Vaginal inflammation
definition
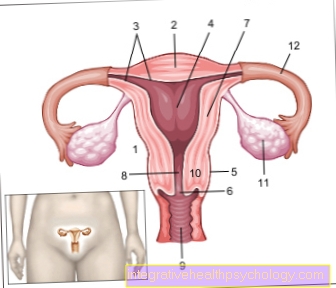
Vaginal inflammation, also called vaginitis or colpitis, is the inflammation of the lining of the vagina. If the labia are also affected, one speaks of vulvovaginitis. This inflammation is particularly often caused by bacteria or fungal infections (see also: Vaginal fungus).
Many women suffer from vaginal inflammation in the course of their lives and this has nothing to do with poor hygiene, as is unfortunately often wrongly assumed. In the following text you will find out how vaginal inflammation develops and how it can be treated successfully.

causes
The vagina naturally has its own protective barrier, which is formed by the so-called vaginal flora. This refers to a number of microorganisms that prevent other harmful microorganisms such as bacteria or fungi from settling.
In addition, the vagina has an acidic pH value, which can also ward off potential intruders. If this natural protective barrier is disrupted, pathogens can more easily colonize the mucous membrane and thus lead to inflammation.
There are a number of factors that can imbalance the natural vaginal flora. Vaginal inflammation after taking antibiotics is typical, for example. Antibiotics destroy bacterial pathogens - but unfortunately not only these.
Our natural bacterial colonization (so-called microbiome) can also suffer from the effects of the drug - this leads to diarrhea in the intestine, for example. In the vagina, important bacteria that are responsible for the protective barrier can be killed - the result is the colonization of new bacteria, which can then lead to vaginal inflammation.
Excessive hygiene, for example with alkaline soaps in the genital area, has a similar effect. Here, too, the natural vaginal flora is broken and incorrect colonization can lead to vaginal inflammation.
The hormone estrogen also has an important influence on the vaginal flora. If there is a lack of estrogen, such as is the case during menopause, the vagina is more prone to inflammation. Mechanical irritation can also disturb the vaginal flora. This includes, for example, contraception with a vaginal diaphragm or the use of tampons.
Finally, it should be mentioned that even very heavy menstrual periods can raise the pH value and thus reduce the barrier function.
Senile colpitis is acute vaginal inflammation after menopause. Find out more at:
Senile colpitis - what you can do about it
bacteria
The most common cause of a vaginal infection is a bacterial infection. This is preceded by what is known as bacterial vaginosis, which means that the natural vaginal flora has been disturbed and there is an incorrect colonization with other bacteria, which can then trigger inflammation.
These are often bacteria that occur in many places and are also naturally part of our bacterial flora. These include, for example, the E. Coli germ, which is found in our intestines, among other things. Other typical germs are staphylococci, streptococci and enterobacteria.
As already explained above, a lack of hygiene does not play a leading role in infection with one of these germs, but rather the disruption of the natural vaginal flora. Even bacteria associated with classic sex diseases such as gonorrhea (gonorrhea, the pathogen is called Neisseria gonorroeae) or chlamydial infection can cause vaginal infection. The typical mode of transmission here is unprotected sexual intercourse - you can protect yourself by using condoms.
Mushrooms
Vaginal inflammation can also result from the incorrect colonization of fungi and is then also referred to as vaginal mycosis. Here, too, the disturbance of the vaginal flora typically precedes it. The pioneer among the fungi for vaginal inflammation is the yeast fungus Candida albicans (see also: Candidiasis), which makes up over 80% of fungal infections of the vagina.
Like other possible fungi, this fungus occurs naturally on our skin and intestinal flora.
diagnosis
So that the gynecologist or family doctor can make the correct diagnosis, he will first be asked a brief survey (anamnese) in order to determine and assess the onset, symptoms and course. The next step is the examination of the vagina, here the condition of the mucous membrane (redness, vesicles, deposits) and possibly also the discharge (color, smell, consistency) can provide clues about the possible pathogen.
The pathogen can be secured by taking a smear with pathogen determination on site under the microscope or in a microbiological laboratory. In addition to diagnosing the current vaginal inflammation, it is also important to identify the cause of it. Has an antibiotic or other medication been taken?
Have your living conditions or diet changed? What is the current genital hygiene like? These and similar questions, possibly with subsequent examinations, can prevent a recurrence of vaginal inflammation.
Concomitant symptoms
Vaginal inflammation is characterized by typical symptoms that vary depending on the pathogen. The main symptom of vaginal inflammation is usually the increased and changed discharge from the vagina. The so-called Vaginal fluoro can be very different: from whitish to bloody, from liquid to dry and crumbly and from low-odor to intensely smelling - what they have in common is that it increases.
Read more about this under: Discharge from the vagina
Other possible symptoms are severe itching in the vaginal and anal region, burning pain that can also be noticed during sexual intercourse, bleeding, painful urination or the formation of blisters. Not every vaginal inflammation is strongly symptomatic, but you should not be afraid to visit your gynecologist, even with small changes in the discharge or itching, so that the incipient infection and its cause can be treated promptly.
discharge
The main symptom of a vaginal inflammation is a change in the natural discharge of the vagina. Most women report a significant increase in fluorine, which, however, can vary greatly in color, consistency and smell. In bacterial infections, for example, a green-yellowish, unpleasant smelling (often fishy smell) fluorine is typical.
A vaginal infection triggered by the yeast Candida albicans usually leads to a rather low-odor, whitish, rather dry fluorine. If you notice a change in your discharge, it is worth a visit to your gynecologist, as he can point to an incorrect colonization of the natural flora or to a vaginal inflammation.
treatment
Vaginal infection is treated depending on its cause. If there is a bacterial infection, antibiotics are used that specifically attack the germ. Depending on the type of infection, these can be administered locally as an ointment or suppository, sometimes injections or tablets are also necessary.
In the case of fungal infections, what are known as antimycotics are used, a class of substances that is specifically directed against fungi. Here, too, the possible applications range from local ointments to systemic tablets. Alternatively, local therapy with antiseptic agents can be used in some cases. These have a similar effect to the well-known hand disinfection and can thus fight fungi, bacteria and microorganisms.
It should be noted that many of the pathogens causing vaginal inflammation can also be sexually transmitted - so treating your partner as well is often beneficial in order to avoid re-infection. After therapy is over, the cause of the vaginal infection should also be treated.
For example, there are bacterial and fungal cultures that can promote the rebalancing of the vaginal flora. Estrogens can also be administered if a hormone deficiency is found.
By antibiotics / after antibiotics?
Many diseases are caused by bacteria - and nowadays they can usually be treated with antibiotics. Antibiotics are aimed specifically at bacteria and destroy them - but there is often "collateral damage". Our body works in close cooperation with many bacteria that help us to fight off harmful germs or to break down our food.
There is even the assumption that some intestinal germs support our immune system. Unfortunately, many antibiotics act not only on the disease-causing bacteria but also on those that work with our body. The vagina is also colonized with helpful bacteria, which, among other things, offer protection against incorrect colonization by other germs.
This is a very sensitive balance between different pathogens and can be unbalanced by taking antibiotics. If one type of bacteria is significantly reduced in the vaginal flora by taking medication, the other germs can now grow more or foreign germs can gain a foothold.
This can then lead to a vaginal infection. It must be emphasized, however, that not every antibiotic intake has to result in a vaginal infection. In addition to the type and dosage of the antibiotic, the duration of intake is also decisive. However, if you notice one of the above symptoms after taking an antibiotic, don't be afraid to see your gynecologist.
Which home remedies can help?
If you have a vaginal infection, home remedies can aid healing. It should be noted that if the symptoms persist without improvement, a doctor should be consulted in any case!
A common home remedy for vaginal infection is to flush the vagina. Various means are available for this: Lavender or tea tree oil are often used, as they can have a disinfecting effect. Before using it over a large area, however, the tolerance should be checked on a smaller area of the skin, as many people are overly sensitive and skin rashes can develop.
You might also be interested in the following topic: Eczema in the genital area
Rinsing with vinegar or lemon solutions is often recommended, but you should refrain from doing this, as these can further damage the already irritated mucous membrane - in the worst case, the pathogens can penetrate even further.
Many patients also swear by the healing properties of aloe vera creams and gels, which should be applied to the inflamed mucous membrane several times a day. It is also recommended to use a tampon soaked in yoghurt to support the natural vaginal flora with the lactic acid bacteria contained in the yoghurt.
It should be noted that the home remedies mentioned above will often fail in the case of severe vaginal inflammation, as neither lactic acid bacteria nor tea tree oil can prevail against the pathogens present. In any case, a doctor's visit is advisable. Conservative drug therapy can be supported with home remedies if necessary.
homeopathy
Homeopathic remedies can also be used to support conservative therapy for vaginal thrush. It should be noted that there is no proven scientific effect with homeopathic remedies and they should not be used as the sole therapy! In the case of severe itching and discharge, Sitz baths with oak bark, witch hazel or black tea are recommended.
With the same symptoms, sodium muriaticum 15C or Kreosotum 15C can also be used. Belladonna D12 is also referred for a rather dry vagina with hot, pulsating pain. Other possible globule preparations are Lilium tigrinum D12, Borax D12 or Pulsatilla D12. Each preparation is specific for a symptom constellation, which can be understood in the relevant literature.
Duration
The duration of a vaginal inflammation depends on the causative agent and the severity of the disease. If the vaginal inflammation is recognized early and consistently treated, a clear improvement should be noticeable after a few days.
It is important to note that prescribed ointments and rinses should be used for a few days after the symptoms have ended to prevent relapse. If antibiotic therapy is prescribed, it is important that the antibiotic is taken as directed by a doctor and that it is not discontinued on its own after the symptoms have improved.
Again, relapse can occur! If the symptoms do not improve in a timely manner, it is advisable to visit the doctor again and, if necessary, to increase or change the therapy. During this process, the doctor will, for example, carry out a precise determination of the pathogen and see whether the germ is resistant to a particular therapy.
With girls / with babies
Vaginal infections can also develop in young children and girls. One of the reasons for this is the lack of the sex hormone estrogen, since the girls are not yet through puberty. The changed flow of urine through the intact hymen can also promote the development of vaginal inflammation.
It is important to teach your children about proper vaginal hygiene at an early age. In the case of recurrent vaginal or bladder infections, it can help if the girl goes into the "skier's position" when going to the toilet, that is, does not completely lower her buttocks and tilt her upper body slightly forward. This favors the outflow of urine along the hymen.
In the case of small children, however, it should be noted that the diapers are not too tight and airtight, as a moist environment promotes bacterial growth. If you notice a sour, fishy odor or discharge on your child, do not be afraid to see your pediatrician.
You might also be interested in this article: Lack of estrogen
During pregnancy
Vaginal infections can also occur during pregnancy. This is favored by the changing hormonal influence on the natural vaginal flora. The women often suffer from vaginal thrush, the ones mentioned above Candida albicanswhich can usually be easily treated with antifungal ointments.
It is important to note that some vaginal inflammation pathogens can also be harmful to the unborn child! This includes, for example, infection with chlamydia, which can lead to premature labor or even miscarriages. It is therefore very important that the pregnant woman consults her gynecologist as soon as possible if the above symptoms occur so that the infection can be treated quickly and efficiently.
How contagious is that?
Vaginal infections are not always contagious. Many of the pathogens occur naturally on our skin and mucous membranes and can only grow more frequently if the protective vaginal layer is disrupted.
However, infection can also occur if the toilet paper is brushed from the buttocks to the vagina when using the toilet. This way, intestinal bacteria can get to the vaginal mucosa. Therefore the opposite direction - i.e. from vaginal to anal - is recommended when using toilet paper.
However, there are also some pathogens that are exchanged as sexually transmitted diseases via unprotected sexual intercourse, including chlamydia, gonococci, herpes viruses or trichomonads. Treatment of the partner is essential here in order to avoid re-infection.