Therapy pancreatic cancer
Synonyms
Pancreatic carcinoma (or more precise term in the narrower sense: ductal adenocarcinoma of the pancreas), pancreatic carcinoma, pancreatic cancer, pancreatic tumor
English: pancreatic carcinoma
The treatment of the patient requires intensive collaboration between surgeons, internists, radiation therapists and pain therapists.
During therapy, the previous definition of the tumor stage (tumor staging) is used as an essential aid to decision-making. There are corresponding therapy guidelines for each tumor stage. Unfortunately, the tumor is often only recognized at a later stage, so that healing (curative) therapy is often no longer possible.
Note
All information given here is only of a general nature, tumor therapy always belongs in the hands of an experienced oncologist (tumor specialist)!
surgery
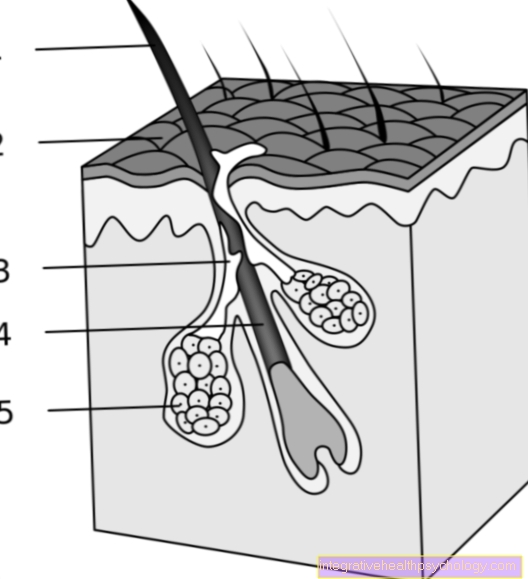
The operation should always be the therapy of first choice. The prerequisite is that the tumor is still operable, i.e. that it is limited to the pancreas and does not grow into any other adjacent organs (infiltrates) and that the patient is in good general condition. The aim of the operation is to remove the tumor as completely as possible, with a sufficient safety margin and together with the nearby lymph nodes. In the case of a tumor in the head of the pancreas, Whippl's surgery is often performed on the patient, in which the bile duct, gall bladder, duodenum and parts of the stomach are removed. One should try to preserve part of the pancreas if possible, because if the whole gland is lost, the digestive proteins (enzymes) formed by the pancreas will be missing. In this situation, the enzymes must be delivered in the form of a capsule (orally). Even more important, however, is the associated absolute lack of insulin (diabetes mellitus), which is formed by the β cells of the islet organ (islets of Langerhans) in the pancreas. From then on, patients have to self-administer insulin to themselves. For this purpose, the insulin is injected under the skin at regular intervals.
Pathological diagnostics
The removed pancreatic carcinoma is assessed microscopically (histologically) after removal. For this purpose, the tumor specimen is cut at certain points and at the resection margins. From these samples, wafer-thin sections are made, stained and assessed under the microscope. The tumor type is determined, its spread in the organ is assessed and the lymph nodes with removed lymph nodes are examined for tumor involvement. Only after the pathological findings can the tumor be clearly classified according to the TNM classification, which describes the primary tumor (T), the lymph nodes (N) and the distant metastases (M).
chemotherapy
During chemotherapy, the patient is given various drugs (Cytostatics) administered in various ways that Cell growth inhibit. Tissues that grow particularly quickly, including tumor tissues, are thus inhibited from growing and also partially killed. It has proven to be beneficial to combine cytostatics with various side effect profiles in order to be able to dose the individual substances at lower levels. Chemotherapy can be done before surgery to shrink the tumor and make it operable (neoadjuvant chemotherapy). If, on the other hand, the chemotherapy is carried out after the surgical removal of the tumor, it is referred to as adjuvant chemotherapy. Which form of chemotherapy is carried out must be decided on a case-by-case basis.
Finally, chemotherapy drugs can also be administered when there is no longer any prospect of a cure (palliative chemotherapy), so as to the tumor-related Chemotherapy side effects to reduce and improve the quality of life.
Further information:
- Conducting chemotherapy
- Chemotherapy substances
radiotherapy
Radiation therapy, like chemotherapy, can be used neoadjuvant, adjuvant and palliative. A combination of chemotherapy and radiation therapy is also popular. Since the pancreas is located deep inside the abdomen and is surrounded by radiation-sensitive organs, the radiation dose must be adjusted so that there are no radiation side effects on the neighboring organs.
Immunotherapy
Immunotherapy is a relatively new therapy option for treating various types of cancer. Here, antibodies and other substances are used that are directed against various structures of the cancer cell, which are characteristically increased in cancer cells and are essential for the cancer cell's metabolism. These drugs are administered in combination with drugs (cytostatics) but also as monotherapy. Several such drugs are still in clinical trials.
Palliative therapy
At the time of diagnosis, some patients have become inoperable and therefore incurable. In this phase of the disease, however, there are still many options to extend the patient's survival time and to maintain the quality of life as much as possible (palliative therapy). Many end-stage cancer patients experience severe pain that requires consistent management. This therapy requires a lot of experience from the attending physician, since it should not be spared even with the strongest painkillers (opiates) in order to achieve sufficient freedom from pain.
Another palliative measure is the maintenance of the bile and food passage. Because of its uncontrolled growth, the tumor can narrow the bile duct, the stomach outlet or the duodenum. These bottlenecks can be eliminated in a minimally invasive operation (endoscopic operation) by inserting a plastic tube (stent). Most often in the bile duct (common bile duct) affected by such a measure.
As already mentioned above, chemotherapy and radiation therapy are used with a palliative approach, because they prevent the tumor from growing or even achieve partial remissions (regression).
An important accompanying measure for all tumor patients should be psychosocial therapy, e.g. in the form of psychological support or through participation in self-help groups.
For more information on palliative treatment options for pancreatic cancer, see our article Palliative treatment for pancreatic cancer.
forecast
If pancreatic cancer is diagnosed and treated at an early stage, there is little chance of a cure. If the tumor develops in the head of the pancreas, it may be detected earlier than with other forms of pancreatic cancer (pancreatic CA) because the bile duct near the head of the pancreas is narrowed relatively early Jaundice (Jaundice) occurs, in the diagnosis of which the tumor is then recognized.
Overall, the smaller the tumor and the earlier the diagnosis is made, the better the patient's chance of survival. In general, the prognosis is good if the tumor is still present under 3 cm is and not yet spread to other organs or areas of the body Has. At approx. 10 to 15 percent the patient can then use the disease Surgery to be cured.
Unfortunately, most carcinomas of the pancreas are only diagnosed when their development is well advanced because they cause symptoms in the patient late and therefore they are not looked for. Healing (curative) therapy is then no longer possible in most cases. Nevertheless, therapy can slow the progression of pancreatic cancer.
Unfortunately, there is no generally valid screening test in which pancreatic cancer could be detected early via changes in the blood count (tumor markers).
Aftercare
The follow-up examinations usually take place at intervals of one to several months. The attending physician should determine the intervals and scope of the follow-up examinations depending on the tumor stage and the individual situation. In particular, every new symptom that appears should be discussed with the patient.
Important follow-up examinations are:
- Ultrasound examination (Sono)
- Computed tomography (CT)
- Determination of the tumor markers (by means of which the effectiveness of chemotherapy and / or radiation therapy can be checked and / or a recurrence of a tumor can be recognized.
Further subject areas
For more information on pancreatic cancer, visit:
- page pancreatic cancer
- Pancreatic Cancer Age
- Pancreatic cancer signs
- Pancreatic Cancer Causes
- End-stage pancreatic cancer
- Pancreas diet
- pancreas
- Diabetes mellitus
- tumor
- Pancreatic cancer prognosis
- Pancreatic back pain
- Palliative therapy for pancreatic cancer
All topics that have been published on the field of internal medicine can be found at:
- Internal medicine A-Z