Atrial flutter and atrial fibrillation
Synonyms in the broadest sense
- Tachycardia absoluta
- Tachyarrhythmia absolutely
- Racing heart
- Heart pounding
definition

Atrial flutter or fibrillation is a temporary (intermittent or paroxymal) or permanent (permanent) Cardiac arrhythmia with disordered activity of the auricles.
With atrial flutter, the atria contract with frequencies of over 250-350 beats per minute. With atrial fibrillation frequencies of 350 to 600 beats per minute are reached.
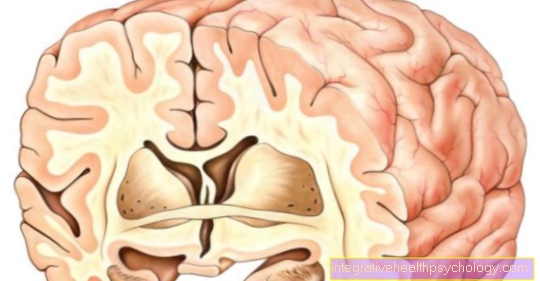
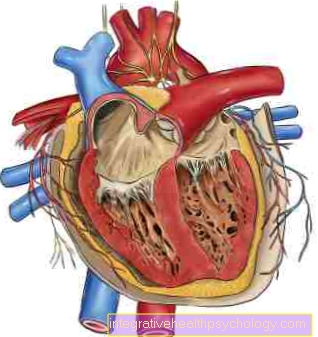
4% of those over 60 have Atrial fibrillation. Atrial fibrillation with Tachyarrhythmia absoluta is the most common form of supraventricular Tachycardias. The atria carry out chaotic actions where that blood is no longer effectively pumped into the chambers. thanks to the Filtering ability of the AV node only some of the electrical potentials that come from the atrium are transferred to the ventricle, so that the ventricles contract quickly, but there is no ventricular flutter. However, the transition of the potentials is absolute arrhythmic, therefore one speaks of a tachycardia absoluta.
So the atrial flutter / fibrillation is one Disease of the atria, but also affects the ventricles. Long-standing atrial flutter / fibrillation is compatible with life, even if it involves risks.
Symptoms of atrial flutter
Symptoms of atrial flutter and atrial fibrillation occur mainly in the paroxymal (seizure) forms and are strongly dependent on the frequency that is transferred to the ventricles. The affected person feels dizzy, palpitations and palpitations. Patients feel the heart jump or bounce, describe that something is wrong with the heart. Since the unusual beating behavior of the heart often leads to anxiety, most patients also have anxiety or pressure on the chest.
In the case of severe tachyarrhythmia, physical performance can also be restricted, including breathlessness and the accompanying feeling of fear. In addition, polyuria (increased urine volume) occur. A pulse deficit can also be determined; that is, individual heart actions that can be heard with the stethoscope on the heart do not lead to a pulse beat.
In many cases, however, atrial flutter does not trigger any noticeable symptoms.
Read more on this topic: Symptoms of atrial flutter
General causes
Atrial flutter / fibrillation can occur in all diseases of the heart that are associated with damage to or overstretching of the atria. Diseases that often lead to atrial fibrillation:
- Heart failure (the heart does not have enough strength to pump all of the blood out of the chambers and atria, there is always something left behind. Thus, step by step, the atria, for example, expand)
- Mitral valve disease (the mitral valve separates the left atrium
from the left ventricle, it is e.g. permeable, blood is pumped into the atrium with each ventricular contraction, which is overstretched. - Metabolic disorders, e.g. Hyperthyroidism
Multiple reentry circuits are considered to be the basic mechanism of atrial flutter / fibrillation. During normal cardiac activity, any potential is extinguished once the ventricular muscles have been reached, as they are then only surrounded by tissue that is difficult or impossible to excite at all. The tissue is said to be refractory. The cells must first “recover” from the potential that has just passed. In the case of a damaged area of heart cells, the transmission of potentials can be slowed down. This excitation can now run through the damaged area in the opposite direction, since it reaches it at a point in time when it may no longer be refractory. The danger here is a “reentry” of the excitation wave into the surrounding tissue when it is no longer refractory. An excitement can develop which, as it were, entertains itself.
You might also be interested in the topic: Causes of atrial fibrillation
Causes of atrial flutter

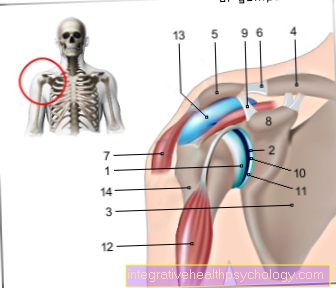
At the Atrial flutter there is an irregular contraction of the left and right atrium of Heart and resulting Cardiac arrhythmias. Between atria and left and right chamber of the heart is in the Stimulus transmission system a knot named as filter acts and only everyone 2nd to 3 impulses transferred to the ventricles.
The atrium beats with atrial flutter faster than the chamber. Of the AV node serves as a vital filter station.
If this station didn't exist, the entire heart would be in irregular, too fast movements devices. The causes of atrial flutter vary, but most often indicate one underlying structural disease down.
So can Enlargement of the heart and coronary heart diseaseleft untreated for a long time lead to atrial flutter. Especially elderly are affected by this stimulus conduction disorder.
Often there is evidence of atrial flutter Incidental finding. The rapid contraction of the atria during atrial flutter can result in a Heart rate in the atria of up to 150 beats per minute come.
A distinction is made in atrial flutter typical and atypical atrial flutter. At the typical atrial flutter the impulses that trigger the irregular contraction of the atria arise in the area of the atria, more precisely in the area of the so-called Tricuspid valve.
At the atypical atrial flutter arise the circular motions further away from said Heart valve. The distinction between typical and atypical atrial flutter is therefore made on the basis of the localization. Symptoms and diagnosis of both flutter variants are the same.
Sometimes you can't find out what the root cause is. Older people in particular are affected by this cardiac conduction disorder. In some rarer cases Atrial fibrillation or atrial flutter can also be diagnosed in younger people. In older people are mostly Enlargement of the heart due to poorly adjusted Blood pressure responsible.
When the heart and its ventricles expand, so do the atria, which the conduction pathways for the transmission of stimuli lead past. At strain if these orbits lengthen, there is one extended stimulus transmission.
While the first excitement still over the Heart muscle rolls, the second is already beginning, a condition that does not exist in normal-sized atria. This results in the typically rapid, uncontrolled contraction of the atria.
Another important cause are coronary heart disease, a disease of the heart in which the supplying Blood vessels are too tight and cannot pump enough oxygen into the heart muscle.
Untreated CHD not only leads to an increase in Heart attack riskbut also to one increased risk of atrial flutter or atrial fibrillation. Especially for atypical atrial flutter smallest scars responsible in the area of the cardiac stimulus transmission system.
They are mostly caused by small heart attacks in the past that were not noticed (silent heart attacks).
Sometimes you can see such scarring in the EKG determine, sometimes one can only suspect such scars as the cause.
The difference between atrial fibrillation and atrial flutter is in the achieved frequency and the typical ECG image. Atrial fibrillation is faster than atrial flutter; the EKG does not show sawtooth-shaped P waves, but rather irregular spikes.
consequences
As a result of atrial fibrillation, a decrease in cardiac output can occur because the atria with their pumping function no longer contribute to the filling of the chambers. In addition, no permanent ventricular tachycardia due to transmission via the AV node leads to damage to the ventricular muscles, which can e.g. lead to heart failure (heart failure). Most dangerous, however, is the slowed blood flow in the overstretched atria. Since there is no longer an orderly contraction, there are places where the blood is almost standing. This can cause blood clots to form in the atrium, which can lead to strokes or pulmonary embolisms.
Read about this too Blood clots in the head
Diagnosis of atrial flutter
The classification of atrial flutter / fibrillation is important. The risk of complications must be assessed on the basis of various questions.
- Is there a permanent or a paroxymal form?
- How long do each episode of atrial fibrillation last?
- Are there underlying diseases? And if so, which ones?
- What is the effect of atrial fibrillation on the circulation?
- Is there a risk of a heart-related blood clot?
Other embolisms or strokes in the patient's history are at high risk. Even with one Mitral stenosis as an underlying disease, the risk of complications is increased. Other risk factors are high blood pressure, Diabetes mellitus and a manifest heart failure.
The diagnosis of atrial flutter / fibrillation is made via the clinic (fast, irregular pulse with pulse deficit) and EKG, if necessary Long-term ECG posed.
The ECG shows irregular intervals between the QRS complexes. The baseline between the QRS complexes is marked by small fluctuations (flicker waves) (can be seen most clearly in lead V1)
In addition to the pure diagnosis of the arrhythmia, a TEA made to rule out atrial thrombi. During a TEE (trans-oesophageal echocardiography) an ultrasound head is placed in the esophagus up to the level of the atria. This can be used to find blood clots that have formed.

ECG in atrial flutter
The ECG shows a typical irregular spread of excitation. The so-called QRS complexes, which stand for a resulting heartbeat, are shown at irregular intervals on the ECG.
Sawtooth-shaped so-called P waves are characteristic, these are small bumps in front of the actual EKG peak that show the spread of excitation in the atrium.
You might also be interested in: What are the ECG changes in atrial fibrillation?
Treatment of atrial fibrillation
When treating atrial flutter, the Age of the patient also Secondary diseases included. In young patients who have no major comorbidities, an attempt is first made Desolation the corresponding place in Stimulus transmission system, which generated irregular pulses, to normalize again. Before the procedure, a so-called Swallow echo (TEA) carried out.
The patient must be similar to a Gastroscopy swallow a tube with a small one at the tip Ultrasound head is located. This is via the esophagus very close to the Forecourt pushed to see if there are any blood clots in it.
In this case a surgery not performed as there is a risk of blood clots loosening and dangerous Embolisms or Heart attacks trigger.
This desolation is called Catheter ablation designated. He will be in a special Cath lab carried out under sterile conditions. About the Inguinal artery becomes a small wire forward to just before that heart pushed. The patient is awake, the puncture site only becomes locally anesthetized.
Via the catheter you can EKGs be slid off from every accessible part of the heart. So you can find out pretty exactly at which point of the heart stimulus transmission the additional impulses arise.
Where the catheter is currently located is indicated by a Fluoroscopy clear. If the point from which the additional impulses come has been found, this point is reduced to approx. 50 degrees heated. This makes this part of the nerve tract unusable. After a short wait, the cardiologists make sure that this area is still firing impulses a short time later.
If not, the wire is removed again and the puncture site is closed with a pressure bandage. The intervention delivers in over 90% of the cases Successes. Most patients are then relieved of atrial flutter.
At the atypical atrial flutter Finding the impulse site is much more difficult, as it can be distributed anywhere in the atrium. If it is found, the area can ultimately be desolated.
In those cases where successful ablation cannot be performed, an medication be tried. The chances of success are much worse than with surgery.
If the catheter treatment fails, atrial flutter can be attempted using so-called Beta blockers or antiarrhythmic drugs to treat. However, the chances of success are lower than with the ablative measure. If the catheter technique was unsuccessful, immediate treatment is much more important Blood thinning start to avoid dangerous embolisms or heart attacks.
You can find more information on this topic at: Treatment of atrial fibrillation
Guideline
There is one for atrial flutter and atrial fibrillation internal treatment guideline. It shows the diagnostic options and steps to be taken as well as the treatment of the disease.
Anticoagulation
Anticoagulation is one systematic inhibition of blood clotting. With atrial flutter and atrial fibrillation, this is necessary because of the rapid atrial movement blood can clot quickly in an uncontrolled manner and these so-called thrombi can be washed out into the bloodstream.
Mostly they get over Arteries in the head area and loosen Strokes out. Unnoticed Atrial flutter or flicker are the most common causes for strokes. Could through a catheter technique no regular rhythm must be started with a consistent anticoagulant. This treatment is for life to take.
The most famous preparation is Marcumar. It inhibits Vitamin K, which is significantly involved in blood clotting. Marcumar is taken gradually until a certain value in the blood is reached. The amount to be taken varies from person to person.
Regular blood tests indicate whether the patient needs to take one, half or a quarter tablet.
There are now newer drugsthat are easier to take (only once a day). However, long-term values and are missing Renal failure these drugs cannot be used without further ado. Under blood thinning, it must be noted that the Bleeding tendency in patients, it takes longer for a bleeding wound to close.
Especially before operational interventions the blood thinning must be stopped. The Marcumar should be approx. 5-7 days before the procedure be dropped off; be discontinued; be deducted; be dismissed. The patient must then overlap Heparin take in (Abdominal injection). Depending on the procedure and the wound, approx. 2-5 days after the procedure be started again with Marcumar. For the newer blood-thinning drugs, manufacturers state that only on the day before the procedure the drug should be paused. You can start again immediately after the procedure. Even with dental interventions, such as Pulling a tooth It may be necessary to pause blood thinning treatment before the procedure.
forecast
The prognosis depends heavily on the underlying disease. There are no significant prognostic differences between the application of the individual forms of therapy (frequency or rhythm control).
Read about this too What is the life expectancy with atrial fibrillation?