stroke
Synonyms
Apoplexy, ischemic cerebral infarction, cerebral circulatory disorder, apoplectic insult
introduction
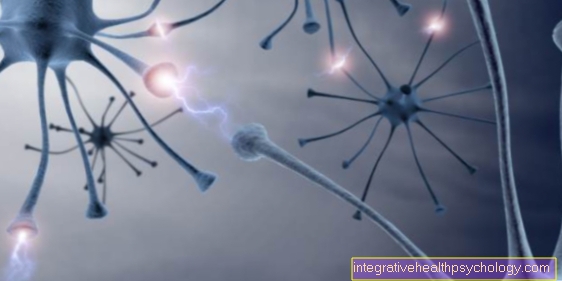
In the event of a stroke (medical: Apoplexy) it is about an insufficient supply of brain tissue with oxygen-rich blood and - depending on the duration of the undersupply - the associated death of the tissue.

What is a stroke
A stroke is damage to brain tissue as a result of an insufficient supply of oxygen to the brain. This under-supply of a circumscribed brain area is based on a circulatory disorder.
In 80% of cases, a stroke is caused by arteriosclerotic changes in the arterial walls ("vascular calcification"), arterial thrombosis or embolism. In all three cases there is a partial or complete occlusion of brain vessels, so that less blood reaches the brain tissue and thus less oxygen is available to the tissue.
therapy
A stroke is an absolute emergency. In neurology and neurosurgery, the concise motto "time is brain", Say"Time is the brain". Every minute counts, because the underperfusion of the affected brain area with oxygen-rich blood leads to the irreversible death of brain cells. Unlike muscle or liver cells, brain cells are not able to regenerate.
If you notice signs of a stroke, this is an absolute emergency doctor indication. This means that the person affected must be transported by ambulance to the hospital as quickly as possible, where therapy is then initiated.
In principle, one differentiates between two forms of stroke. Ischemic Stroke (anemic), and hemorrhagic stroke (bloody). In almost 90% of the cases it is an ischemic stroke, i.e. insufficient blood supply to the brain area. In the majority of cases, these are triggered by an embolism - i.e. a tissue plug. For example, the plug migrates from the carotid arteries into the brain, where it blocks a vessel.The larger the plug, the less it gets into the increasingly finer vessels, and the larger is the area that it cuts off from the blood supply. In this case, the neurologist or neurosurgeon gains access to the vascular system and works his way up to the plug. This is then removed and removed from the body, for which various techniques are available. The “stopper” has now been removed, the vessel and its end branches can be perfused again, and the brain area is supplied with oxygen again.
The situation is different with hemorrhagic strokes: Although this form is only responsible in a good 10% of cases, it has to be treated fundamentally differently. The cause here is bleeding within the brain. Not only does this increase intracranial pressure (please refer: increased intracranial pressure), as more and more (blood) volume is pumped into the skull, but does not flow out again via the vascular system.
The supply area is also no longer adequately supplied with fresh, oxygen-rich blood. The goal here must be to "patch up" the ruptured vessel and restore blood flow.
This is also done by accessing the vascular system, or - if the intracranial pressure is already greatly increased - by opening the top of the skull and treating it from the outside.
In summary, one can imagine an ischemic stroke as if there is a knot in the garden hose, which ensures that no more water comes out in the end.
A hemorrhagic stroke would then be a hole in the garden hose through which all of the water escapes. Accordingly, the treatment of the two forms of stroke differs.
Read more on the topic:
- Stroke measures
- Stroke therapy
Prognosis and course
The prognosis is crucially dependent on how extensive the loss of brain tissue is.
20% of the patients of the patients who come to the hospital because of a stroke die in the clinic as a result of the cerebral insufficient supply. For the surviving stroke patient, one can get one
Formulate the 1/3 rule:
1/3 of the sick remain in need of long-term care after a stroke, 1/3 of the patients can take care of themselves again after the stroke and corresponding rehabilitation measures and 1/3 of the patients experience almost to complete resolution of the symptoms.
Consequences of a stroke
The consequences of a stroke are very much dependent on the severity and localization of the circulatory disorder, but also on the time window between the event and the therapy or care in a hospital.
The damage that ultimately remains can include all kinds of neurological deficits, such as speech or visual disorders, paralysis and sensory disorders in certain regions of the body.
It is important that a rehabilitation program begins early after a stroke. This includes physiotherapy and, depending on the damage, occupational therapy and speech therapy. The attempt is made to actively restore the connections between the brain cells that have been damaged by the stroke. If rehabilitation is not started early, these connections can perish permanently. In this case, certain abilities or body functions cannot be regained. Therefore, early rehabilitation should be emphasized.
Find out more about this topic at: These are the consequences of a stroke!
Symptoms
In the event of a stroke, severe physical limitations suddenly occur, depending on the location of the vascular occlusion in the brain.
The following symptoms can be an expression of a stroke and should therefore be medically clarified immediately:
The patient finds it difficult to speak or has slurred speech. A stroke usually affects one half of the body, which is why the patient cannot move or feel the affected half of the body. The sensitivity, the feeling sense, and the motor skills are restricted or switched off. The patient can therefore no longer be sure. Often one corner of the mouth hangs down limply, which can make it difficult to eat. Chewing and swallowing disorders can also occur.
Other signs of a stroke can include incontinence (= unwanted loss of urine) or the changed perception of one half of the body.
Also read the article: Symptoms of a stroke and Stroke of the language center.
Signs of a stroke
A classic harbinger of a stroke is the so-called transitory ischemic attack (TIA). In very simple terms, the TIA is a "stroke light", in which, however, no brain tissue is destroyed and all symptoms regress completely within an hour (previous definition: complete regression of symptoms after 24 hours). A TIA is considered to be closely linked to a stroke and a typical harbinger of the later occurrence of a stroke.
Read more on the topic: Transient ischemic attack
Classic symptoms of a TIA, as with a stroke, are paralysis on one side, with reduced strength on the affected side. Strokes are usually strictly one-sided.
This is because one side of the brain is usually affected in isolation. If the right hemisphere is insufficiently supplied, the symptoms of paralysis appear on the left side of the body, as the nerve pathways of the hemispheres cross each other after they have left the skull. The symptoms of a TIA are similar to those of a stroke, with the difference that they regress. Other signs include, for example, slurred speech - patients are often fatally mistaken for drunk. In addition, it can also lead to states of confusion as well as gait and balance disorders (please refer Foot palsy) come.
A weaker handshake is also typical in comparison: the patient shakes and squeezes the hand on the affected side much weaker than on the healthy side.
A classic sign is paralysis of the facial muscles on one side of the face. The face looks limp and bulky there, while the healthy half of the face still functions without any problems. When sticking out the tongue, a deviation towards the affected side is often observed. The uvula in the mouth also follows this phenomenon. Loss of field of vision is also one of the typical signs of a stroke.
A visual field loss can be based on a large number of neurological diseases, but a sudden occurrence in combination with other symptoms typical of a stroke is trend-setting. Visual field deficits manifest themselves in that the patient can no longer see anything on one side of the visual field. The patient is not necessarily aware of the failure. Usually it is only discovered when the patient is conspicuously often "stuck" on corners or furniture because he has calculated the distance incorrectly.
Read more on the topic: Signs of a stroke
How to recognize a stroke?
Recognizing a stroke is not always that easy. Depending on the location of the circulatory disorder in the brain, different symptoms can occur. Occasionally these are so poor that the stroke is not recognized as such.
A proven scheme that has led to early detection of some strokes is the so-called "NEARLY". This scheme from the English-speaking area serves as a memory aid for quick identification and correct action. The "F" stands for Face and means that in the case of an acute stroke, one side of the face is often paralyzed. If you ask the person to smile, this is particularly easy to see. The "A" stands for Arms. Ask the person affected to stretch their arms straight out. If one arm cannot be held upright on its own, this also speaks for paralysis. The "S" stands for Speech and can be checked by speaking a simple sentence: if the language is difficult to understand, it is an acute language disorder. The "T" stands for Time: if the first three letters are positive, the emergency call should be dialed quickly.
Learn more at: What are the symptoms of circulatory disorders in the brain?
Symptoms of a stroke caused by an insufficient supply of oxygen to brain tissue
The arteries have certain supply areas of the brain and therefore associated functional areas of the body. On the basis of the symptom pattern that is present in a stroke, conclusions can be drawn about the affected vessel or the under-supplied area.
The front part of the brain is supplied by the internal carotid artery and the middle cerebral artery. An occlusion of the internal carotid artery has the following effects:
- The patient has a one-sided paralysis of the body, which mainly affects the arms and face. The affected half of the body also shows loss of sensitivity, i.e. Sensory disturbances.
An initially flaccid paralysis with a decrease in muscle tone can turn into spastic paralysis. - Speech disorders are possible if the speech-controlling side of the brain is insufficiently supplied (with most right-handed people, the left hemisphere is the place of speech control; the handedness does not necessarily determine the location of the dominant hemisphere).
- Temporary visual problems are possible symptoms of an embolic vascular occlusion in the area of the internal carotid artery, more precisely the opthalmic artery, which arises from the former.
The back of the brain is supplied by the two basilar arteries. Possible failure symptoms with a partial or complete vascular occlusion are the following:
- Dizziness is a symptom that can indicate a stroke.
- The patient may complain of difficulty swallowing.
- The occurrence of noises in the ears, impaired hearing (hearing loss) or double vision (= diplopia) should be examined for the presence of a stroke.
- So-called "drop attacks" are typical for restrictions in the vascular supply in the area of the basilar artery: the patient suddenly falls down without notice.
- If both arteries supplying it are blocked, the symptoms are drastic and can lead to loss of consciousness (= coma). Read more on the topic: Coma after a brain hemorrhage
In a stroke, the following two vessels are most frequently affected by a constriction or an occlusion:
- Internal carotid artery (approx. 50% of cases)
- Vertevral artery (approx. 15% of cases)
- Arteria cerebri media (approx. 25% of cases)
Risk factors for stroke
The following previous illnesses or factors favor the development of a stroke and should therefore be switched off:
- High blood pressure (= arterial hypertension)
- Smoke
- alcohol
- Obesity
- Sedentary lifestyle
- Lipid metabolism disorder
- increased cholesterol (= hypercholesterolemia)
- Diabetes (= diabetes mellitus)
- Cardiac arrhythmia (such as atrial fibrillation)
- Stroke in a 1st degree relative aged under 66 years
These factors cause, among other things, the development of arteriosclerosis (hardening of the arteries). The changes in the vascular wall are a main reason for the formation of thrombi and embolisms in the blood vessel system and thus for the possible occurrence of a stroke. In addition to the auricle, the carotid artery is the most common source of these occluding blood clots.
Frequency of the disease in the population:
The likelihood of developing a stroke is age-dependent and in the western industrialized countries is 300 per 100,000 people per year for the 55 to 64 age group.
For the ages of 65 to 74, the risk of suffering a stroke rises to over double: 800 per 100,000 people per year are affected by apoplexy.
Course of a stroke
The course of a stroke depends on the location and extent of the circulatory disorder.
The stroke is often preceded by so-called transient ischemic attacks, also known as TIA. This is a kind of harbinger with symptoms similar to those of a stroke itself. However, according to the current definition, these do not last longer than an hour. The risk of having a stroke in the following days after a TIA is around 10%.
In the event of a stroke, the impaired blood flow leads to the death of cells. This often results in irreparable damage, but the peripheral areas of a stroke are still partially supplied with oxygen and therefore have a longer time window before they die. Therefore, rapid therapy in the event of a stroke is crucial.
If the stroke is caused by a blood clot, a so-called lysis therapy can be initiated. Here the time window for effective and successful therapy is 4.5 hours.
You might also be interested in this topic: Healing after a stroke
Causes / development of a stroke
A vascular occlusion can lead to an insufficient supply of the brain tissue, so that it dies. The causes for the occlusion of the vessel are arteriosclerotic changes in the vessel walls (Vascular calcification), the obstruction of the vascular lumen by a blood clot (= thrombus) or the occlusion of a vessel by an entrained thrombus (= Embolus) to call. Bleeding from a cerebral artery can also cause tissue damage.
Venous thromboses (= Blood clots) of the intracranial veins or hypoxemia (= low blood oxygen levels) Cause of brain substance damage.
Read more about this under: Causes of a stroke
Circulatory disorder in the brain
A stroke is caused by a problem with blood flow in the brain. This means that there is either a reduced blood supply to a certain area of the brain or a hemorrhage. If the blood supply is reduced, what is known as cerebral ischemia occurs, i.e. the insufficient supply of oxygen to the brain tissue. This in turn leads to the death of the cells that need the oxygen to survive. The hemorrhage, on the other hand, leads to increased mechanical pressure on the cells, which ultimately also causes them to perish.
At around 80%, reduced blood flow is the significantly more frequent cause of all strokes.
It is caused by various factors such as
- arteriosclerosis
- Cardiac arrhythmias
and - Vascular inflammation
Promoted. The hemorrhage (usually a Subarachnoid hemorrhage) is favored, for example, by vascular bulges, so-called aneurysms.
Read more on the subject at: Circulatory disorder in the brain
Ischemic circulatory disorder
In around 80% of cases, a stroke is based on an insufficient supply of brain tissue with blood (Ischemia). The supplying vessels are either narrowed or completely closed. The most common is the internal carotid artery, usually at the fork of its main vessel (Common carotid artery) into the internal and external carotid arteries, affected by a narrowing or occlusion.
Two thirds of the strokes caused by ischemia are caused by changes in the vascular wall on the basis of arteriosclerosis: a thrombosis or an embolism, in which a blood clot is usually detached from the carotid bifurcation, is the cause of the narrowing of a vessel and the resulting undersupply of a certain brain area.
One third is triggered by blood clots that form in the heart and from there enter the cerebral vasculature as an embolus.
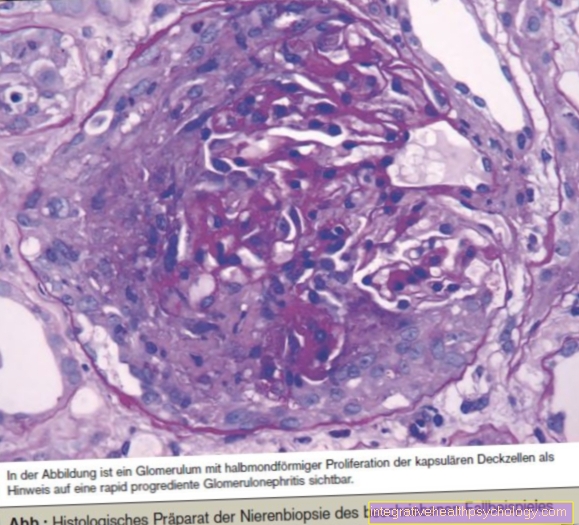
Cerebral hemorrhage
Circulatory disorders of the brain are caused by a bleeding in which blood flows into the brain tissue with a frequency of 15%. In most cases, the arterial walls are brittle due to longstanding high blood pressure and pre-existing arteriosclerosis. Other causes of bleeding are vascular malformations or bulging vessels, the walls of which can quickly tear (Aneurysms).
Read more on the topic: Cerebral artery aneurysm
A cerebral hemorrhage leads to severe headaches, nausea, vomiting and impaired consciousness. The neurological deficits appear within minutes to hours. Diagnostic imaging is necessary: a computed tomography (CT) examination can show bleeding.
You can find out more about this topic under our topic: Cerebral hemorrhage
Subarachnoid hemorrhage (SAB)
The subarachnoid space lies under a sheet of the meninges, which is made up of three sheets. The subarachnoid space lies between the leaf, the so-called pia mater, which is tightly attached to the brain, and the arachnoid. He is with nerve water (= Liquor) is filled and there are vessels running through it.
Often in the affected patients there is a vascular bulge at the base of the skull and this bulge suddenly tears, so that blood gets into the nerve water.
The symptoms of SAB are as follows:
- severe shooting headache
- Neck stiffness (= Meningism)
U.N - Impaired consciousness.
Using a CT or a nerve water puncture (= Lumbar puncture) a subarachnoid hemorrhage can be diagnosed.
Read more on the subject at: Subarachnoid hemorrhage
Intracranial vein thrombosis
Thrombosis is a rare cause of stroke. They occur in patients who have a coagulation disorder with a tendency to thrombosis and are not common at 1%.
Here, too, the headache is an early symptom of vascular occlusion, followed by neurological dysfunction, and minor seizures are also possible.
diagnosis
First of all, a precise description of the symptoms and their time course is necessary:
- When did the symptoms start?
- How are the complaints expressed?
- Have they gotten worse or better since they appeared?
- Did you experience any other symptoms in the course of the initial symptoms?
As part of the medical history, the attending physician asks whether there are any risk factors for arteriosclerosis such as smoking, high blood pressure, sedentary lifestyle and obesity. He also asks about any existing heart disease or other previous illnesses of the patient in order to get a comprehensive picture of him.
A neurological examination is carried out and particular attention is paid to the type and location of the functional failures, as this information can give the examining doctor an indication of the brain area affected by the insufficient supply.
The function of the 12 cranial nerves is checked in various tests such as the mutual pupillary reflex of the eyes, the mobility of the tongue or the motor function of the facial muscles. The reflexes of the arms and legs are checked, paying particular attention to any differences between the two halves of the body.
An examination by an internal medicine doctor is used to investigate the cause of a stroke: special attention is paid to the examination of the heart and vessels to find possible sources of embolism. Thrombi that form in the heart, detach and are transported into the head vessels, can develop in atrial fibrillation or after a heart attack. An ultrasound scan of the heart (= Echocardiography) shows the interior of the heart, heart valves and heart walls and can reveal a thrombus.
The neck vessels can be narrowed by a thrombosis, which is why the neck vessels should be listened to on both sides and an ultrasound examination should be carried out to visualize the vessel walls and the blood flow in the vessel.
A computed tomography image of the skull provides a representation of the brain tissue and the bony skull. Different shades of gray in the tissue can indicate bleeding or an insufficient supply of blood. In the early stages of a stroke, the affected tissue appears lighter than the healthy environment (= Density increase in the CT), but after 24 hours it is darker (= Density reduction in the CT image). Bleeding is generally darker than the surrounding healthy tissue.
Magnetic resonance imaging (MRI) is also possible. This represents vessels very well, which is why vascular malformations are easy to diagnose with this technique and can provide additional information.
See also: MRI of the brain
Stroke in the eye
The eye reacts more sensitively than any other organ to fluctuations in blood pressure and circulatory disorders. The "stroke in the eye" colloquially describes a so-called "Amaurosis fugax“, A short-term blindness.
Within a few minutes the vision in one eye is suddenly reduced, the patient sees as if through a frosted glass pane. Then a complete failure can occur for a few minutes, which then quickly regresses. Since there are often no further symptoms, many patients do not attach great importance to this phenomenon.
However, it is a sign of a TIA, i.e. a transitory ischemic attack. This is considered a harbinger of a stroke and should urgently be clarified neurologically and ophthalmologically.
Read more on the topic: Stroke in the eye
Stroke in the cerebellum
A stroke can also occur in the cerebellum. Various symptoms can occur here that are characteristic of a functional failure in this area of the brain. Thus, many cerebellar infarctions can be differentiated from strokes in the cerebrum.
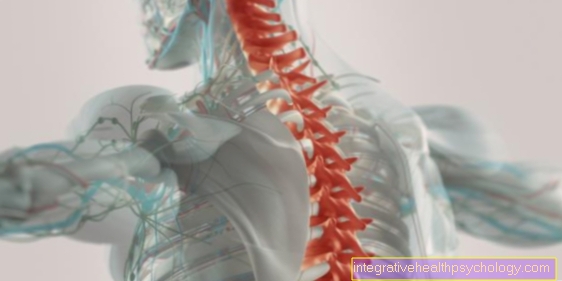
Stroke in the spinal cord
A stroke can also occur in the spinal cord. The spinal cord is supplied with blood by several arteries. A stroke in the spinal cord means that a circulatory disorder has arisen in this vascular system and, as a result, an undersupply of the spinal cord with the loss of nerve cells. In general, there are sensory disorders, pain and paralysis, which can have different causes.
See the next article for full details on this topic: Stroke in the spinal cord
Stages of circulatory disorder
Stage I.
At this stage, which is determined by chance, there is a narrowing of the vessels that does not cause any symptoms.
Stage II
Stage II is divided into two different types:
a) Transient ischemic attack, in short: TIA
The patient complains of neurological (= affecting the nervous system) symptoms such as paralysis, sensory or speech disorders, which have completely receded within 24 hours.
The failures show up in a supply area that is affected by the undersupply of blood.
b) PRIND
PRIND stands for "Prolonged Reversible Ischemic Neurological Deficit" and means that stroke symptoms last more than 24 hours, but resolve completely within 7 days. One could also speak of a TIA lasting longer than 24 hours (see above).
Stage III
Stage III characterizes a stroke with symptoms usually lasting several weeks. Damage that cannot be reversed is usually permanent.
However, there is the possibility of a partial regression of the neurological deficits such as paralysis, sensory disturbances or muscle weakness.
Stage IV
If a stroke has occurred and neurological impairments are long-term, this is referred to as the residual stage or stage IV.
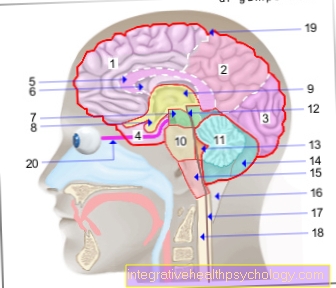
Anatomy of the vessels supplying the brain
The brain is supplied by so-called extracranial vessels, which split up and are called intracranial vessels if they have passed the base of the skull in their course. Extracranial means located outside the skull and these vessels include the branches supplying the brain, which extend from the main artery (= aorta) branch off: These arteries that supply the head are laid out in pairs, i.e. there is a left and a right artery. An artery is a blood vessel that leads away from the heart.
The vascular supply of the brain from the aorta takes the following course:
- The subclavian artery arises from the aorta, from which the common carotid artery branches off on both sides Carotid artery) from. The common carotid artery divides into the external carotid artery, which supplies the external head, and the internal carotid artery, which extends into the skull and supplies the brain with blood.
- The internal carotid artery and the basilar artery are the two main vessels that supply blood to the brain.
- The basilar artery emerges from the vertebral artery, which ascends along the spine to the head.
- Within the brain, the supplying vessels branch out in the so-called Circulus Wilisi, a vascular circuit from which the three cerebral arteria cerebri anterior (front), media (middle) and posterior (rear) emerge on each side. The blood supply is ensured by the cerebral vascular circuit, since one half of the brain can also be supplied by the vessels on the opposite side; this is called a collateral cycle.