Pudendal Nerve - Course and Failure
definition
The pudendal nerve is a nerve that runs in the pelvic and genital areas. It is also known as the "pubic nerve". He is responsible for the motor innervation of muscles as well as for sensitive innervation, i.e. all tactile and pressure sensations, in the area from the anus to the genitals.

anatomy
The pudendal nerve has its origin in an interweaving of several nerves, which is also referred to as a plexus in medical terminology. This nerve plexus in turn originates in the lowest area of the spine, the sacrum, and the last vertebra of the lumbar spine adjacent to the top.
At the end of the nerve entanglement, four individual nerve cords emerge. One of these nerves is the pudendal nerve. In the following it moves through the basin, wanders through several openings and removes protrusions. It is accompanied by an artery and a vein. The nerve then pulls into the pudendal canal, also known as the 'Alcock' canal. In this canal, a strong layer of connective tissue is placed around the pudendal nerve and its accompanying vein and artery. This canal represents a constriction. When the pudendal nerve has finally passed through the 'Alcock' canal, it divides again into four further branches, its terminal branches.
These include the perineal nerves, the inferior rectales nerves, the dorsal penis nerve and the dorsal clitoral nerve. These different nerve cords run in different directions and supply areas of the genital and genital areas. The perineal nerves run in the direction of the perineum and scrotum in men and to the large labia in women. It also runs to parts of the muscles of the urethra. The inferior rectal nerves, on the other hand, run in the direction of the anus. The dorsal penis nerve and the dorsal clitoral nerve each run to the penis in men and to the clitoridis in women.
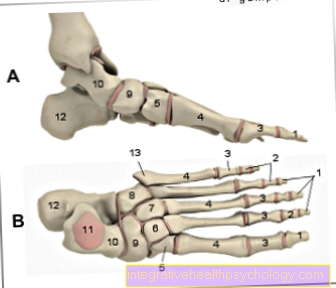
Course of the pudendal nerve
The pudendal nerve arises from the spinal cord at the level of the sacrum. The nerve cords that come from the sacral segments S1 to S3, sometimes also S4, ultimately come together to form the pudendal nerve. The pudendal nerve then migrates into the pelvis, where it passes through a large opening, the infrapiriforme foramen. It then wanders around a protrusion, the ischial spine, and then enters the anterior part of the pelvis through another opening, the lesser sciatic foramen. Once there, it runs through the so-called 'Alcock' canal, whereupon it splits into its end branches. The terminal branches in turn mostly end in regions of the anus, the perineum or the genitals.
function
As a nerve, the task of the pudendal nerve is to connect tissue and muscles with the spinal cord and brain and thereby perceive sensations as well as to be able to carry out movements or muscle tension. The pudendal nerve reaches large areas of the genital and genital areas via its terminal branches. It reaches the entire region of the anus through to the genitals via its sensitive branches, which perceive all pressure and tactile sensations. In terms of motor skills, he is also responsible for the areas located there.
For example, he is responsible for supplying the pelvic floor muscles. The pelvic floor muscles play an important role in ensuring continence in women and men. By tensing and relaxing, it supports the regulation of urination. In addition, it can react to sudden increases in pressure in the abdominal region, which can be caused, for example, by sneezing, coughing or laughing, and thus prevents unintentional urine output.
Another area that the pudendal nerve supplies is the external sphincter muscle of the anus. As with the pelvic floor muscles, it can support and regulate bowel movements by tensing and relaxing.
The genital organs of men and women are supplied by another terminal branch of the pudendal nerve. In men, one of the branches leads directly to the penis, where the ejaculation is controlled. In women, a branch leads to the clitoris, where the woman's sexual arousal is regulated. The pudendal nerve thus also contributes to sexual function.
In addition, due to its generally central location in the pelvic area, the pudendal nerve ensures a stable position for all viscera within the pelvis.
What are neuropathies?
Neuropathies are a disease of the nervous system. However, this is generally not the central nervous system, which includes the brain and spinal cord, but rather the nerves that extend from the spinal cord to the periphery of the body - the peripheral nervous system. Neuropathy damages those peripheral nerves.
As a result of the damage, the nerves can only pass on the information to the brain or the body periphery to a limited extent or not at all. The disease can be very diverse and have different causes. It is often triggered by other diseases, for example by externally invading pathogens. But diseases such as diabetes mellitus or various autoimmune diseases can also trigger neuropathy.
Pudendal nerve neuralgia
Pudendal nerve neuralgia is damage to the pudendal nerve and the associated pain. The damage usually occurs at the largest constriction during the course of the pudendal nerve, the so-called Alcock's canal. This is why pudendal nerve neuralgia is often referred to as 'Alcock' syndrome. Pudendal nerve neuralgia occurs twice as often in women as in men.
Read more on the subject under: Pudendal neuralgia
Symptoms of pudendal neuralgia
Typical symptoms of pudendal nerve neuralgia are lightning-like pain in the perineal region - the area between the anus and genitals. The pain can have different degrees of intensity. As a rule, they gain weight while sitting, as pressure is then exerted on the corresponding area. When standing or while sitting on the toilet, there is pressure relief and thus pain relief.
Very severe injuries to the pudendal nerve can even lead to muscle paralysis and sensory disorders. This can lead to urinary and fecal incontinence, as the nerve injuries mean that the sphincter muscles of the anus and the pelvic floor muscles can no longer be supplied. In addition to supplying the sphincter muscles and the pelvic floor muscles, the pudendal nerve is also responsible for supplying the penis and clitoris. If the nerve is damaged, sexual function and fertility can be restricted.
Cause of pudendal nerve neuralgia
Damage to the pudendal nerve can be caused by mechanical factors, such as pressure on the perineum region when cycling or special positioning during operations. However, damage can also be caused by pelvic injuries, the consequences of childbirth or thrombosis in the pelvic region.
Pudendal nerve neuralgia is usually diagnosed by a urologist or gynecologist, who then refers you to a neurologist.
What if the pudendal nerve is pinched?
If the pudendal nerve is pinched, it can cause severe pain. The pain can then usually be localized in the region between the anus and genitals. They can come on very suddenly and very severely. Patients with a pinched pudendal nerve sometimes even described the feeling as a sharp razor blade.
If the pudendal nerve is pinched, it is irritated by the tissue or muscle that is pressing on it. This stimulation sends pain signals to the brain, which can ultimately lead to a sudden and sometimes very strong pain sensation.
The largest constriction through which the pudendal nerve passes is the pudendal canal, also known as the 'Alcock' canal. The highest risk of entrapment of the nerve is therefore there. The cause of the entrapment can be very simple, everyday movements, such as cycling.
Irritation of the pudendal nerve
The pudendal nerve can be irritated by the layers of tissue surrounding it. If permanent pressure is exerted on a nerve, for example through incorrect posture or overload, this can lead to local nerve irritation, which can possibly spread further.
The irritation of the pudendal nerve is usually very similar to the damage to the nerve. There can be severe pain in the area between the anus and genitals, which can radiate differently. In addition, functions such as urination or bowel movements may be restricted.
However, nerve irritation does not have to occur suddenly, but can also become stronger over time. If a nerve irritation is not treated, it can also turn into an inflammation of the nerves.
What role does the pudendal nerve play in incontinence?
Damage to the pudendal nerve can impair continence. The reason for this is that a terminal nerve branch of the pudendal nerve, the inferior rectal nerve, supplies the pelvic floor muscles. This supports the regulation of urination by tensing and relaxing. If the pudendal nerve is damaged, the pelvic floor muscles cannot function, which in turn leads to incontinence.
What is pudendal nerve syndrome?
Pudendal nerve syndrome is a condition in which the pudendal nerve is damaged or permanently irritated. This is accompanied by sudden, very severe pain in the genital and anus area.
In the area of the pelvis, the pudendal nerve passes through several openings until it finally passes through the so-called 'Alcock' canal. This represents a bottleneck at which entrapment and thus damage or irritation of the pudendal nerve can quickly occur.
If the nerve is damaged, this can lead to restrictions in continence, sexual function and general movement.
Pudendal nerve blockage
The pudendal nerve block, also known as the pudendal block, is used for severe birth pains. A local anesthetic is used to numb the pudendal nerve with the help of a long cannula, which is intended to relieve the pain in the area around the pregnant woman's vagina. When a woman is born, tears in the perineum region, so-called perineal cuts or perineal ruptures, can occur. In order to make this pain as bearable as possible for the woman giving birth, in addition to the natural pain in childbirth, the pudendus block is performed. Local anesthesia of the pudendal nerve has the advantage that the uterine muscles cannot be influenced by it, so that the urge to press and contractions always remain.
As a rule, the operation is only carried out after the cervix is fully opened in the expulsion phase. The local anesthetic usually lasts about an hour. This may even offer time to sew a possible perineal tear.
The goal of the pudendal nerve blockade is pain relief, not complete pain relief. Sometimes the blockage has no effect at all, which is why it is now mostly replaced by peridual anesthesia.