Sulfonylureas
Synonyms
Medicines diabetes mellitus, diabetes medication, glibenclamide (e.g. Euglucon ®N), glimepiride (e.g. Amaryl®), gliquidon (e.g. Glurenorm®)
How do sulfonylureas work?
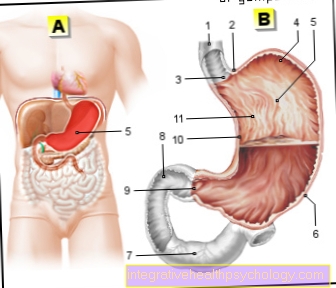
Sulphonylureas stimulate the pancreas to release more insulin. The prerequisite for this, however, is that the beta cells of the pancreas are still able to produce themselves. If the pancreas function is exhausted, sulfonylureas no longer help. Insulin therapy must now be started at the latest.
Glibenclamide (Euglucon ®N) is the most potent of all sulfonylureas and has been the most thoroughly studied. It works very quickly and is able to lower the blood sugar level below the normal fasting values of 80 to 110 mg / dl. If taken in an uncontrolled manner, hypoglycaemia can therefore be provoked.
When starting therapy with glibenclamide, the dose should be crept in to prevent hypoglycaemia. In practice this means that you start with half a tablet per day (3.5 mg) with a morning dose before breakfast and gradually increase the dose at weekly intervals. The maximum dose for glibenclamide is 3 times 3.5 mg (3 whole tablets) per day. The morning administration or the tablet division according to the scheme 2-1-0 (morning - noon - evening) makes the most sense at the beginning, because the pancreas is stimulated longer after ingestion throughout the day. If you always take the other tablets with main meals, do not vary the dose yourself and do not follow a diet, there is usually no risk of hypoglycaemia.
Note: hypoglycaemia
If you determine that your blood sugar level is too low, you should of course not take any more tablets. In this case, a longer-term dose adjustment should be made by your doctor. The evening meal and a small supper can lead to hypoglycaemia at night.
No effect despite the maximum dose
If the maximum dose of 3 times 3.5 mg per day has been reached and the blood sugar cannot be controlled as desired, insulin therapy must be considered. According to various studies, it can already be predicted that after glibenclamide therapy for about 6 years, the insulin reserves of the pancreas will be exhausted and insulin therapy will be necessary. Do not delay this point in time unnecessarily in order to avoid any consequential damage caused by the increased blood sugar levels. Regular blood sugar monitoring by your family doctor is therefore particularly useful when you are undergoing therapy with glibenclamide.
Dosage and dose adjustment
The recommended dosage is as follows:
- Glibenclamid: max. 3 times 3.5 mg in the division 2-1-0 (morning-noon-evening)
In the beginning, half a tablet is started in the morning.
- Glimepiride: max: 3 mg per day as a morning dose
In the beginning, one tablet is started in the morning.
- Gliquidon: max. 4 times 30 mg a day in 3 doses spread over the day.
At the beginning you start with 15 mg or half a tablet.
Every three months your doctor will check whether the current dosage has the desired blood sugar-lowering effect on the one hand and does not cause unnecessary hypoglycaemia on the other hand. In the event of an acute change in lifestyle, heavy physical exertion during sport or illness, or if you are bedridden, the dose must be adjusted. You can even reduce your dose on your own in the event of exceptional stress in order to avoid hypoglycaemia. In the case of fever and febrile colds, on the other hand, the body's need for insulin is increased; a dose adjustment in the sense of an increase in the sulfonylurea dose then makes sense.
Alcohol consumption and sulfonylureas
Alcohol increases the effect of sulfonylureas! The risk of hypoglycaemia increases. It can also provoke other side effects such as palpitations, headache, confusion and dizziness. If you do want to consume alcohol, drink it only with meals and in moderation.
Side effects
Gastrointestinal problems and impaired consciousness can arise, especially at the beginning of therapy with sulfonylureas. heartburn, Nausea, vomiting, bloating, diarrhea, constipation and blurredness See are not uncommon here. However, the side effects are due to the initial fluctuations in blood sugar levels and, especially at the beginning, there is no reason to stop the therapy early!
Since insulin production is strongly boosted under therapy with sulfonylureas, there is always a risk of hypoglycaemia if you skip meals or eat low-carbohydrates. The blood sugar level can drop below 50 mg / dl for a long time. Every main meal should therefore contain a proportion of carbohydrates (potatoes, rice, pasta, bread) to avoid such hypoglycaemia.
Sulphonylureas can impair the formation of blood, which is associated with persistent tiredness and poor concentration. Also, sulfonylureas can cause allergies, itching and swelling of the skin cause. If you notice any of these symptoms, you should see your doctor.
Like other oral anti-diabetic drugs, sulfonylureas can liver damage. Your doctor will therefore check yours at least every 6 months Liver values check.
When should sulfonylureas not be taken?
Sulphonylureas must not be taken if you are hypersensitive to medicines of the sulphonamide type. These include antibiotics that are used for urinary tract infections (cotrimoxazole). Some medicines for high blood pressure (diuretics) have a similar origin and have been stopped by some due to hypersensitivity. Your doctor will speak to you directly on some of these drugs to check your tolerance.
Sulphonylureas should generally not be used in diseases of the liver, kidneys and heart. However, with regular medical checks of blood values, you do not need to worry about possible organ deterioration.
Interactions
Antihypertensive drugs how Beta blockers (Metoprolol, Bisoprolol) or ACE inhibitors (Enalapril, Verapamil, Captopril, Ramipril, Lisinopril) can increase the effect of sulonylureas.
Hormone preparations and thyroid drugs also influence the effect. However, there are no interactions that absolutely prohibit therapy with sulfonylureas. Your doctor will respond individually to your medication regimen and establish a cost-benefit ratio for therapy with sulfonylureas.
Exclusion of liability / disclaimer
We would like to point out that medication must never be discontinued, applied or changed independently without consulting your doctor.
Please note that we cannot claim that our texts are complete or correct. The information may be out of date due to current developments.