Impingement syndrome surgery
introduction
In the case of shoulder impingement syndrome, there is a narrowing of the space between the roof of the shoulder and the head of the humerus. Due to this tightness, the structures and soft tissues running in this space, such as tendons, muscles or bursa, are pinched, which leads to severe pain and significant movement restrictions in the shoulder joint.
The terms shoulder tightness syndrome or shoulder-arm syndrome are also used synonymously for the disease.
In the field of hip joint surgery, the term impingement syndrome also occurs, whereby it concerns a narrowing of the space between the socket of the hip joint and the head or the neck of the thigh bone.

When do i need an operation?
In the early stages of the disease, it is often sufficient to take care of the affected shoulder, avoid overhead work and avoid lifting heavy objects. At the same time, with the help of conservative treatment methods in the form of pain relievers and anti-inflammatory drugs (ointments, syringes or tablets), physiotherapy, cold therapy and electrotherapy as well as targeted muscle training, symptoms can be improved.
An operation is necessary if the pain and restricted mobility in the arm and shoulder persist or increase for several months despite conservative therapy. Due to the lack of relief for the constricted structures and soft tissues, further damage and inflammation occur in the shoulder joint area. In the worst case, muscles or tendons of the shoulder-stabilizing muscle group (rotator cuff) can tear and thus make an operation urgently necessary.
Further information on this topic:
- Therapy of impingement syndrome
- Physiotherapy for an impingement syndrome
Operative therapy
General
The attending physician differentiates between stage I and II of the disease, in which after about half a year to a year of conservative forms of therapy, the treatment must be classified as unsuccessful and there is a lesion of the tendon caused by the so-called acromionic spur, and stage III, the stage the incomplete rupture.
The surgical procedure in a subacromial bottleneck syndrome, as the impingement syndrome is also called, it is called subacromial decompression (decompression = expansion).
With regard to this decompression there are - depending on the underlying cause - different approaches for an operation. The aim is to eliminate constrictions in the shoulder joint so that tendon material or soft tissue is no longer pinched.
A distinction is made in the operational area between:
- Acromioplasty according to Neer (= Défilé - extension)
In principle, it is understood to mean the expansion of the subacromial space by decompression of the supraspinatus tendon. The aim is to create more space for movement of the soft tissues below the shoulder roof. To achieve this, a small portion of bone is removed from the lower part of the acromion. Acromioplasty can possibly be performed arthroscopically. Acromioplasty can be used for both a rotator cuff lesion and an intact rotator cuff. You will find more detailed explanations of this procedure below. - A corrective operation that may be necessary after a broken bone on the head of the humerus that has healed.
- Surgical removal of calcified foci on the rotator cuff (tendinitis calcarea). A thickened and inflamed bursa that is on the rotator cuff is partially or completely removed. This is usually done in conjunction with an acromioplasty (see above).
Appointment with a shoulder specialist

I would be happy to advise you!
Who am I?
My name is Carmen Heinz. I am a specialist in orthopedics and trauma surgery in the specialist team of .
The shoulder joint is one of the most complicated joints in the human body.
The treatment of the shoulder (rotator cuff, impingement syndrome, calcified shoulder (tendinosis calcarea, biceps tendon, etc.) therefore requires a lot of experience.
I treat a wide variety of shoulder diseases in a conservative way.
The aim of any therapy is treatment with full recovery without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
You can find more information about myself at Carmen Heinz.
Subacromial decompression
Subacromial decompression is specifically discussed below.
The roof of the shoulder consists of two parts, the posterior bony part, called the acromion, and the anterior ligament part, the coraco-acromial ligament. The tendons and soft tissue of the rotator cuff are located in the subacromial space, which forms a tunnel-like space in the shoulder joint. This "tunnel" is with one subacromial bottleneck syndrome too narrow and needs to be expanded.
The distance between the humeral head and the lower surface of the acromion is medically known as the acromio-humeral distance. Normally, a minimum distance of 10 mm must be guaranteed. This space can be enlarged by removing the downwardly directed "bone nose" on the acromion.
While in the past the anterior part of the shoulder roof was usually removed, it is now usually done without. If the so-called "abutment", the front part of the ligament, is completely missing, the head of the humerus can slide upwards.
The surgical procedure can be carried out using both arthroscopic (arthroscopic subacromial decompression, also known as ASD) and open technology (OSD = open subacromial decompression).
Arthroscopic subacromial decompression - ASD - takes place as part of the mirroring of the shoulder joint that is carried out at the same time. As a rule, you only need 2-3 small skin incisions about 1 cm in length, into which special instruments are inserted. The surgeon can insert a camera into the joint, with the help of which he can directly identify and remove bony structures that lead to constrictions. Using a shaver, a special rotating set of instruments, part of the undersurface of the acromion is milled off.
In the case of more pronounced clinical pictures, open therapy is usually preferable. Here larger bone spurs can be removed and any adhesions that may be present can be removed at the same time. If necessary, the surgeon can also remove parts of the joint (bone parts, tendons or parts of bursa) and / or smooth joint surfaces. The open subacromial decompression - OSD - takes place through a skin incision of approx. 5 cm. Due to the higher stress on the patient, this procedure is associated with a longer hospital stay.
If it is possible to differentiate between the two types of surgery, the ASD is usually preferable to the OSD. The main advantage of the ASD is that it is less invasive. With this variant, the procedure can usually be carried out on an outpatient basis, i.e. the patient can leave the hospital on the day of the operation.
After each type of operation, extensive physiotherapy is prescribed, whereby it is important to find a good balance between overstressing the joint too early and immobilizing it too long, both of which can have a long-term negative effect on the healing process. The larger the operation, the slower the mobilization of the joint should be started and the longer it usually takes until the affected shoulder can regain completely normal mobility and freedom from pain.
You can find more detailed information in the chapter: Subacromial decompression
X-ray of an impingement syndrome before surgery

Spur before surgery
Image of a special x-ray image (outlet view), in which a constricting spur can be seen under the shoulder roof.
X-ray image of the shoulder after removal of the spur

After surgery
The same X-ray after the arthroscopic operation after the spur was removed.
Do i need general anesthesia?
If a surgical procedure is necessary, this is usually carried out using general anesthesia. In the meantime, the patient is placed in a sitting position ("beach chair position") and is not aware of the operation.
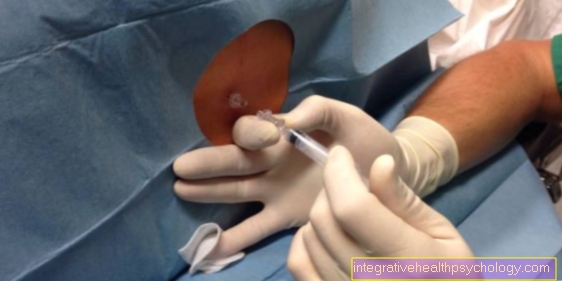
Consciousness and pain sensation are completely switched off with this anesthetic method and the patient cannot be addressed during the procedure. In rare cases, local or regional anesthesia (scalene block or plexus anesthesia) can be used. Here, nerve fiber bundles in the neck and armpit area are injected with an anesthetic. The patient is conscious and can be addressed at any time. This form of anesthesia is usually used in combination with general anesthesia or to temporarily eliminate pain.
General information on general anesthesia can be found here: General anesthesia - procedure, risks and side effects
Duration of the operation
The surgery usually takes 30-45 minutes.
In the case of open interventions and complex preparation of the shoulder joint, for example in the case of pronounced adhesions in the joint, the operation time can increase to up to several hours. The procedure is performed under general anesthesia. At least one day should be planned for the treatment as a whole, as the anesthesia is usually followed by an observation period. In the case of inpatient admission, you should expect 2-4 days.
How painful is such an operation?
If the operation is performed under general anesthesia, the patient does not feel any pain during this time and is also unconscious.
In the first time after the procedure, pain reliever medication enables the shoulder to move almost painlessly. Early movement is very important to prevent sticking or renewed, space-consuming adhesions. After a few days, the pain should have subsided to such an extent that pain medication can be dispensed with.
You may also be interested in this topic: Exercises against muscle shortening in impingement syndrome
Hospitalization
The operation for an impingement syndrome can be performed in an inpatient or outpatient setting.
An outpatient operation is only planned with a hospital stay for the day of the operation, the hospital can be left on the same day. Should complications arise, a stay beyond the day can be recommended. Outpatient treatment should only be considered if someone is available to support day-to-day activities after discharge and there is some mobility to come to the hospital for follow-up examinations or later complications.
Inpatient surgery is usually planned for 2 nights with this treatment.
Also read our topic: Tendon affection in an impingement syndrome
Risks of the operation
An operation in general always involves certain risks.
General anesthesia is not survived equally well by all people and complications can certainly arise during this. However, these are not specific, but apply to every surgical procedure and are discussed with the doctor before the operation begins.
The surgical wounds may become infected after the operation. Since only small incisions are made during the operation for the impingement syndrome, the risk of developing an infection is classified as low.
A risk that cannot be neglected is that despite the operation, the tendon damage will persist and crack formation will occur. Likewise, despite the operation, a new impingement syndrome can occur, among other things due to a thickened bursa or other inflammatory thickened structures in the shoulder area.
After operations, the increased risk of thrombosis should be taken into account when immobilizing the patient, but this can be prevented with medication if the patient is immobilized for a longer period of time.
Read more on the subject at:
- Postoperative thrombosis prophylaxis
- Post-operative complications
Advantages and disadvantages of the operation
Shoulder impingement syndrome should initially be treated with pain medication, muscle relaxation, immobilization, and anti-inflammatory measures before surgical therapy is considered.
If the symptoms persist under this treatment, or if imaging tests have diagnosed a protruding bone or a torn tendon, surgery is a treatment option to widen the joint space to relieve symptoms or to reconstruct the tendon.
One advantage of the enlargement is that symptoms do not recur immediately after renewed exposure (a renewed impingement syndrome cannot, however, be ruled out), as there is enough space in the joint space and restricting structures have been removed. This is not the case with pain reliever / anti-inflammatory therapy after improvement. This can quickly lead to recurring pain.
Nevertheless, an operative measure always carries a certain risk and the therapy is much more complex than taking medication. Surgical treatment is recommended if other approaches do not offer permanent freedom from symptoms and recurring symptoms occur despite conservative therapy.
You might also be interested in this topic: Physical therapy for impingement syndrome
Aftercare
After the operation, the arm should initially be held still. A sling bandage is usually suitable for this, in which the forearm is supported and the shoulder is thus immobilized. This should not be used for longer than 3 days and light movement in the shoulder joint is usually recommended as early as the day after the operation.
In the case of inpatient treatment, movement exercises are carried out with the help of physiotherapists, which allow the joint to be mobilized at an early stage. This is to prevent adhesions and also reduces the risk of thrombosis. For the following 2-3 weeks, the focus should be on regular physiotherapeutic treatment, which can be accompanied by pain-relieving and anti-inflammatory drugs (NSAIDs). This is followed by rehabilitation measures that serve to strengthen the shoulder muscles and thus ensure correct joint guidance.
The physiotherapeutic follow-up treatment includes, on the one hand, so-called passive movements, which the physiotherapist performs in the lead, and on the other - after a certain lead time - active movements that the patient performs himself under physiotherapeutic guidance.
In addition, there is the possibility of post-treatment with the help of a motor movement rail (= CMP). While the patient is sitting in a chair, the shoulder is placed on an electrically powered movement rail and a pain-free movement of the shoulder is initiated. As a rule, patients find treatment with CMP pleasant. The movement rail can be adjusted continuously and according to your individual scale.
Cooling measures (cryotherapy measures) are taken immediately after the operation to reduce the pain and, above all, to reduce the swelling of the soft tissue. In addition, pain relievers and decongestants can be prescribed individually as required.
How long does the entire healing take?
After the operation, extensive physiotherapeutic follow-up treatment and possibly rehab is necessary.
If the healing process is good, the patient can already carry out light, everyday activities after a few days (e.g. lifting a cup). Several weeks to several months can pass before the mobility of the shoulder joint is completely restored. On the one hand, the professional and private situation of the patient plays an important role, on the other hand, it also depends on how severely the shoulder was damaged before the operation.
If you want to go back to sport, you should strive for a conscientious rehab, as the injury or illness is often accompanied by a loss of strength and coordination of the muscles involved. Particular caution is required when driving a car, as there must be good mobility of the shoulder without pain. The attending physician will decide together with the patient when he can carry out which activities again.