Therapy of ulcerative colitis
introduction
The main goals of ulcerative colitis therapy are to relieve the symptoms of ulcerative colitis, avoid complications, and thus maintain the patient's quality of life. A distinction is made between therapy for acute attacks and long-term therapy.
An important pillar of therapy is also the psychosomatic care of the patient.
All the options available today to treat ulcerative colitis are only symptomatic, that is, they cannot address and cure the root cause of the disease.
Read about this too Can you cure ulcerative culitis?

Therapy based on the guideline
In the acute episode, i.e. in the acute inflammation, the therapy can escalate depending on the severity of the disease.
In the case of a minor relapse, therapy with mesalazine is recommended first, which is also used in lower doses in remission therapy. It can be taken in the form of tablets or given as a suppository or foam if there is local inflammation of the rectum. If mesalazine is not effective on its own and even if the dose is increased, the guideline states that systemic therapy with corticosteroid steroids in the form of tablets should be started. The drug of choice is prednisolone for 8-12 weeks. If the form of ulcerative colitis is very severe, therapy should be given in a hospital. The corticosteroid steroids can be given in the hospital through a venous line, which makes them more effective than tablet form.
If this therapy is not sufficiently effective, immunosuppressants such as ciclospoprine A, azathioprine or tacrolimus (reserve medication) can be given instead. Antibodies such as infliximab are also available as alternatives.
If ulcerative colitis is so severe that immunosuppressive drugs or antibodies are necessary, the guideline recommends surgical therapy in the form of proctocolectmia. This means removing the entire colon and rectum, which is what heals ulcerative colitis.
Medical therapy

The drug therapy of ulcerative colitis is based on two pillars. First the therapy in the acute episode and second, the long-term therapy in the interval to maintain remission. Various medications are available for this.
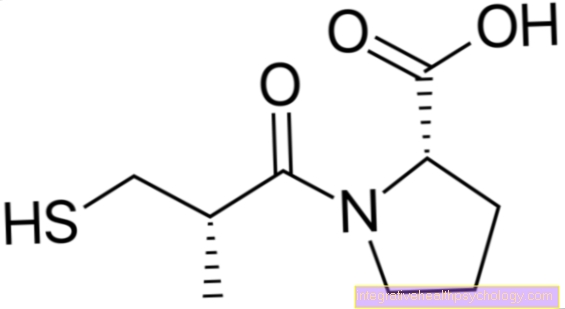
1. Salicylates (5-Amino-Salicylate / 5-ASA):
Mesalazine, for example, belongs to this group of drugs. This anti-inflammatory drug can be in the form of a tablet (orally) or via the anus (rectal) administered (suppositories). In the case of left-sided ulcerative colitis, the rectal administration of a klysma or rectal foam is sufficient. If there is inflammation that also affects the transverse colon (Transverse colon) and the ascending part of the colon (Ascendant colon), salicylates must be administered orally. Salicylates are used both in acute therapy and in maintaining remission.
How high the dose of sulfalazine is chosen depends on the severity of the attack.
This drug works by shutting down the body's immune system, so it is classified as an immunosuppressive drug.
It is so effective in ulcerative colitis because certain components of the immune system are overactive.
This is why this is also the drug of choice for maintaining remission, i.e. between the individual relapses in which the patient is actually symptom-free. This should delay the next surge longer.
If there is an extremely severe relapse, the sulfasalazine can be replaced by other immunosuppressants (for example azathioprine or cyclosporine) can be replaced or supplemented.
In addition, parenteral nutrition must often be provided in such a case, as the patient can no longer consume food in the normal way.
It is important to note that electrolytes, protein or blood may also have to be supplied parenterally.
If no or only unsatisfactory improvement can be achieved after 3 days even after regular treatment of such an attack, the patient must be operated on.
2. Glucocorticoids (cortisone):
This tried and tested drug has an excellent anti-inflammatory effect and is often used when salicylates are not effective enough. Glycocorticoids are not preferred for long-term therapy because they have lasting side effects (e.g. osteoporosis). However, some patients, such as those who have persistent ulcerative colitis disease activity, require long-term treatment with low-dose glycocorticoids. The most popular glycocorticoid is budesonide, because it is broken down particularly quickly in the liver and thus has fewer side effects despite its good effect in the intestine. They can be administered rectally, orally and also intravenously during therapy. At the end of the treatment with corticoids it is important that you “sneak out” them, that is, do not stop the medication abruptly, but rather regulate the dose down in a controlled manner by lowering the dosage of the menicament.
3. Immunosuppressants:
In the case of a therapy-refractory course of ulcerative colitis, immunosuppressive medication can be used so that glycocorticoids, which are more rich in side effects, can be dispensed with. These drugs work by shutting down the body's immune system. It is so effective in ulcerative colitis because of the overactivity of certain components of the immune system. This is why this is also the drug of choice for maintaining remission, i.e. between the individual relapses in which the patient is actually symptom-free. This should delay the next surge longer.
The drug azathioprine is initially the therapy of choice. Cyclosporine and, if necessary, methotrexate are available as alternative medication. Most immunosuppressants have a slow onset of action, so that the time until they take effect must be bridged with cortisone administration. But even these drugs often have side effects, so that the treated patients have to be examined regularly by the doctor and regular blood counts are necessary.
Read more on the topic: Immunosuppressants
4. Immunomodulators:
The new drug infliximab has also been approved for the treatment of ulcerative colitis since 2006. This antibody binds to TNF- ?, an inflammation-mediating messenger substance, which is neutralized by the binding and TNF-? can no longer exert its effect.
A more recent approach in therapy is that probiotics can also be used in addition to or as an alternative to 5-ASA in order to maintain remission. This term refers to the ingestion of selected intestinal bacteria, which support the healthy intestinal flora in fighting the disease. Often bacteria are from the strain E. coli Nissle used. Such therapy is only paid for by health insurances if there is an intolerance to 5-ASA.
In the acute episode, anti-inflammatory drugs are mainly used.
The most common way to do this is to use a drug called prednisolone, which has a similar effect to cortisol.
Since the disease is limited to the intestines, the anti-inflammatory effect is not needed in the whole body and can therefore be applied locally (for example as an enema or rectal foam) reduce the frequency and severity of side effects.
In the event of a severe episode, however, you switch to intravenous administration of prednisolone.
Read more on the subject at: Drugs for ulcerative colitis
Humira®
Humira® is the trade name for an antibody called adalimumab. Adalimumab is one of the so-called biologicals, which are artificially produced proteins that can intervene in various processes of the immune system. Humira specifically inhibits TNF-alpha (tumor necrosis factor alpha), which is involved in inflammatory processes. It is hoped that the inhibition of TNF-alpha will reduce the inflammatory activity during the acute severe flare-up of ulcerative colitis.
At the moment, Humira is not yet explicitly recommended by the guideline, but studies have already shown that remission (no diarrhea and no inflammatory spots in the colonoscopy) can be restored and maintained with the help of Humira. Humira can therefore be used in patients with a severe course when corticoids and azathioprine have not shown sufficient effect. It is important to note that Humira has a number of contraindications for which it should not be given. These include pregnancy, immunosuppressed patients, acute, symptomatic infections, chronic infections and especially tuberculosis, multiple sclerosis, cancer and moderate heart failure.
Side effects of such therapy can include symptoms of the flu, a decrease in blood content or the occurrence of an allergic reaction.
You may also be interested in this article: Infliximab
Remicarde®
Remicarde® (infliximab) is an antibody and, like Humira, belongs to the group of TNF-alpha inhibitors. It is used when corticosteroid steroids and azathioprine have not been effective in a severe ulcerative colitis attack. However, one study showed that after 8 weeks of administration of Remicarde, only 21% of the examined patients were in remission. The remaining patients still had inflammatory activity. Antibody therapy is considered safe and, if the contraindications are strictly observed, it can be used as an attempt to escalate despite a one-fifth chance of success.
The contraindications apply to TNF-alpha inhibitors in general, so that they are similar to those of Humira and are listed there.
Remicarde differs from Humira in that it partly consists of mouse protein, while Humira consists only of human proteins. As a result, when Remicarde is taken, allergic reactions to the mouse protein can occur, which can manifest themselves, for example, with a rash, itching or shortness of breath. Therapy should therefore be carried out under medical supervision in order to be able to detect an allergic reaction or other side effects promptly.
Methotrexate
Methotrexate belongs to the group of immunosuppressants and is a folic acid antagonist. The drug inhibits an important enzyme involved in DNA synthesis, thereby inhibiting it. Due to its cytostatic effect, it is often used as a chemotherapeutic agent for cancer. However, according to the guideline, the administration of ulcerative colitis is controversial because it was not able to show any advantage over a placebo preparation in randomized controlled studies, which represent the gold standard of medical studies. One point of criticism of the studies is the relatively low dosage of the drug and it is discussed whether a higher dosage could achieve the desired effect. Because of these discrepancies, methotrexate has not yet been recommended as a second drug in the case of azathioprine intolerance.
Read more on the subject at: Methotrexate
Treatment of particularly severe attacks
If there is an extremely severe relapse, sulfasalazine can be replaced or supplemented by other immunosuppressants (e.g. Azathioprin® or Ciclosporin). In addition, parenteral nutrition must often be provided in such a case, as the patient can no longer consume food in the normal way. It is important to note that electrolytes, protein or blood may also have to be supplied parenterally. If no or only unsatisfactory improvement can be achieved after 3 days even after regular treatment of such an attack, the patient must be operated on.
Read more about this under Ulcerative colitis flare-up
Surgical therapy of ulcerative colitis
Indications for surgical treatment are relevant bleeding, perforations (small holes in the intestines), first indications of early stages of colon cancer or a so-called toxic megacolon (a dangerous expansion of a section of the intestine).
In addition, there are some circumstances where the doctor can work with the patient to decide whether surgery is the treatment of choice. These include growth stagnation in children or contraindications to the drugs required for long-term therapy.
The removal of the large intestine (colectomy) is curative in ulcerative colitis, in contrast to Crohn's disease (curative). In the case of serious complications, such as the toxic megacolon, a perforation (Intestinal perforation), an insatiable bleeding, an ileus (bowel paralysis) or if drug therapy does not respond, surgery is indicated.
If an operation is necessary for ulcerative colitis, the surgeon usually removes not only the currently affected section of the intestine, but the entire colon. This means that the disease is cured. However, the operation naturally carries the risk of various complications. It is important that a resorvior is constructed from the small intestine, which then takes over the storage function for the stool as a replacement for the rectum.In some cases, an artificial anus is temporarily necessary (stoma, anus praeter), which is later moved back to give the patient a controlled bowel movement (Continence) to enable. A colectomy is also indicated if cancer cells or precancerous lesions (Dysplasias) being found.
Read more on the subject at: Removing the large intestine - is life without it?
Diet therapy
A particular diet is not necessarily indicated for ulcerative colitis. In severe, acute episodes, however, food intake can be reduced by a fully absorbable elementary foodAstronaut food) become necessary, in extreme cases even full intravenous (parenteral) nutrition is necessary. In the interval phases (remission; phases with low symptoms) a protein-rich whole diet should be consumed and only those foods that the patient cannot subjectively tolerate should be left out. Often times, Me is one of these foods. Should deficiency symptoms such as iron deficiency, vitamin D or calcium deficiency arise, these substances should be administered medically.
In principle, the ideal diet can look slightly different for each ulcerative colitis patient. Therefore, the motto is that what is good for you can be eaten without hesitation. In general, however, you should make sure that the food is not too flatulent and does not contain too much meat, fat or alcohol. On the other hand, eating fruit and vegetables, sufficient fiber and protein are beneficial. For some patients, avoiding dairy products or soft drinks has proven beneficial. Often it is also important to ensure that the food has a sufficiently high calorie content, because patients often lose massive weight due to frequent diarrhea.
In severe acute episodes, normal food intake may become impossible for a patient with ulcerative colitis. In such a case, it is necessary to change the diet to an artificial diet that does not have to go through the intestines, i.e. so-called parenteral nutrition. This can get into the body through the vein, for example.
A more recent approach in therapy is that probiotics can also be used in addition to or as an alternative to 5-ASA in order to maintain remission. This term refers to the ingestion of selected intestinal bacteria, which support the healthy intestinal flora in fighting the disease.
Bacteria from the E. coli Nissle strain are often used.
Such therapy is only paid for by health insurances if there is an intolerance to 5-ASA.
Read more on the subject at: Colon Disease Diet
Stool transplant
A stool transplant is the transfer of stool or the bacteria contained in stool from a healthy donor into a patient's bowel. The stool transplant pursues the goal of being irreparable restore damaged intestinal flora of the patient and thus to create or at least promote a physiological, i.e. healthy microbiome.
Stool transplants are to date not officially approved as a form of therapy, but count as an "individual healing attempt" if indicated accordingly. The only common use is in symptomatic Intestinal infection by the Clostridium difficile bacterium dar (pseudomembranous colitis).
Also what the therapy of inflammatory bowel disease Crohn's disease and ulcerative colitis are affected by a stool transplant currently doing research operated.
Most of the controlled studies that have been carried out to date have, however, produced mostly disappointing results. Only in children did a study in a small group of patients show a clear clinical response. In order to be able to make more precise statements about this, a few more years and studies will have to pass.
Worm eggs
The worm eggs come from the pig whip worm (Trichuris suis ovata). With a mild to moderate flare-up, taking the worm eggs biweekly may improve inflammatory activity. The worms, which are a few millimeters in size, hatch from the eggs and can reach the large intestine and are excreted with the stool. No serious side effects were observed when taking it, but this therapy has not yet been approved in Germany and is also not recommended.
homeopathy
Homeopathy is only recommended for ulcerative colitis as an adjunct therapy to support conventional medicine. There are a large number of possible homeopathic preparations for this disease, so only a selection is mentioned here.
Spiessglanzmohr (Aethiops antimonialis) can be taken for inflammation of the intestine with diarrhea and cramps. Another remedy that can have an effect on diarrhea is China officinalis, which should be taken three times a day. Ipecacuanha is a possible remedy three times a day for pain at the beginning of an attack.
Therapy during pregnancy
In therapy during pregnancy, a balance must be found between minimal medication and adequate treatment of ulcerative colitis. If mesalazine or corticosteroid steroids are taken in remission therapy, these can normally be taken in the same dose during pregnancy.
An acute flare-up represents a much greater risk for the unborn child and should be brought to remission as quickly as possible during pregnancy using the classic therapy regimen. The medication should be discussed with the treating gastroenterologist and the gynecologist before you want to have children and adjusted if necessary.
Azathioprine should only be given during pregnancy with special indications and with caution. Additional immunosuppressants such as ciclosporin A or tacrolimus should not be given during pregnancy as negative effects have been observed in animal experiments. In clinical practice, on the other hand, patients with transplants are known to have uncomplicated pregnancies while taking these drugs. TNF-alpha inhibitors such as Remicarde® and Humira® are strictly contraindicated during pregnancy.