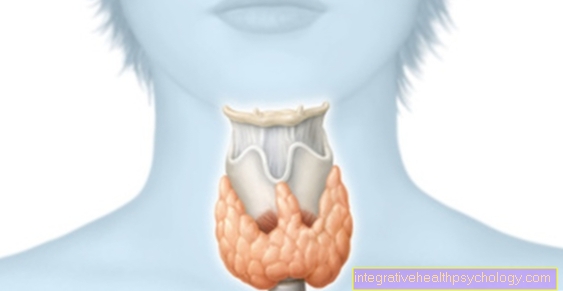
Autonomous adenoma of the thyroid gland
definition
An autonomous adenoma of the thyroid gland is a benign nodule (= adenoma) consisting of thyroid tissue that produces thyroid hormones in an uncontrolled (= autonomous) manner. Because of the excessive production of thyroid hormones, patients often suffer from an overactive thyroid, too Hyperthyroidism called. In the following text you will find out what the causes of such an autonomous adenoma can be and how it can be treated.

Causes of an autonomic adenoma
There are two main causes for the development of an autonomic adenoma: iodine deficiency and genetic factors. The thyroid depends on iodine as a building block in the production of its hormones. If there is a nutritional deficiency in iodine, the thyroid cannot produce enough hormones. This messes up the entire control cycle.
The result is that the thyroid gland is stimulated by our brain to produce more hormones. As a result, nodes now grow from new thyroid cells, which then produce excessive amounts of hormones with a better iodine supply - the result is an overactive thyroid. Even if the iodine supply in Germany has improved significantly in the last few decades, it remains one of the most common causes of autonomic adenoma.
Genetic factors can also lead to the formation of thyroid nodules that cannot be controlled by the body's own regulatory system. Here, too, the thyroid gland consequently produces too many thyroid hormones. If there is a genetic cause behind an autonomic adenoma, several members of a family are often affected, but they can differ greatly in the severity of the symptoms. An endocrinologist can help determine the cause.
Hashimoto's thyroiditis
The thyroid disease Hashimoto's thyroiditis is a chronic inflammation of the thyroid gland triggered by a misdirected reaction of our body's own immune system. Here, our immune cells mistakenly attack the body's own thyroid tissue. In this context, one speaks of an autoimmune disease.
Even with Hashimoto's thyroiditis, an overactive thyroid can occur in the meantime. However, this does not create any autonomous nodes in the thyroid gland. In addition, the condition of hyperfunction is only temporary, most of the patients with Hashimoto suffer from an underactive thyroid because so much thyroid tissue has been destroyed. This makes it easy to distinguish an autonomous adenoma from Hashimoto's thyroiditis.
Read more about this under: Hashimoto's thyroiditis
Diagnosis of an autonomic adenoma
The first suspicion of an autonomous adenoma is often made clinically, which means that the doctor can get an initial picture based on typical symptoms (such as sweating, rapid heartbeat, feeling of lump in the throat). In some cases, the autonomic adenoma can be felt on the outside of the thyroid gland - but this is by no means common, as very small lumps can often lead to severe symptoms.
Blood is now often taken for further diagnostics. The important thyroid values can be determined here. A typical constellation with an overactive thyroid in an autonomic adenoma would be increased thyroid hormones (so-called fT3 and fT4) with a decreased regulatory hormone that is formed in the brain (so-called TSH).
In the following, the lump can be visualized with an ultrasound of the thyroid gland. A thyroid scintigraphy may be necessary to differentiate between an autonomic adenoma and Graves' disease, a disease that is also associated with an overactive thyroid. This is a radiological exam that identifies highly active thyroid tissue and can thus indirectly show the lump.
Laboratory values
The most important laboratory values in thyroid diagnostics are the actual thyroid hormones fT3 and fT4, as well as the regulatory hormone TSH. TSH is produced in the brain and stimulates the thyroid to produce its hormones (fT3 and fT4). The thyroid hormones, on the other hand, have an inhibitory effect on the brain and reduce the release of TSH. This creates a control cycle in which the hormones can be kept at a continuous level.
If our thyroid now produces thyroid hormones in an uncontrolled manner, our laboratory values change: the concentration of fT3 and fT4 increase as they are increasingly produced. In addition, these hormones inhibit the release of TSH - as a result, this laboratory value drops. The classic laboratory constellation in the case of an overactive thyroid in the context of an autonomic adenoma is: ↓ TSH, ↑ fT3, ↑ fT4.
These symptoms indicate an autonomous adenoma
Autonomous adenoma can manifest itself in two ways. On the one hand, the growth of the thyroid gland can lead to a feeling of lump in the throat. This can lead to difficulty swallowing. On the other hand, and often more pronounced, are the symptoms that can be traced back to the overactive thyroid. These include, for example, excessive sweating, tremors, and hair loss. Palpitations and palpitations or even cardiac arrhythmias can occur.
Warm rooms are no longer well tolerated, the patients are very irritable and restless, have sleep disorders and mood swings. Many patients also report diarrhea and unwanted weight loss. The common occurrence of many of these symptoms is very typical of an overactive thyroid, but the severity of the symptoms can vary greatly from person to person. If you report these symptoms to your doctor, a blood sample and an ultrasound can help.
Therapy of the autonomic adenoma
There are several treatment options for the therapy of autonomic adenoma. It should first be noted that only symptomatic patients need to be treated at all. Many patients with an autonomic adenoma are often completely free of symptoms for a long time and therefore do not need any therapy. However, if symptoms such as palpitations or unwanted weight loss occur, it makes sense to therapeutically contain the overactive thyroid.
As a rule, the treatment of first choice here is taking tablets. The so-called thyreostatics inhibit the uptake of iodine in the thyroid gland and thus reduce the new build-up of thyroid hormones. The common active ingredients are thiamazole, carbimazole or propylthiouracil. If drug therapy is insufficient or is not desired by the patient, there is also the option of radioiodine therapy and surgical removal of the thyroid gland.
Both options have in common that by destroying or removing thyroid tissue, they usually lead to a permanent cure for the overactive thyroid. However, there is often very little or no healthy thyroid tissue left, which is why patients subsequently have to take thyroid hormones in tablet form for life. Which form of therapy is chosen should be weighed up individually with a specialist.
When do you need radioiodine therapy?
Radioiodine therapy is a common treatment option for an autonomic adenoma. Here we take advantage of the fact that only the thyroid can accumulate iodine in our body and any excess iodine is excreted in the urine. The patient is given radioactive iodine, which is absorbed into the thyroid gland, where it causes local destruction of the thyroid cells. In this way, the autonomic adenoma can also be removed.
Whether a patient needs radioiodine therapy must be carefully considered with a specialist. The first choice of therapy is often the so-called thyreostatics, which are taken as tablets and reduce thyroid hormone production. Only when this therapy cannot sufficiently suppress the symptoms of hyperthyroidism or the patient is looking for a definitive treatment option can one consider radioiodine therapy.
Prognosis of an autonomic adenoma
The duration of the disease in an autonomic adenoma is very individual for each patient. Many patients with an autonomic adenoma are symptom-free, their thyroid values are in the normal range and the nodule is only an incidental finding e.g. detected in ultrasound. Of course, these patients do not need any therapy and should only make use of regular laboratory checks.
If there is symptomatic hyperthyroidism, this should be treated. The so-called thyreostatics tablets must be taken for at least 8-12 months before an attempt to withdraw them can be started. If the patient opts for radioiodine therapy or surgical removal of the thyroid gland, the disease is finally cured. For this, the thyroid hormones must be taken in tablet form for life.
The prognosis of an autonomic adenoma is therefore good, as there are several treatment options. The autonomic adenoma is also a benign nodule and shows no tendency to develop into thyroid cancer.
Course of disease
The course of the disease in an autonomic adenoma can be very different, but basically often follows the same pattern. Many patients are asymptomatic at the onset of the disease. The autonomic adenoma is caused by increased growth stimuli in the presence of iodine deficiency. Only when the patient takes more iodine again can this lead to an overactive thyroid with typical symptoms such as rapid heartbeat, sweating and weight loss.
Depending on the severity of the symptoms, the diagnosis is often made quickly through a laboratory test. If patients are on adequate therapy, thyroid levels should return to normal and any symptoms of illness should go away.





















.jpg)

.jpg)
