Thyroid cancer therapy
Synonyms in the broadest sense
Therapy thyroid malignancy, papillary thyroid carcinoma, follicular thyroid carcinoma, anablastic thyroid carcinoma, medullary thyroid carcinoma
Note: thyroid cancer
For more information on the occurrence, symptoms and diagnosis of thyroid cancer, see: Thyroid cancer
therapy
The surgery is the primary form of therapy for malignant (malignant) thyroid tumors.
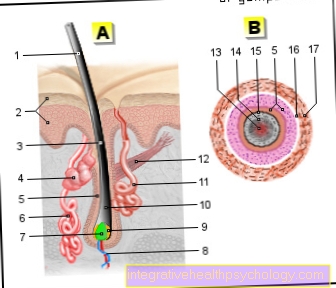
You remove the complete thyroid (=radical thyroidectomy) and the regional, i.e. the lymph nodes adjacent to the thyroid gland.
The operation will be carried out at iodinestoring tumors connected to the radioiodine therapy. Their aim is to remove all of the iodine-storing tissue from the body, since this possibly remaining thyroid tissue could lead to renewed tumor formation.
Three to four weeks after the surgery will be a Full body scintigraphy carried out with a low dose of radioactive iodine in order to detect iodine-storing thyroid remains and metastases of the carcinoma.
This investigation is followed by the Radioiodine therapy on: The patient receives a high-dose treatment of 131 iodine in several doses. These are repeated until no more iodine-storing tissue can be detected. The radioactive iodine is deposited in the cancer cells, but cannot be used to form thyroid hormones: it destroys the cells due to the radioactive radiation.
After the operation and radioiodine therapy, the thyroid hormones must be replaced (=Hormone replacement), as the body's own production is no longer possible.
Info: hormone replacement therapy
The substitution should take place in such a high dose that the TSH value remains as low as possible in order not to exert any growth stimulus on any metastases of the thyroid carcinoma that may still be present.
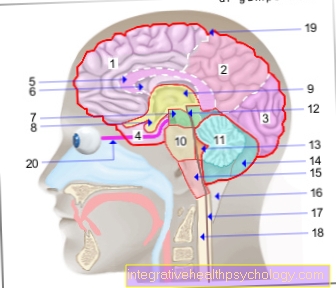
The stimulation of hormone-producing thyroid cells takes place in a closed control loop: The hormone TRH (= Thyrotropin Releasing Hormone) is released from the central nervous system and acts on the pituitary gland, which now increases TSH (= Tyroidea Stimulating Hormone, thyroid stimulating hormone ) is produced and released into the blood.
TSH works on the thyroid gland: The thyroid cells are stimulated to produce hormones, so that T3 and T4 (thyroid hormones) are subsequently released.
The low TSH level is achieved through a high therapeutic dose of the thyroid hormone T4, i.e. a high concentration of thyroid hormone T4 in the blood slows down the release of TSH in the sense of a negative feedback.
Anaplastic thyroid carcinomas are non-hormone-producing tumors that do not store iodine and are therefore not destroyed by radioiodine therapy. External radiation treatment is carried out after the operation because the undifferentiated tumors are sensitive to radiation.
C-cell carcinomas, on the other hand, are resistant to radiation. A radical thyroid operation is necessary to improve the prognosis for the patient.
Read more on the topic: Thyroid Cancer Types
Complications
The following complications of thyroid surgery should be mentioned:
The operation can injure neighboring structures. The irritation or injury to the Recurrent nerves (= Recurrent nerve des N. vagus), which runs near the thyroid gland, can become more persistent hoarseness and difficulty breathing.
After radioiodine therapy, inflammation of the head or salivary glands can occur Stomach ulcer come. If the treatment is carried out very often and in high doses, the risk of developing one increases leukemia to get sick by 1%.
Aftercare
Patients should have lifelong follow-up care. Follow-up care consists of regular biannual examinationswhich include a palpation of the thyroid gland and an ultrasound scan.
The determination of the is used to monitor the course of the tumor disease ThyroglobulinMade from healthy thyroid tissue and thyroid cancer cells. If this value becomes measurable again after a radical thyroid operation, this indicates the presence of metastases or another tumor disease (= relapse).
In addition, scintigraphic and X-ray controls can be carried out to detect metastases and recurrences.
Please also read: Metastases in thyroid cancer
Prognosis and course
The papillary and the follicular thyroid carcinoma have the best survival rates, over 95% or 90% of the sick survive the next
10 years after the illness. Patients under 45 years of age have a better prognosis than older patients.
The prognosis of the patient with medullary thyroid carcinoma is significantly worse: only half of the patients survive another 10 years after the disease.
Differentiated thyroid carcinomas occur in 20% of cases within
Metastases of the thyroid tumor 10 years after the disease, which make aggressive repeat therapy necessary.
Patients who attend a anaplastic thyroid carcinoma are sick have the worst prognosis: life expectancy is only about half a year.
Read more about this under Life expectancy in thyroid cancer.
prophylaxis
In radioactive accidents, e.g. In reactor accidents, the storage of radioactive iodine in the thyroid gland can be prevented by taking high doses of potassium iodide.