Risks of a colonoscopy
definition

The colonoscopy is also called colonoscopy in technical terms. This is an examination of the intestine using a long endoscope to which a camera is attached to examine the tissue. It is one of the most important examinations for the early detection of colorectal cancer and can be carried out by specialists in medical practices or on an outpatient basis in hospitals.
The colonoscopy procedure
The colonoscopy is done by a Gastroenterologists carried out. In order to have a good view of the inside of the intestine, the patient must have one the day before the operation thorough colon cleansing With laxative carry out. The intestines should be free of stool and food particles. For the procedure, the patient can turn to a light anesthesia through a Pain medication are moved and is monitored. The investigation can also without anesthetic can be made, but many patients find advancing the endoscope uncomfortable.
Please also read our page Anesthesia for a colonoscopy- is it dangerous?
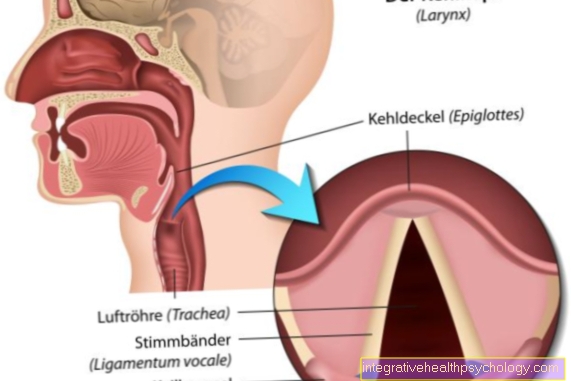
The doctor carefully inserts the endoscope into the intestine under vision. While he rinses with water and unfolds the intestinal wall through the introduction of air, the doctor pushes the endoscope to the transition from Large intestine and Small intestine in front. Now the actual procedure begins. The doctor withdraws the endoscope slowly and carefully observing the intestinal mucosa. The camera attached to the endoscope is movable and by rotating it the doctor can finally capture all areas.
The doctor can meanwhile Biopsies (Tissue samples) to remove polyps or small tumors or else Gastrointestinal bleeding with braces to breastfeed. Polyps in particular are easy to remove and are an important prophylactic measure. They are often the benign precursors of a tumor that can develop into a malignant one over time. The examination takes twenty minutes to half an hour, depending on the indication. Patients with previously administered anesthetic should not drive a car afterwards, have themselves picked up from the hospital and take it easy. High-risk patients are admitted to the hospital for an additional day for observation, depending on their previous illnesses.
Risks
The Risks of a colonoscopy are varied, but rarely occur in a trained doctor. However, they cannot be ruled out one hundred percent, which is why the patients are informed precisely in advance and must consent to the examination. Basically, the colonoscopy is well tolerated and usually without complications, but it can be too easy Abdominal pain after a colonoscopy come. Patients can also have the examination carried out consciously. The introduction and advancement of the Endoscope uncomfortable pain or feeling uncomfortable.
This can be counteracted with medication, but then spontaneously Intolerance reactions being able to lead. Patients who wish to have a colonoscopy under anesthesia may develop a hypersensitivity reaction to the drugs used. This can arise immediately or later, so careful monitoring is useful. This can cause a possibly occurring allergic reaction identified and countermeasures initiated immediately. When advancing the endoscope or by removing Cysts or polyps can cause bleeding. These can be directly breastfed using appropriate instruments.
A special risk group are patients who generally have a Coagulation disorder suffer or those who regularly anticoagulant drugs take in. With you it is Bleeding tendency significantly increased. Therefore, careful preparation and education is necessary before the examination. These patients often have to stop their medication several days before the procedure for the procedure to take place. Injuries to the intestinal mucosa from the inserted instrument can also occur, but are rare. The risk increases if the intestinal wall has already been damaged by, for example, chronic inflammatory diseases.
The intestinal wall can then be very thin and easily injured in places. In the worst case, the injury can lead to a complete rupture of the intestinal wall, a so-called perforation in the free abdominal cavity is then present. This complication can have far worse consequences. Even if the intestine has been thoroughly cleaned before the endoscopy, there may still be stool remains inside. In the event of a perforation, these can then enter the abdominal cavity and trigger inflammation there. One then speaks of one Peritonitis (Peritonitis), which under certain circumstances and depending on the general condition of the patient can have serious consequences.
Other organs can be affected and eventually become one Blood poisoning (sepsis), which represents a life-threatening situation and a intensive care as well as a treatment with Antibiotics needed. In order not to challenge this risk, the procedure should be carefully considered in terms of its necessity in the case of an acute inflammation of the intestinal mucosa. Not only can germs and bacteria be carried into the abdominal cavity through the injury in the intestinal mucosa, tumor cells can also be flushed out. As a result of the removal of tumorous tissue, individual tumor cells can be loosened if the wall is damaged and perforated. There is then the risk that they attach to other organs or other tissue and cause a new tumor to grow there (metastasis) trigger.
If a perforation has occurred, it is urgently necessary to carefully rinse the abdomen with plenty of fluid in order to minimize the risk of the complications mentioned. For patients with a known disease of the cardiovascular system, there are generally higher risks with operations than with healthy people. Each intervention especially under anesthesia puts a strain on the circulatory system and can lead to serious complications. The risks increase with age.
Use
The colonoscopy can be used as a preventive medical check-up from the age of 55 in the statutory health insurance. The examination can be repeated after 10 years. It offers a possibility of a present Colon cancer To be recognized early and thereby also to increase the chance of a cure. The examination is particularly useful and should be carried out earlier than offered by the health insurance companies if there is a family history of an inflammatory bowel disease or even cancer is known. However, since patients are examined with an indication of a disease even without symptoms, a careful balance should be made between actual effectiveness and the risk factors that exist for the patient.