the symptoms appear in childhood or young adulthood.
The symptoms of Gaucher disease are largely due to an enlargement of the liver and spleen, the growth of which the body tries to compensate for the lack of enzymes. This increases the breakdown of all blood components, which can be recognized in the blood count and used as a diagnostic indicator together with the enlarged liver and spleen.
The missing enzyme glucocerebrosidase can be used therapeutically as a drug. The prognosis and course of Gaucher's disease depends largely on the severity of the enzyme's loss of function.
For more information, read on here: Gaucher's disease.
Osler's disease
Osler's disease is a hereditary disease that is characterized by a strong vasodilatation. In principle, this expansion of the vessels can occur anywhere, both on the skin and on internal organs. The walls of the enlarged vessels are relatively thin and tear easily. As a result, the affected areas bleed quickly.
The vasodilatation occurs particularly frequently on the face and in the nasal mucous membrane, so the affected people usually complain of frequent nosebleeds and small blotchy bleeding on the face.
If Osler's disease is suspected, appropriate diagnostics should be carried out, since the vasodilatation can also occur in vital organs or organs with good blood supply, such as the lungs, brain or liver, in which bleeding from a ruptured vessel is dangerous.
You can find more on this topic on our website Osler's disease
Recklinghausen's disease
Neurofibromatosis type 1 - or Recklinghausen's disease - is a genetic disease in which those affected often develop tumors on the cells of the nerve covering. The tumors that develop can be both benign and malignant and appear at a young age.
Typical tumors, however, are benign neurofibromas: These consist of cells that sheath and isolate the nerve like an electrical cable, as well as the surrounding connective tissue. They are benign, i.e. non-spreading and slowly growing tumors.
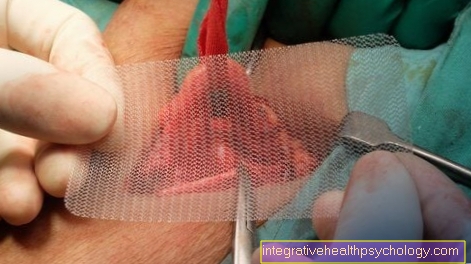
However, surgery to remove neurofibromas can be difficult, as they are often firmly attached to the nerve and the corresponding nerve then has to be removed. Nevertheless, this is the only treatment option for symptomatic neurofibroma, as causal therapy for this hereditary disease is not possible.
You can find more on this topic on our website Neurofibromatosis type 1
Muscular dystrophy
The term muscular dystrophy describes a group of hereditary diseases in which certain muscle components cannot or cannot be assembled correctly by the body cells. As a result, the affected people usually develop muscle weakness as early as childhood and adolescence, and this can result in a loss of muscle mass, movement restrictions and even physical disabilities.
If the presence of muscular dystrophy is suspected, blood values should first be determined. If the values match the suspected diagnosis, a muscle biopsy can still be performed: A small tissue sample is taken from the muscle, which is then examined microscopically for cellular defects. A genetic examination is also possible to establish the diagnosis, since the corresponding genetic locations are usually known for the various forms of muscular dystrophy and would have to be changed. A causal therapy for muscular dystrophies is not known.
You can find more on this topic on our website Muscular dystrophy
Xeroderma pigmentosum
Xeroderma pigmentosum is a rare hereditary disease in which certain enzymes in the skin of the affected person do not work. These enzymes normally take care of the repair in the DNA, which can be damaged by sunlight or the contained UVB light. The UVB damage can cause skin cancer in affected people as well as in all other people, but with Xeroderma Pigmentosum the process is accelerated by the lack of repair mechanisms. As a result, the affected people develop severe forms of skin cancer in childhood and adolescence and after a short exposure to sunlight.
A causal therapy is not yet possible. The affected people have to avoid sunlight for life, which is why the nickname "moonlight children" has established itself for the affected (sometimes very young) affected people. In addition, these people should be supervised by a dermatologist for regular skin cancer screening in order to remove newly developed skin cancer immediately. If these measures are strictly followed, the life expectancy of a person with xeroderma pigmentosum is about the same as that of an unaffected person.
You can find more about this disease on our website Xeroderma pigmentosum
Lynch Syndrome
Lynch syndrome is a change in DNA that causes a defective enzyme in the body's cells.In the affected people, a certain mechanism is therefore defective, which is otherwise supposed to protect the cells from degeneration, i.e. uncontrolled growth - people with Lynch syndrome therefore have a greatly increased risk of developing cancer.
Colon cancer often occurs because the cells naturally often divide here anyway and errors in the growth and death programming of a cell become apparent more quickly. Affected people often develop a tumor in the large intestine at an unusually young age, i.e. before the age of 50, which is then called HNPCC (hereditary non-polypous colon cancer). However, not everyone who has the genetic makeup of Lynch syndrome will develop colon cancer. On the other hand, other organs can also develop a tumor, since the genetic predispositions that favor the development of a tumor are present in all body cells. Regular checks and preventive examinations are therefore necessary for those affected by Lynch syndrome in order to adequately treat tumors that develop at an early stage.
You can find more on this topic on our website Lynch Syndrome
















.jpg)