Thyroid hormones
introduction
The thyroid gland produces two different hormones, thyroxine (T4) and triiodothyronine (T3).
The synthesis and release of these hormones is regulated by the hypothalamus and pituitary gland. They are primarily used to increase energy consumption.
The thyroid produces the hormones T3 and T4 on the one hand and calcitonin on the other. These hormones are discussed separately below.
Also read:
- Calcitonin
- T3 - T4 hormones
- TSH

Synthesis of thyroid hormones
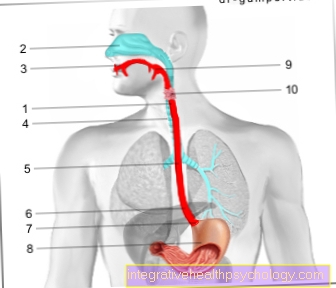
Through an active mechanism, under the influence of the Thyrotropin from the pituitary gland can the thyroid gland iodine from the blood absorb into the thyroid cells (thyrocytes).
This is done with the help of a sodium iodide symporter, which absorbs the iodide from the blood using an energy-consuming mechanism.
Then the so-called iodization takes place in the thyroid cells (thyroid cells). Here, the iodide in the cells is first oxidized by the thyrocyte peroxidase and then by the iodine transferase to the Amino acid tyrosine attached.
Then two iodized tyrosine residues condense with each other and form thyroxine (T4). This is then released from the thyroid cells and used as a Thyroglobulin in the Thyroid follicles saved.
Release of thyroid hormones
If the Thyroid hormones are to be released, a signal is first sent to the Thyroid follicle which is then sent by endocytosis Thyroglobulin return to the thyroid cells.
In the thyroid cells, the thyroglobulin is transported to the basement membrane. There the thyroglobulin is split off from its carrier substance and it is created free thyroxine (T4) and free triiodothyronine (T3).
These thyroid hormones are released into the blood in a ratio of 10-20: 1.
Because only T3 is the biologically active thyroid hormone, it is produced in the blood from T4 by mono-deiodination on the phenol ring. This deiodination is carried out by the individual organs and their Activation of deiodase controlled. For this reason, not all of the T4 is converted directly into effective T3, but only when an organ needs the hormone to work.
Transport in the blood
Either Thyroxine (T4) as well as Triiodothyronine (T3) are 99% in the blood to that Thyroxine-binding globulin (TBG) bound.
This is used to transport the hormones and prevents T3 from working prematurely. Only approx. 0.03% T4 and 0.3% T3 are unbound and therefore biologically active in the blood.
The half-life of unbound T4 in the blood is approx. 190 hours, the half-life of effective T3 is approx. 19 hours.
Inactivation
The Inactivation of the biologically active T3 thyroid hormone takes place in the kidney and liver by a renewed deiodination. The iodine released in the process becomes the thyroid to renew Hormone synthesis provided.
Regulation of thyroid function
The Thyrotropin (TSH) from the Pituitary gland regulates the Iodine intake and Thyroid synthesis in the thyroid.
Likewise, the release of T3 and T4 from the thyroid gland into the blood also decreases under the influence of the Thyrotropin to. T3 and T4 from the blood then practice one again negative feedback on the hypothalamus and pituitary gland out.
This means that a high concentration of thyroid hormones in the blood leads to an inhibition of the release of TSH from the pituitary gland and thus a lower production and release of thyroid hormones in the thyroid gland.
If the concentration of hormones in the blood drops, this leads to the stimulation of the hypothalamus and pituitary gland, so that more thyroid hormones are formed and released. This mechanism enables an exact regulation of the hormone concentration of thyroid hormones in the blood (euthyroid metabolism).
Effect of thyroid hormones
In general, only triiodothyronine (T3) is biologically effective and activates the entire metabolism. In detail, this means that T3 increases the energy expenditure depending on the dose.
This means an increased activation of the ATP-consuming sodium-potassium pump in the cell walls. This increases the energy expenditure of the entire body. This is also known as the caloric effect and only occurs a few hours to days after administration of the thyroid hormone.
Furthermore, T3 has an effect on the carbohydrate metabolism. By increasing glycogen breakdown in the liver, it lowers the glycogen content and at the same time increases the liver's own glucose production.
As a result, T3 has little effect on insulin, i.e. it slightly increases the sugar content of the blood.
It also has a comparable effect on fat metabolism. T3 mobilizes fats from adipose tissue and thus has a lipolytic effect.
Both the effect on the carbohydrate and fat metabolism serve to provide energy sources for consumption as part of the caloric effect.
In addition, physiological thyroid hormone concentrations have an anabolic effect, i.e. they serve to build muscle. Increased thyroid hormone concentrations, on the other hand, have a catabolic effect, i.e. promote protein breakdown
In addition, the thyroid hormones increase the responsiveness to catecholamines (adrenaline, noradrenaline), which in turn also increase the basal metabolic rate and the breakdown of sugar and fat.
Symptoms of a thyroid hormone disorder
According to the functions described above:
- a Hyperthyroidism (Hyperthyroidism) unwanted weight loss
- Racing heart (Tachycardia)
- slight shaking of hands
- slightly increased body temperature with increased sweating
- nervousness
- inner restlessness
and - sleep disorders.
An underactive thyroid (hypothyroidism), as occurs, for example, with iodine deficiency, leads to the opposite symptoms:
- Weight gain
- slow heart rate (bradycardia)
- fatigue
- paleness dry skin
and - flaky, brittle hair.
The causes of these diseases are very different and can be congenital, autoimmune (Graves disease) caused or by a tumor be conditional.
Therapy is correspondingly diverse, but in most cases it can be treated well by substituting hormones or suppressing the function.
The role and function of the thyroid gland
The thyroid is considered to be very important as it is crucial for the Energy metabolism of the whole body is. It produces the following three hormones: Triiodothyronine (T3), thyroxine (T4) and calcitonin.
T3 and T4 are colloquially referred to as thyroid hormones, while calcitonin plays a role in the metabolism for calcium and phosphate and is also produced by so-called C cells.
For the so-called Thyroid hormones (T3 and T4), which come from the actual thyroid cells, the thyroid gland does not only have The function of manufacturing, but also that of storing. For the production of the hormones, the thyroid gland needs iodine as a building block, which is taken from food and only taken up by the thyroid gland through the blood. This is used, for example, in radioiodine therapy.
The production and storage of the hormones takes place in so-called follicles, small fluid vesicles that are surrounded by cells of the thyroid gland. The hormones are then bound to you Carrier protein, thyroglobulin, saved.
Due to the extremely important function of the thyroid hormones, they are also subject to a control loop through the body. The thyroid, as a releasing organ, is stimulated by two glands in the head that are connected in series. In the so-called Hypothalamus will that Thyreoliberin (Synonym TRH), which is then called another gland Pituitary gland to release the Thyroid Stimulating Hormone (TSH) stimulates. This acts directly on the thyroid gland and causes the Production of T3 and T4 boosted and the stored reserves are mobilized to raise the blood level of these hormones. The hormones T3 and T4 in the blood, on the other hand, have a direct inhibitory effect on the two glands just mentioned, so that they produce and release fewer hormones. However, if there is not enough T3 and T4 in the blood, this inhibition subsides and the thyroid gland is stimulated again to increase the production and release of thyroid hormones.
The TSH is a very sensitive parameter for the current requirement for thyroid hormones. Therefore this value is determined very often.
More about this topic can be found: Thyroid levels
Summary
The thyroid produces two important thyroid hormones that are biologically largely ineffective thyroxine (T4) and the effective triiodothyronine (T3).
You will be in the Thyroid cells synthesized with the help of iodine and released from the thyroid follicles when necessary.
The effective T3 is released directly from the thyroid gland in much lower concentrations, but is instead formed from T4 by the mechanism of deiodination. This prevents the immediate effect of T3 and the individual organs can control the conversion and thus the effect themselves.
All the release and formation of the thyroid hormones is due to hormones from the Hypothalamus and the Pituitary gland controlled, which in turn are regulated by the current concentration in the blood. This principle is called negative feedback and is necessary to precisely control the concentration of hormones in the blood. The active T3 is inactivated in the liver and kidneys.
However, the thyroid can also release too much or too little hormone. This is known as hyperthyroidism or hypothyroidism and can be treated well in most cases and depending on the cause.


.jpg)









.jpg)