Neurodermatitis
Definition of neurodermatitis
Neurodermatitis is eczema that occurs as a cradle cap in babies and affects the elbows, the hollow of the knees and the neck in later life.
Eczema is an acute or chronic disease of the epidermis (so-called epidermis) with flat skin changes that cannot be clearly distinguished from healthy skin. It is an inflammation.

The reasons
The causes of neurodermatitis have not yet been fully clarified. There seem to be connections between the very complex disease process and the individual course with genetic factors, changes in the body's own defense system and environmental influences. A psychosomatic component also seems to be the cause of atopic dermatitis so far.
Genetic factors seem to ensure that those affected react more strongly to certain influences than others. However, the exact scientific evidence for this theory is currently lacking.
The predisposition is inherited on several genes. The onset and existence of the disease is also dependent on many external (exogenous) factors and internal (endogenous) modulation factors. Exogenous factors are, for example, food allergens, endogenous factors include infections and psychological factors.
A defect in the skin barrier is always at the beginning of atopic dermatitis. The cause for this may be local inflammation or a primary defect in the function of certain skin cells. This cell defect causes more messenger substances to be released that attract inflammatory cells. A complex immunological process is set in motion, which corresponds to an allergic reaction. In addition, the barrier function of the skin is further disturbed, as the body's own defenses cause further skin defects. Another theory about the cause of neurodermatitis suspects a kind of autoimmune disease behind the disease, in which the body's own defense system is directed against its own skin cells.
Another cause could be a colonization of the skin and the mucous membrane by microogranisms. It has been found that the skin and paranasal sinuses of people with neurodermatitis are often overcrowded with bacteria of the type Staphylococcus aureus prevails. These bacteria penetrate the skin through existing skin defects and produce enterotoxins. Enterotoxins are poisonous proteins against which the body's own defense system forms antibodies. In this way, the inflammatory response of neurodermatitis is intensified. Similar intensification reactions are conceivable in fungi such as Pityrosporum ovale or Candida albicans and in various viruses.
The development of the disease
Several disorders play a role in the disease of neurodermatitis.
Allergen contact leads to an inflammatory reaction in which immunoglobulins and messenger substances, so-called cytokines, play a major role. The itching is mainly triggered by the subsequent release of histamine from certain cells.
Biochemical disorders are, for example, the reduced secretion of sebum from the sebum glands of the skin. This results in dry skin with a reduced barrier function. Therefore, there is a loss of water, a reduced protective skin coat with easier penetration of foreign substances and increased itching.
All of these disorders have a certain genetic disposition, so we are given the tendency to neurodermatitis on our genes.
The symptoms
The skin symptoms are usually symmetrical and the dry skin is often accompanied by severe itching, which leads to a desire to scratch in the patient. However, this makes the situation worse by causing weeping eczema. Different symptoms occur depending on the age of the patient.
With neurodermatitis in infancy, weeping and inflammatory eczema foci, especially on the face and head, are typical (“cradle cap”). Spontaneous regression occurs in 50% of babies.
In childhood there is often a coarsening of the field skin (skin of the palms and feet), a deep, weeping abrasion and dry skin. In children, all of these symptoms occur primarily in the hollows of the knees, elbows, skin and ankles, and on the neck. In adolescence and adulthood, chronic coarsening of the field skin with nodules occurs mainly on the face, neck, flexor sides of the arms and legs, as well as on the back of the hands and feet.
Further characteristics of neurodermatitis patients are a double crease in the eyelid (Dennie Morgan fold) and a paradoxical vascular reaction: In contrast to healthy people, patients with neurodermatitis do not develop red, but white traces when scratching (white dermatographism ).
So-called minimal variants of neurodermatitis are also known. For example, it is possible that atopic eczema only occurs on the earlobe, eyelids, and fingertips and toes.
For more information, read on: You can recognize atopic dermatitis by these symptoms
The itching
The itching is in the foreground in neurodermatitis. Although the predilection points, i.e. the place where the rash shows, differ between the different age groups, itching of the skin is always part of it. This can also occur when the skin is only dry and not yet reddened. Sometimes the itching is so severe that the skin is scratched with blood. Especially at night, when those affected can no longer consciously suppress the scratching stimulus, severe scratching attacks often occur, which worsens the skin condition and delays the healing of the skin areas.
In addition, the itching can promote skin infections, as it is easier for bacteria to penetrate scratched skin areas. Treatment of the itch is therefore very important.
The localization
Eczema on the face
The face is particularly affected by eczema in babies. Since neurodermatitis makes the skin more susceptible to allergens, the face is particularly affected in infancy, puberty and adulthood when the facial skin reacts, for example, to cosmetics, other care products or clothing.
Treatment of neurodermatitis on the face is possible. In general, care should be taken to ensure that the skin, which is generally dry in those affected, is cared for daily with moisturizers. Creams that also bind moisture (hydrophilic creams) and creams that reduce water loss from the skin (moisturizing creams) can be used here. When treating neurodermatitis on the face with ointments containing cortisone, special care should be taken, as the skin on the face is already thinner than on the rest of the body and cortisone makes the skin thinner (atrophied). Therefore, only low-effective cortisone ointments containing, for example, hydrocortisone should be used on the face. In order to optimally treat neurodermatitis, it is essential to consult a dermatologist.
You can find more information on this topic at: Atopic dermatitis on the face or These creams can help with atopic dermatitis
Atopic dermatitis of the eyes
Atopic dermatitis of the eyes is particularly typical during puberty, but can also occur at any other age. This leads to reddened lids. The skin is very dry and can also be flaky. Since neurodermatitis is an inflammatory reaction of the skin, the eyelids are often swollen as a result of the skin disease. If no other skin areas are affected, the eye reaction must be differentiated from an allergic reaction. Usually, however, there are other parts of the body, such as the elbows or the back of the hand, that are also affected by neurodermatitis.
The itching, which is also found on the eyelids, is also excruciating. Those affected scratch their skin sore, especially at night. Since the risk of skin infections is greatly increased, treatment should definitely be given. The care of the eyelids is a little more difficult, as it is essential to ensure that the care products do not get into the eyes and do not intensify the skin reaction.
In an acute flare-up of inflammation, the use of creams containing cortisone cannot be avoided. Since the skin on the eye is very sensitive and thin, only weak creams that have been prescribed by the dermatologist should be used.
Atopic dermatitis of the scalp
The scalp is particularly affected in babies. In this case, neurodermatitis is also called cradle cap. There are itchy nodules and blisters. Above all, the skin is dry and flaky. Later on, other parts of the body are typically affected. In rare cases, however, the scalp can also be affected during puberty or adulthood. This also leads to severe itching and red, dry skin.
Atopic dermatitis on the head is mainly triggered when the sensitive skin reacts to, for example, shampoos, hair coloring products or the fabric of a hat. Washing your hair too often can also dry out the scalp and provoke neurodermatitis. The triggers should definitely be avoided to contain further flare-ups.
All in all, rashes and flaky skin on the head are signs of another skin disease: psoriasis. In order for the correct diagnosis to be made, a dermatologist should be seen if rashes and dry skin appear on the scalp. In principle, shampoos should be used that do not irritate the scalp, i.e. that do not contain any fragrances or preservatives. In addition, shampoos should be used that donate moisture to the scalp. Products that contain urea, which also binds water, have proven to be effective.
Also read the article: Atopic dermatitis of the scalp.
Atopic dermatitis on the hand
Neurodermatitis often occurs on the back of the hand and on the fingers. This is particularly noticeable when it gets cold outside and the already dry skin dries out even further. It is therefore important to ensure adequate moisture care, especially in the winter months. In addition, certain professional groups are particularly affected by neurodermatitis on the hands. These are mainly professions that deal with skin-irritating substances.
These include, for example, hairdressers, where frequent contact with water, shampoos and hair dye can irritate the hands. The spaces between the fingers are often severely affected. The rash can then also appear on the palms of the hands. Nursing and healing professions, in which disinfectants are used, are more often affected by neurodermatitis on the hands.
Atopic dermatitis on the hands is also a red, itchy rash. Scratching can make the skin sore and wet. Therapy during acute inflammation is mainly possible with cortisone creams. Since a change of occupation is often not simply possible or not wanted, if you have mild neurodermatitis you can try to wear gloves when working with substances that irritate the skin - such as in the hairdressing profession. However, care should be taken to put cotton gloves under the gloves, which are often made of latex or nitrile, as the material can also trigger a skin reaction.
Find out more about the topic here:
- Atopic dermatitis of the hand.
- Neurodermatitis on the finger and fingernails
Neurodermatitis in the crook of the elbow
The crook of the elbow is a special predilection point (point where neurodermatitis occurs particularly frequently) in neurodermatitis. Skin rashes are particularly common in childhood, puberty and adulthood. The rash is red, interspersed with small nodules, and is usually very itchy. The itching can become worse, especially if there is heat or sweat in the crook of the elbows.
To prevent atopic dermatitis, care should be taken that no scratchy clothing is worn. In acute attacks, it is usually only possible to contain the inflammation with the help of a cortisone cream.Since atopic dermatitis is provoked by dry skin, you should also avoid showering several times a day. After showering, the skin needs to be cared for with moisturizing lotions that are suitable for sensitive and allergy-prone skin. Lotions that contain urea, which also binds water, are particularly suitable for this. If the itching is particularly severe, creams that contain polidocanol can be used. These numb the skin superficially and take away the itching. Cotton gloves can be worn at night to prevent the skin from being scratched open with the sharp nails and thus not increasing the inflammation or delaying healing.
Are you interested in this topic? For detailed information, see: Neurodermatitis in the crook of the arm
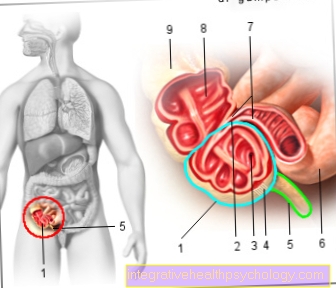
Neurodermatitis in the genital area
Atopic dermatitis in the genital area is not common. This is mainly due to the skin's reaction to allergens, such as the wrong shower gel. Shaving the pubic hair can also provoke the onset of neurodermatitis.
Since the use of cortisone creams in the genital area is to be enjoyed with particular caution, it is essential to consult a dermatologist. Cortisone passes into the body very easily in this area and can therefore cause particularly severe side effects.
Atopic dermatitis in babies
Atopic dermatitis often appears for the first time between the third and sixth month of life. 60% of diseases manifest themselves within the first year of life. In babies, neurodermatitis begins as a so-called cradle cap. The name comes from the fact that the skin resembles burnt milk. Itchy nodules, blisters, crusts and scales appear.
The rash is mostly found on the face, head, and the extensor sides of the arms and legs. This is in particular contrast to the older patients, in whom the flexors of the arms and legs are particularly affected. Other areas of skin on the trunk are sometimes also affected. In babies, the diaper region is usually not affected by the rash.
The baby's skin should definitely be treated as there is an increased risk of bacterial skin diseases on the affected skin areas. To prevent eczema in babies, babies should be breastfed for four to six months. Feeding the baby with hypoallergenic infant formula is also recommended.
Find out all about the topic: Atopic dermatitis in babies.
The diagnosis
There are several different criteria for diagnosis. The main symptoms, i.e. the most important and most common symptoms, are dry skin and severe itching.
The main criteria include:
- itching
- dry skin
- Typical appearance (eczema, coarsening of the field skin, nodules)
- Typical location (child: face, outer sides of arms and legs; adolescent: bending elbows, knees)
- Occurrence of atopic dermatitis in the family or already in the patient himself
- Chronic and / or repeated course
The anamnesis (medical history), i.e. the questioning of the patient about his health, his environment, etc., should also be taken conscientiously. There can be many indications of the formation here.
Blood tests are done for the amount of immunoglobulins, especially the IgE type. However, IgE can also be increased in allergies. So an increase does not provide any proof of the existence of neurodermatitis.
The treatment
The therapy of an atopic dermatitis disease is adapted to the course of the disease and the severity of the symptoms. As a guide, you can stick to a level scheme, which must be adapted individually.
The first stage of the therapy is applied to dry skin and consists of basic skin care that stabilizes the skin's barrier function and is intended to make the skin less sensitive to irritation and allergens. In addition, provocation factors that aggravate atopic dermatitis should be avoided as far as possible.
If mild eczema occurs, external active ingredients can also be used as a second stage of therapy. Frequently used ointment additives are, for example, evening primrose oil, St. John's wort extract, dexpanthenol or zinc. Antiseptic agents can also provide relief from atopic dermatitis, especially if there is an excessive colonization of the skin with bacteria or fungi. Since neurodermatitis is often accompanied by severe itching, the second treatment stage also includes treating the itching, which can be done, for example, with tannin preparations. So-called antihistamines can also relieve itching.
If more pronounced inflammatory symptoms occur, ointments with anti-inflammatory active ingredients are used, but most often with the active ingredient group of glucocorticoids (cortisone). The glucocorticoids act against itching and inflammation of the skin and relieve severe relapses of neurodermatitis. Different active substances are used depending on the type and severity of the symptoms. For the second stage of neurodermatitis therapy, weakly or moderately effective glucocorticoid preparations are sufficient.
In the case of severe attacks, strong glucocorticoids can also be applied externally in the third stage when moderate eczema occurs. Irradiation with high-dose UV light can have an anti-inflammatory effect on the affected areas of the skin and allow temporary healing.
Long-lasting or severe eczema require systemic therapy in addition to the treatment options already mentioned (stage 4). In these cases, internal use of cortisone can be considered. The most severe forms of neurodermatitis are left with the drug Cyclosporin A. Cyclosporin A often causes atopic eczema to regress quickly, but it also has serious undesirable side effects, which is why it is not generally recommended. Cyclosporine A can, for example, lead to increased blood pressure, kidney damage or gum growth and promote the occurrence of malignant tumors.
Read more on this topic:
- Treatment of neurodermatitis
- photodynamic therapy
Cortisone
Cortisone is used in atopic dermatitis primarily in the acute inflammatory phase. Above all, the cortisone is applied directly to the skin using a cream. It soothes the inflammation and also helps against the itching. The itching usually disappears within a few hours, the redness usually disappears within a few days.
Because cortisone makes the skin thinner, which is also known as atrophy of the skin, it should not be used too often. Wound healing disorders can also occur as cortisone reduces the immune system. In the case of severe skin involvement, cortisone therapy in tablet form is also possible. However, this can lead to severe side effects such as high blood pressure, water retention or osteoporosis. It should therefore only be used in consultation with a doctor.
Find out all about the topic here: Cortisone in atopic dermatitis.
Different creams
Neurodermatitis is associated with very dry skin. It makes sense to treat this dry skin with a gentle skin care cream. Ointments, creams and lotions that have a high percentage of fat and moisture can be used for this. This daily basic care should be used regularly so that the barrier function of the skin can be stabilized. In addition, skin care should reduce the skin's sensitivity to allergens and irritations.
The composition of the eczema creams depends on the current condition of the skin. As a rule, oil-in-water emulsions are used, but water-in-oil emulsions can also be used for very dry skin. E.
Since skin affected by neurodermatitis has a very low concentration of urea, creams containing urea can help to reduce the characteristic dryness of the skin. However, the application of urea to the skin of irritated or cracked skin can lead to further irritation or painful burning sensation when applied.
Many other additives in creams against neurodermatitis are supposed to improve the moisture retention or the healing process of the skin. Specific active ingredients such as evening primrose oil, St. John's wort extract, zinc or dexpanthenol are added to the creams to care for the skin. The Multilind® healing ointment, which contains tin oxide as an active ingredient, can be used, for example, as a care product for neurodermatitis.
A cream against neurodermatitis can also contain antiseptic agents. If the skin is overly colonized with bacteria or fungi, for example triclosan, chlorhexidine or antibiotics can be used externally. Additional treatment with dilute chlorine bleach (sodium hypochlorite solution) can also reduce the skin condition if the bacterium is colonized Staphylococcus aureus improve.
If the rash becomes wet, tannic creams are available. These have a drying, antipruritic and mild anti-inflammatory effect. Stronger flare-ups of atopic dermatitis are treated with creams that contain immunosuppressants, usually cortisone. Creams containing cortisone can be used in different concentrations and ointment bases. Hydrocortisone creams are often sufficient for milder symptoms or on the face. Since cortisone has many side effects, the indication for the use of creams containing cortisone should be made individually by a specialist.
Find out all about the topic here: These creams can help with eczema or Skin care for atopic dermatitis
Home remedies
There are many different home remedies that can be used for atopic dermatitis. Since not all home remedies have the same effect on everyone, those affected have to test individually what helps and what does not. On the one hand, home remedies are used to increase the moisture in the skin. On the other hand, home remedies can be used against the inflammation and itching in an acute attack in order to delay the use of cortisone.
Aloe vera gel can relieve itching, for example, thanks to its cooling and soothing effects. Apple cider vinegar diluted with water (ratio 9: 1) can also be applied to the skin. Apple cider vinegar has anti-inflammatory effects and can also help relieve redness and itching. Yoghurt or quark applied to the skin have a cooling and therefore itching effect. The yoghurt or quark is simply washed off after it has dried out. St. John's wort oil can also soothe skin affected by neurodermatitis.
Hyaluronic acid gel can be applied to provide the dry areas of skin with more moisture. Coconut oil is also a home remedy that can reduce the symptoms of an acute rash. It also provides moisture. However, the oil should not be applied directly to the skin, but mixed with a skin-friendly base cream beforehand (ratio of base cream to coconut oil 9: 1). If this mixture is kept in the refrigerator, it can also reduce itching in the case of acute inflammation thanks to its cooling effect.
Read more about the topic here: Home remedies for atopic dermatitis.
What role does the psyche play in neurodermatitis?
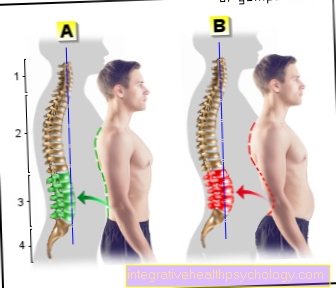
Atopic dermatitis is not a neurological or mental illness. However, emotional stress can provoke the onset of neurodermatitis. These include stress, anger, grief or nervousness. Many people affected also report that atopic dermatitis gets worse when they are not feeling well.
However, since those affected often suffer from the noticeable symptoms - especially if the rash occurs on the face - it is often a vicious circle, as this emotional stress can worsen atopic dermatitis. One should also take the suffering of neurodermatitis sufferers seriously, as this can result in further psychological stress and withdrawal from social life.
What is an eczema flare-up?
A flare-up is the length of time that symptoms of a chronic illness appear. The symptoms can worsen or show on previously healthy skin. In atopic dermatitis, certain triggers are often involved in the outbreak of the attack.
The thrust can - with the right treatment - be contained again. How long an attack lasts also depends on the treatment of the affected skin.
What are the triggers for a surge?
The triggers for a flare-up in atopic dermatitis are very diverse and sometimes very unspecific. For example, exposure to dust can provoke the rash in a very short time. Heat build-up, for example during sports, when the skin becomes too warm and starts to sweat, can trigger atopic dermatitis. In the winter months, the skin dries out from cold weather. Since the skin of neurodermatitis sufferers is already dry, the additional dehydration of the skin causes the rash to break out.
Emotional stress such as stress or grief can also cause a surge. Sometimes the symptoms worsen even with infections. Skin irritations, for example from skin-irritating substances such as creams or scratchy clothing, can also lead to a rash.
Many other stimuli can lead to the onset of neurodermatitis, so it should be found out individually what aggravates the neurodermatitis and these factors should be avoided.
Is eczema contagious?
Atopic dermatitis is not contagious. The cause of neurodermatitis has not yet been clarified, but a genetic predisposition is suspected. This means that firstly, atopic dermatitis is hereditary and other skin diseases can often be found within the family. A predisposition to the increased formation of antibodies that are involved in inflammatory reactions and allergies is inherited: the so-called IgE antibodies.
Furthermore, it is suspected that those affected have a barrier disorder of the skin, in which water escapes from the inside to the outside, so that the skin dries out and becomes more susceptible to environmental influences.
Can you cure neurodermatitis?
Neurodermatitis is a chronic disease that cannot be cured. If the first symptoms occur in infancy, the symptoms can be expected to decrease during puberty and adulthood. Only in a few cases does neurodermatitis become severe in adulthood. Spontaneous regression is possible at any time, i.e. possible in every age group.
Read more on this topic: Can you cure neurodermatitis?















-de-quervain.jpg)