Atrial fibrillation therapy
Therapy of atrial fibrillation and atrial flutter
If possible, a causal (causalAtrial fibrillation therapy should be sought, which treats the underlying disease.
Atrial fibrillation, which occurs acutely, usually disappears spontaneously after therapy has been initiated. If it persists, a decision has to be made between two equivalent therapy concepts: frequency control and rhythm control.
You might also be interested in:
- What are the ECG changes in atrial fibrillation?
- What is the life expectancy with atrial fibrillation?
The main therapeutic goal of both concepts is to improve the circulatory situation and to prevent complications from blood clots.
1. Frequency control: (the speed of the heart's actions should be reduced)
Drug-based frequency control: Digitalis preparations (especially for additional cardiac insufficiency) and class II antiarrhythmics (beta blockers, e.g. for the underlying hyperthyroidism) or calcium channel antagonists such as verapamil are used for this therapy. Problems arise from the side effects of the drugs. The problem is that antiarrhythmic drugs (especially class I antiarhythmics) can themselves trigger arrhythmias as side effects, especially in previously damaged hearts. Prescribing this type of medication must therefore be considered very carefully.
If, in rare cases, drug therapy is not sufficient to bring the frequency under control, there is the possibility of an AV node ablation (ablation = removal and sclerosing of unwanted tissue by current doses) with subsequent use of a pacemaker.
2. Rhythm control: = regularization (also called cardioversion) of the atrial flutter / fibrillation = conversion into a sinus rhythm.
Requirement:
- the atrial flutter / fibrillation no longer exists for approximately 12 months
- the treatable causes are eliminated
- no presence of advanced heart disease
The chances of success in the regularization attempt are reduced if:
- too much stretching of the atrium
- Heart failure (heart failure)
- The arrhythmia has been around for too long
If the atrial flutter / fibrillation persists for longer than 48 hours, anticoagulation therapy (it removes any blood clots) must be carried out (for therapy with anticoagulants see below) before attempting regularization for four weeks.
After regularization, an anticoagulation (medicinal blood thinning) is always carried out.
The pros and cons of both therapeutic approaches:
Pro rhythm control:
- The frequency control alone usually does not solve the circulatory problems, the atria still beat irregularly, the pumped blood volume fluctuates.
- Is particularly suitable if the atrial fibrillation has only existed for a short time (less than 48 hours) or has occurred in the context of acute illnesses and there is no great atrial distension
Pro frequency control:
- low subjective and objective symptoms
- in all cases in which rhythm control is not particularly suitable (prolonged existence, atrial distension, multiple relapses)
Medication
Drug treatment for atrial fibrillation depends on the cause. In addition, the drugs, the so-called antiarrhythmics, have clear indications, contraindications and interactions with other drugs. Frequently used drugs for atrial fibrillation are beta blockers, flecainide, propafenone and amiodarone.
Beta blockers
Beta blockers like bisoprolol are drugs that work on what are known as beta adrenoreceptors. They are used for various heart diseases, such as high blood pressure, heart failure, too fast heartbeat (tachycardia) and cardiac arrhythmias such as atrial fibrillation. Beta blockers can cause side effects such as weight gain or erectile dysfunction; they can worsen existing diseases such as bronchial asthma and diabetes mellitus. In the cardiovascular system, there can be a sharp drop in blood pressure, a slow heartbeat and circulatory disorders.
You might also be interested in: Beta blockers and sport - how do they get along?
Anticoagulation therapy
The long-term therapy of atrial fibrillation generally requires the consideration of an antithrombotic (blood-thinning) treatment. The aim of this therapy is to make the blood less coagulable and thus to prevent the formation of clots (thrombi). The reason for this is that atrial fibrillation is a common cause of strokes and embolisms. If the blood is diluted with medication, the risk of clots forming is reduced. Whether there is an increased risk of strokes and embolisms depends on various factors that are calculated using the CHADS2 score according to the current guidelines for the treatment of atrial fibrillation. The treating cardiologist decides whether medical blood clotting is necessary.
Read more on the topic: Xarelto®
You might also be interested in:
- Stroke - What Are The Signs?
- embolism
In anticoagulation therapy, certain drugs influence the coagulability of the blood (coagulare = Latin for falter).
Anticoagulants that are used for this would be ASS 100 (e.g. aspirin) or Marcumar (a vitamin K antagonist). If the atrial flutter / fibrillation has persisted for more than 48 hours, such therapy is necessary before cardioversion. After a cardioversion, anticoagulation is generally initiated for four weeks. Whether a prophylaxis against clots is otherwise necessary is decided based on the factors age, heart disease and certain risk factors:
Patient: Therapy
Under 60 years of age, no diseases: no therapy
Under 60 years of age, heart disease: ASA 300mg / d
Over 60 years, no risks: ASS 300mg / d
Over 60 years of age, diabetes mellitus or CHD: Marcumar
Over 75 years: Marcumar
Patients (regardless of age) with risk factors heart failure, high blood pressure, overstretched left atrium, hypertyreosis: Marcumar
Which drugs are used there?
Vitamin K antagonists, the so-called Marcumar, have been used to thin the blood for years. Marcumar is used to treat and prevent blood clots and vascular occlusions and heart attacks. Marcumar therapy, however, requires regular coagulation controls (INR value). For some years now there have been new drugs for thinning the blood, the “new oral anticoagulants” (NOAC). These drugs show good effectiveness and easier application than Marcumar. These include "thrombin inhibitors" and "factor Xa inhibitors".
You might also be interested in the topic: What should be considered when stopping Xarelto?
Marcumar
The blood-thinning drug Marcumar contains the active ingredient phenprocoumon, a "vitamin K antagonist". In addition to the long-term treatment of a heart attack, it is used for the prevention and therapy of thrombosis.
If atrial fibrillation is at risk of developing blood clots and causing strokes or embolisms, Marcumar can be used to reduce the risk of clot formation. The dosage of the drug is adjusted individually and the doctor regularly measures the state of blood clotting. The INR value is used as a measure of the thick or thin fluid in the blood in order to set Marcumar correctly and to monitor it permanently. Some patients report that they feel restricted in their quality of life due to the constant blood tests and also describe severe bleeding due to the severe blood thinning.
NOAK - new oral anticoagulants
The new oral anticoagulants are drugs that act directly on blood coagulation and inhibit individual coagulation factors. These include the “factor Xa inhibitors” apixaban, rivaroxaban and edoxaban, as well as the “factor IIa inhibitors” dabigatran etexilate and argatroban. These drugs are easier to take than Marcumar's because the controls are less time-consuming. The NOAC are becoming increasingly popular for stroke prophylaxis in atrial fibrillation, but there are no long-term studies on the effectiveness of the drugs.
You can also find additional information at: Alternatives to Marcumar
What is cardioversion?
The term cardioversion describes the restoration of a normal heart rhythm (so-called sinus rhythm) in the presence of cardiac arrhythmias such as atrial fibrillation. There are two different methods of restoring a normal heart rhythm using cardioversion: electrical cardioversion using a defibrillator, also known as an electric shock, and cardioversion, which is carried out using medication.
Cardioversion using an electric shock
The electrical cardioversion, colloquially known as electric shock, is performed with the help of a defibrillator as part of a short anesthetic. This gives the heart electrical impulses that can synchronize the activity of the heart muscle cells again. The cells that no longer work in the same rhythm during atrial fibrillation are brought back into the same rhythm in this way.
Relapse prevention: The relapse rate after electrical cardioversion is up to 75% after one year. Therefore, the above-mentioned antiarrhythmics are used to prevent recurrence: Amidaron is the most effective, but associated with many side effects and contraindications. Beta blockers can also be used to prevent relapse. However, because of the risk of proarrhythmic (arrhythmia-promoting) effects, drug therapy is only rarely indicated.
ECG triggered cardioversion
Two electrodes are attached to the chest and an attempt is made to restore the heart rhythm with a direct current dose. See defibrillation (same principle). The advantage is the immediate onset of the effect and the avoidance of drug side effects, the disadvantage is the higher burden on the patient and the greater risk of embolic complications (e.g. stroke).
Drug cardioversion
In addition to electrical cardioversion, drug therapy can also be used for atrial fibrillation. This form of cardioversion can be used without anesthesia and, under certain circumstances, even performed by the patient himself. Commonly used drugs include amiodarone, flecainide and ajmaline.
In patients without an underlying heart disease, this is done with class I antiarrhythmics.
Patients with heart disease are usually treated with amiodarone - a class III antiarrhythmic. Therapy is always carried out under inpatient control.
Patients who only have intermittent disorders may, after training with a "pill in the pocket“To be equipped. You then simply take your tablet when necessary, provided that your heart is healthy.
How safe are you after cardioversion?
Electrical cardioversion is used to restore a normal sinus rhythm in the heart muscle cells in the case of atrial fibrillation. The activity of the cells is synchronized and the pulse rate becomes stable. Depending on the cause of the atrial fibrillation, relapses, i.e. renewed atrial fibrillation, can occur after cardioversion. The probability is about 50%, so that every second patient gets atrial fibrillation again and the pulse becomes unstable. Therefore, after an electrical cardioversion, treatment should be initiated to prevent further cardiac arrhythmias, which consists of antiarrhythmic drugs.
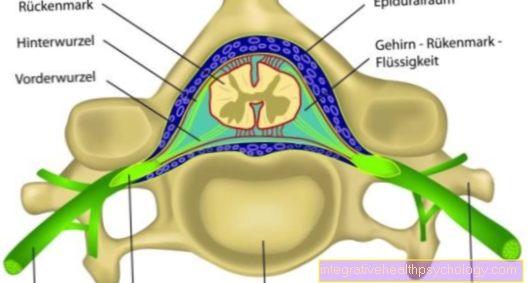
Pacemaker
Pacemakers are used to treat a slow heart rate or atrial fibrillation, for example. The pacemaker provides the heart with regular electrical stimulation that prevents atrial fibrillation from occurring. Whether a pacemaker is necessary depends on the cause of the atrial fibrillation.
ablation
Ablation on the heart is a treatment in which excess or diseased sources of excitation are obliterated in order to permanently eliminate cardiac arrhythmias. By exposure to cold or heat, scars are set in the heart muscle tissue during the ablation so that the muscle excitations are suppressed, which cause additional unhealthy excitations.
Ablation is used on the heart for atrial fibrillation when the arrhythmia does not improve despite drug therapy. Patients benefit for whom conventional medication does not help to restore a normal heart rhythm.
Cardiac catheter
The heart catheter examination is a procedure that can reveal pathological changes in the coronary arteries, the heart valves and the heart muscle. A thin plastic tube, the heart catheter, is inserted through blood vessels in the groin or arm and advanced to the heart. The cardiac catheter enables you to measure electrical activities in detail in the event of arousal disorders. Cardiac catheterization can help assess the heart in atrial fibrillation and provides options for minimally invasive treatment, e.g. with ablation, then one speaks of a "catheter ablation".
For more information, see: Diagnosis of coronary artery disease
Alternative therapies to atrial fibrillation
The treatment of atrial fibrillation is the subject of current research and is constantly evolving. For a few years now there has been the option of ablation therapy (sclerotherapy) to eliminate the origin of the atrial fibrillation in persistent and seizure atrial fibrillation when medication is no longer effective. In this process, high-frequency current (so-called radio frequency ablation) is used to set sclerotherapy points in order to switch off the flicker waves during atrial fibrillation, namely in the pulmonary vein muscles near the atrium (known as pulmonary vein isolation, PVI).
Since 2014 there has been another innovative method for the treatment of paroxysmal (attack-like) and persistent (persistent) atrial fibrillation, the so-called pulmonary vein isolation with a cryoballoon. This therapy for atrial fibrillation has so far proven to be safe and effective. So-called cold ablation is used instead of a high-frequency current in order to achieve better clinical effectiveness.
Support with homeopathy
Self-medication is generally not advisable for atrial fibrillation. If you want to use globules in addition to or instead of medication, you should discuss this with your family doctor and cardiologist. With atrial fibrillation, the heart beats too quickly, so that Tabacum (D30, 8 globules twice a day) in combination with Cactus (3 times a day 8 globules) can have a positive effect on the heartbeat, according to alternative practitioners.
It does no harm also to reduce the risk factors for atrial fibrillation.
Diabetes is considered to be a major risk factor, which means that there is a benefit in keeping blood sugar low. It is the same with high blood pressure, since a permanently high blood pressure damages the heart and blood vessels. Homeopathic globules for high blood pressure are Aurum metallicum and Arnica. To check the blood sugar level e.g. Lowering diabetes mellitus is popular in homeopathy Syzygium jambolanum taken. Nonetheless, atrial fibrillation is a serious condition that requires medical attention.
Schuessler salts - are they helpful?
In the case of cardiac arrhythmias such as atrial fibrillation, the Schüßler Salt No. 7 Magnesium phosphoricum is used. 10 small balls of the Schuessler salt are added to about 100 ml of hot but not boiling water in a cup and sipped. 10 pieces should be taken in the morning and 10 in the evening. In the case of atrial fibrillation, the therapy should be discussed with the family doctor and cardiologist.
Guidelines for the therapy of atrial fibrillation
The guidelines of the German Society for Cardiology (DGK) provide guidelines for the treatment of atrial fibrillation. In order to make the diagnosis of suspected but undocumented atrial fibrillation, heart rhythm monitoring may be necessary to determine the type of atrial fibrillation. In the chronic disease, atrial fibrillation, there are different types of disease that require different treatment. In long-term treatment, the German Cardiac Society recommends, depending on the type and symptoms of atrial fibrillation, the consideration of antithrombotic therapy (blood-thinning), rate-regulating and rhythm-maintaining treatment. Depending on the cause of the atrial fibrillation, treatment for the underlying heart disease may be necessary.
Where can I find the guidelines?
The guidelines of the German Society for Cardiology are publicly available.They can be found on the DGK website (https://leitlinien.dgk.org/stichwort/vorhofflimmern/) and can be requested in writing from the DGK. The attending cardiologist is responsible for applying the guidelines for the treatment of atrial fibrillation.