Side effects of Marcumar®
Synonyms in a broader sense
- Phenprocoumon (active ingredient name)
- Coumarins
- Vitamin K antagonists (inhibitors)
- Anticoagulants
- Anticoagulants

Side effects of Marcumar®
Side effects (so-called ADRs, adverse drug effects) and interactions with other drugs
The most common undesirable effects of coumarin therapy are easier bleeding with bruising (hematoma).
Usually these are harmless (2-5% of patients), so stopping the drug is enough for the concentration of coagulation factors in the blood to rise again in two to three days.
Bleeding from the urinary tract or in stomachwhich can occur especially after overdosing.
Then the time until the new synthesis of the coagulation factors is insufficient and Vitamin K must be administered so that new coagulation factors can be formed immediately in the liver.
The coagulation then normalizes within a few hours. In (rare) emergencies, i.e. e.g. life-threatening bleeding within the brain, the missing coagulation factors are infused directly (administered as a concentrate via the vein).
Another very rare but serious complication of coumarin therapy is triggered by the initially increased coagulation:
Very small clots (so-called microthrombi) clog the smallest veins and capillaries that supply the skin and the underlying (Latin: subcutaneous) fatty tissue.
As a result, the affected cells die (medically: necrosis) and become bluish-black. This Circulatory disorder occurs three to eight days after the start of treatment with coumarins / Marcumar® and is initially noticeable as a painful reddening of the skin.
The treatment must then be stopped and continued with heparin, which, however, cannot be taken as a tablet, but only given by infusion directly into the vein.
A blue-speckled discoloration on the soles of the feet or toes can occur, but in contrast to the "coumarin necroses" described above, it is harmless and reversible:
This "Purple Toes Syndrome"(English: Purple Toes Syndrome") can occur after a long treatment with coumarins / Marcumar® for around three to eight weeks and is improved when the feet are raised. This side effect of coumarin / Marcumar® therapy is also rare.
Weight gain
In a survey by the health portal Sanego, 6% of 354 people reported weight gain in the course of treatment with Marcumar®. The extent to which there is a direct connection between weight gain and the drug is not fully understood. Loss of appetite has rarely been seen as a side effect that is more likely to be associated with weight loss. However, since everyone reacts individually to medication, weight gain cannot be ruled out.
Side effects on the intestines
The most important and most common side effects of treatment with Marcumar® are bleeding. These are mostly caused by overdosing. In principle, the bleeding can occur anywhere in the body. Occasionally there may be bleeding into the intestinal wall. Stool that is red or black may indicate bleeding from the gastrointestinal tract. You should definitely consult your doctor.
Liver side effects
Liver inflammation is a common side effect of treatment with Marcumar®. It can appear with or without jaundice. In some cases, liver tissue damage and liver failure have been observed as very rare side effects. In these cases, liver failure required liver transplantation or resulted in death. However, this happens very rarely. Regular checks of the liver and blood values and discussions with the doctor in the event of complaints or uncertainties reduce the risk.
Skin side effects / rash
Occasionally, a rash, red hives in the form of so-called hives, itching and skin inflammation occur during therapy with Marcumar®. In addition to the side effects on the skin, temporary diffuse hair loss can occasionally occur. Marcumar® inhibits all vitamin K-dependent factors. It also inhibits the so-called protein C. This protein has an anticoagulant function. So-called skin necrosis can arise due to the shorter half-life of protein C compared to the other vitamin K-dependent factors. Because when you start treatment with Marcumar ®, the protein C blood level falls first. This can lead to skin or vein thrombosis. To prevent this, heparin is initially administered. Serious skin damage with permanent disability or as a result of death can very rarely be recorded. Generally allergic skin reactions were also rarely observed.
fatigue
In a survey by the health portal Sanego, 6% of 354 people reported fatigue as a side effect in the course of Marcumar therapy. There may be a connection with changes in blood pressure since therapy. But it is also possible that the tiredness is influenced and caused by other factors. Depending on how severe the tiredness is, it can affect the person's ability to concentrate. Insufficient concentration can limit activities in everyday life or even endanger yourself or others. In these cases you should definitely consult your doctor.
impotence
In a survey by the health portal Sanego, 1% of 354 people reported impotence as a result of Marcumar treatment. To what extent there is a direct context to the drug and the impotence or whether other factors play a role in combination is still unclear. Not all authors state impotence as a side effect in the context of therapy with Marcumar®. For example, erectile dysfunction is not listed in the yellow list and in the manufacturer's technical information as side effects of treatment with Marcumar®. In the book “Manual of Impotence”, the author Prof. H. Porst writes that, among other things, erectile dysfunction would be possible with Marcumar®, but the mechanism of action is unclear.
Read more on the subject at: Causes of Erectile Dysfunction
Blood in the urine
Blood in the urine is a very common side effect of treatment with Marcumar®. This could possibly be a sign of overdose. The discoloration of the urine may indicate bleeding in the urogenital tract. Therefore, these should be reported to the attending physician in any case. It is advisable to check the blood coagulation values and possibly the kidneys. The dosage may have to be changed.
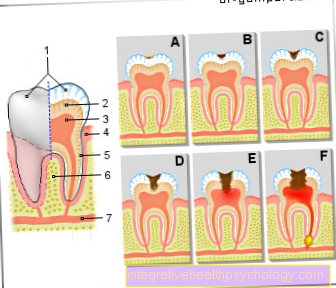
osteoporosis
After months of using Marcumar®, this can occasionally lead to a reduction in bone mass or what is known as osteoporosis. This is due to the fact that Marcumar® inhibits vitamin K. Vitamin K is necessary for the formation of the bone matrix. As a result, prolonged use of the drug can lead to a disturbance in bone metabolism. This increases the risk of fractures, especially for people with a corresponding disposition. However, a dose of vitamin K cannot, conversely, improve bone density.
Read more about the topic here: osteoporosis
sweat
In a survey by the health portal Sanego, 2% of 354 people said that they would sweat (increased) since treatment with Marcumar. Most of the time, they reported that they sweat faster than before the time of treatment. The extent to which there is a direct connection between sweating and therapy with Marcumar® is not fully understood. However, it cannot be ruled out that the drug may lead to altered vegetative processes in the body. As a result, this could also affect sweating.
When should Marcumar® not be given?
In the pregnancy allowed coumarins generally not be administered because serious damage can occur both in the early stages of child development ("embryopathies", third to eighth week of pregnancy) and in the later, usually less sensitive developmental stages ("fetopathies", from the ninth week of pregnancy) .
More on this topic at: Medication in Pregnancy
Also in the Lactation (see also Breastfeeding) must alternatively Heparin be used because Phenprocoumon (Marcumar®) is also used in the Breast milk accumulates and can cause bleeding in the child.
The only exception is the shorter-acting warfarin. In order to avoid dangerous bleeding due to overdose, the interaction of the coumarins with other drugs must also be considered:
The simultaneous administration of the used not only as pain relievers, but also for preventive anticoagulation after a heart attack Acetylsalicylic acid (ASS), leads to increased concentrations of coumarins in the blood and thus to an increase in effectiveness.
The reason for this is the high binding of both drug groups to transport proteins in the blood.
There Acetylsalicylic acid (aspirin) If the coumarins are displaced from the binding sites on the blood plasma proteins, the latter are increasingly released as unbound, active form and can develop their anticoagulant effect.The effectiveness of the coumarins / Marcumar® is also enhanced when drugs are taken in parallel that inhibit the production of acid in the stomach (antacids; these are used to prevent and / or treat gastric ulcers) as well as the absorption inhibitors of bile salts (example: colestyramine) Used to treat high cholesterol, as they block bile acids from being recycled in the body, thus lowering blood cholesterol.
Another mechanism of the Increased effectiveness, which has to be taken into account when dosing coumarins / Marcumar®, represents the increase in activity of those that break down the coumarins / Marcumar® liver - Enzymes from other drugs:
E.g. the allopurinol a drug against that gout, some Antibiotics and the one frequently used against cardiac arrhythmias Amiodarone (Cordarex) for an enhancement of the effectiveness of the coumarins / Marcumar®.
Also of great importance is the influence of a diet rich in vitamin K (this inhibits the coumarin effect) or diet low in vitamin K (the consequence is an increased tendency to bleeding; this can also be due to the influence of the anticoagulant effect) Bowel disease, Disorders of fat digestion can be triggered.
In newborns whose liver cannot yet form sufficient coagulation factors and those who cannot absorb sufficient vitamin K through breast milk in the first few days of life are therefore generally recommended to be given vitamin K before the fourth week of life.)
Alternatives to Marcumar®
In addition to coumarins / Marcumar®, the most frequently used anticoagulants are heparin, which can only be administered intravenously, and a mini-protein originally obtained from leeches (scientific name: Hirudo medicinalis), hirudin, which is negatively charged and produced in small quantities by the body itself (and therefore cannot be absorbed through the intestinal mucosa) Heparin is a mixture of two chemically differently structured sugar components (for those interested: a so-called disaccharide made from a glucosamine and a glucosuronic acid).
The anticoagulant effect of heparin consists in the 1000-fold increase (or acceleration) of an anti-coagulant naturally occurring in the blood, the antithrombin (which in the literature is often referred to as AT for short). Antithrombin itself inhibits the enzyme thrombin, which is essential for blood coagulation and cross-links the blood platelets with fibrin to close wounds, by forming inactive complexes with it.
Heparin itself is not a uniformly structured molecule, but comes in different sizes, so that two subgroups with different properties and applications can be distinguished: On the one hand, the "unfractionated" heparins consisting of larger building blocks (a molecule is between 6,000 and 30,000 times as heavy as a single hydrogen atom), which are given intravenously for treatment of pulmonary embolism, leg vein thrombosis and angina pectoris (see above) for anticoagulation.
On the other hand, there are “fractionated” heparins, also known as “low molecular weight” due to their smaller molecule size (these are always lighter than 6000 hydrogen atoms).
The chemical properties that differ from those of the high molecular weight heparins are the reason for the increasingly frequent use of this group of drugs: They only have to be injected under the skin (medical: subcutaneous) once a day, which is why they are also used regularly in outpatient settings (e.g. by the family doctor).
Furthermore, undesirable side effects are much less common: Examples of this are, in addition to the bleeding that may occur with all anticoagulants, the increased risk of osteoporosis (bone loss) and allergic reactions.
Osteoporosis is a systemic disease of the skeleton, which is characterized by reduced bone mass and disruption of the microarchitecture and which can e.g. noticeable through spontaneously occurring bone fractures, without a previous trauma / accident being able to explain the fracture / break.
The best protection against this disease, which mainly affects the female sex, is an adequate intake of calcium with food (this is mainly contained in milk) and an adequate supply of vitamin D (it is recommended to consume sea fish twice a week ). In addition, sufficient physical exercise should be ensured, as this promotes mineralization of the bone.
Long periods of deficiency in sex hormones should be avoided; If necessary, the estrogens required for bone metabolism can be used as part of hormone replacement therapy, e.g. in postmenopausal women; be substituted.
Further information can be found under our topic: Bone loss (osteoporosis)
In addition to osteoporosis, there are intolerance reactions that have been observed more and more frequently in recent years:
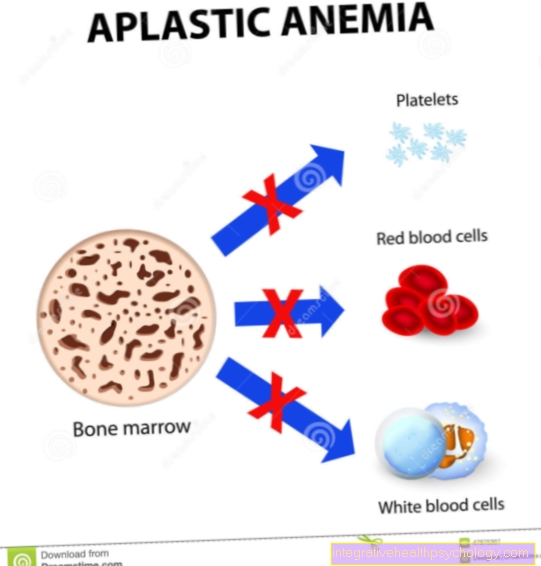
"Heparin-induced thrombocytopenias", or HIT's for short, are two clinical pictures in which platelets are destroyed due to a malfunction of the immune system. With less severe, reversible type 1 HITs, up to 30% of the platelets are usually lost early on at the start of heparin therapy.
On the other hand, type 2, which occurs in approx. 0.5 to 3% after the fifth to eleventh day after the start of therapy, is more severe, often life-threatening: In this process, the body's own proteins, which are formed by cells of the immune system and which otherwise cross-link during blood clotting, destroy blood platelets . The deadly effect (in up to 30% of patients) is less the heavy loss of blood platelets (the number contained in a micro-liter often drops from around 300,000 to below 50,000), but rather the massive release of coagulant substances from the vascular walls .
This is where the designation of HIT 2 as “White Clot Syndrome” comes from: Vascular occlusions in the arteries in the blood depleted in red platelets as well as clot formation in leg veins and pulmonary embolisms can be life-threatening.
To avoid these complications, therapy must be stopped immediately at the first warning signs of HIT and continued with another anticoagulant.
Hirudin, which used to be obtained from leeches, has proven itself, and today it can also be produced by genetic engineering (the substances obtained in this way were called "lepirudin" and "desirudin").
Hirudin is used to liquefy the blood of their host animals for the up to 15 cm large, olive-green colored annelids. The use of leeches to treat a wide variety of diseases was particularly widespread in 19th century medicine; Today, however, the leech is under nature protection in Europe and, according to the Washington Convention on Endangered Species, may only be collected with special permission. One advantage of hirudin over heparins is that it can be used in patients with HIT 2 with a rapid onset of action and that it is generally well tolerated, so that undesirable side effects are very rare.
The disadvantage, however, is the poorer controllability: unlike heparins, there is no antidote that would enable the anticoagulation to be terminated prematurely (the heparin effect can be neutralized by injecting the protein protamine obtained from salmon).
Read a lot more information on this topic at: Alternatives to Marcumar®