The low platelet count - when does it become dangerous?
introduction
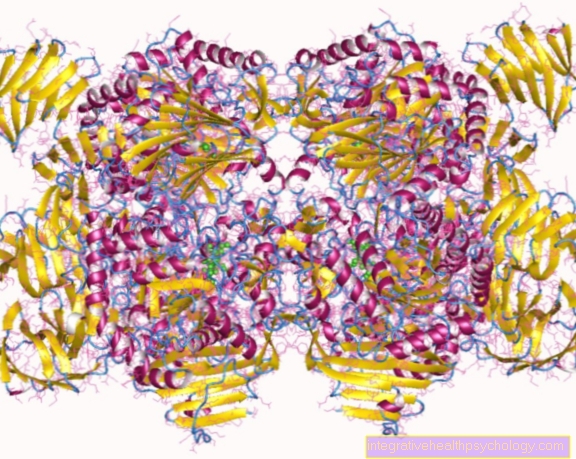
Platelets are components of the blood, which are also known as platelets. They perform an important role in blood clotting by being responsible for closing the vessels in the event of injuries.
The number of platelets can be determined from a small blood count and may occasionally be decreased. If the value of the platelets in the blood has fallen below the normal value, one speaks of thrombocytopenia or thrombopenia. The causes for this can be very different. On the one hand, the lack of platelets in the blood can arise because the body does not produce enough new platelets or the existing platelets are increasingly broken down.
If the number of platelets is only slightly lower than the normal value, it can usually be tolerated and compensated for by the human body as long as there are no other diseases. However, if the number of platelets has fallen far below the normal value, this can lead to heavy bleeding, even with minor injuries.

The reasons
A low number of platelets in the blood can have many different causes. As a rule, the deficiency is due to a disturbed formation of new platelets or an increased breakdown of these.
A restricted formation of platelets can arise, for example, from a congenital disorder and is usually diagnosed at a young age. However, the educational disorders can also develop in the course of life. The reason for this can be a bone marrow disease, such as leukemia, or bone marrow damage caused by drugs, toxic substances, radiation or tumors. A deficiency in vitamin B12 or folic acid can also be responsible for a decrease in the number of platelets in the blood, as these important nutrients are no longer available for platelet formation in the event of a deficiency.
If an increased breakdown is responsible for the lack of platelets, the cause can be, for example, clotting activation or a reaction with antibodies. Mechanical damage to the platelets by artificial heart valves, for example, can also be a cause of increased breakdown of platelets.
Pseudothrombocytopenia occurs when the platelets are incorrectly measured too low in the laboratory sample, but are present in normal numbers in the patient.
Find out all about the topic here: The causes of thrombocytopenia.
Chemotherapy as the cause
Chemotherapy is a treatment with so-called cytostatics (= cell-killing agents). These cytostatic agents are chemical substances that are particularly intended to kill the pathologically altered cells. Physical radiation, so-called radiotherapy or hormone therapy, should also serve the purpose of causing diseased cells to die.
Unfortunately, all of these treatments can also induce the death of healthy cells as a side effect. Among other things, this can also affect blood components such as platelets. Since the platelets are responsible for blood clotting, a drop in platelets can show that even the smallest injuries lead to major bleeding. Therefore, the number of platelets during chemotherapy is measured and checked at regular intervals.
Find out more about the side effects of chemotherapy.
The HIT as the cause
The abbreviation HIT stands for heparin-induced thrombocytopenia.When patients take the drug heparin, various reactions in the body can lead to a drop in platelets. One speaks of HIT if the number of platelets has fallen to less than 50% of the initial value before starting therapy with the drug.
A distinction is made between two types, HIT type 1 and HIT type 2. HIT type 1 is usually the relatively harmless form, as the platelets only react directly with the drug heparin. The clinically less favorable form is HIT type 2. With this type, antibodies are formed in the body and thus platelets clump together. This clumping can lead to thrombosis, for example.
Since there is always the risk of HIT in patients with heparin, a baseline platelet value should be determined before starting therapy and this should then be checked at regular intervals.
Read more about this topic here: Heparin-induced thrombocytopenia.
Werlhof's disease as the cause
Werlhof's disease, also known as Werlhof's disease, is an autoimmune disease in which antibodies in the human body are directed against its own platelets. If the antibodies formed bind to the body's own platelets, these are broken down in the spleen. This leads to a lack of platelets in the blood. The platelets are no longer able to do their job of clotting the blood as well and there may be a tendency to bleed.
The cause of Werlhof's disease has not yet been clarified, symptoms are often found in patients after a viral infection of the upper respiratory tract, which is why this is being discussed as a possible cause. The severity of the disease can vary widely and sometimes develop without any clinical symptoms.
For more information, see: Werlhof's disease.
The symptoms
The symptoms of a platelet deficiency can be very diverse. A prolonged bleeding time, for example, can indicate a reduced number of platelets. Many and very pronounced hematomas ('bruises') after harmless injuries can also indicate this.
If bleeding occurs in internal organs, which cannot be stopped due to the lack of platelets, symptoms may include bloody stool or urine. Petechiae (the smallest bleeding in the skin) are also an indication of a platelet deficiency. These can usually be found on the arms and legs and appear as the smallest, red, scattered dots. It is characteristic of these petechiae that they cannot be pushed away by finger pressure.
The bleeding
Since platelets take on the function of clotting the blood in the body, a deficiency in these blood components often poses a risk of bleeding. The more pronounced the deficiency, the more severe the bleeding. If there is a pronounced platelet deficiency, these can arise from even the smallest injuries to the skin or mucous membranes. Injuries to the internal organs can also lead to profuse internal bleeding. Bleeding should always be stopped as quickly as possible, as major loss of blood can lead to a life-threatening condition.
What's the quickest way to stop bleeding? Find out more here.
The petechiae
Petechiae are the smallest hemorrhages in the skin or mucous membrane that can occur due to a lack of platelets. They are characterized as red, punctiform hemorrhages and are about the size of the head of a pin. They do not appear singly, but in larger groups.
The lower legs and ankles are usually affected by petechiae first. Places where they usually occur are also the mucous membranes or the head. The forearms and torso can also be affected. A typical feature of the petechiae is that they cannot be pushed away by pressing with the finger.
The consequences
The consequences of a reduced number of platelets can be very different. In general, a distinction must be made between how much the number of platelets deviates from the normal value. The period in which the number of platelets in the blood has decreased is also important for the consequences.
If the values are only slightly lower than the normal value, then it usually proceeds without clinical symptoms for the patient. However, if the number of platelets is significantly reduced, this can lead to even harmless injuries, for example to the skin, leading to major bleeding. This can often be recognized by hematomas (= bruises ‘). These are then usually very large and distinct.
Petechiae (= the smallest bleeding) can also appear on the legs and arms, for example. These petechiae appear as small, juxtaposed red dots that cannot be pushed away by finger pressure. Bleeding gums or nosebleeds can also occur more frequently. Even the smallest of injuries, such as brushing a toothbrush or blowing your nose, can be enough to cause bleeding.
Black stools or bloody urine can indicate that there is internal bleeding.
The laboratory values
The number of platelets is determined by a small blood count. To do this, a blood sample is taken and the platelet count per µl of blood is measured. Normal values are in the range of 150,000 - 380,000 platelets per µl of blood. This range, in which the normal values should be, applies to both women and men.
If the laboratory value is between 100,000 and 150,000 platelets per µl of blood, this usually does not indicate any clinical symptoms. If the laboratory value is less than 100,000 platelets per µl of blood, symptoms often appear in the form of a prolonged bleeding time, spontaneous bleeding or the smallest bleeding that occurs more frequently on the arms and legs.
The treatment
Treatment for reduced platelet counts depends on the cause and severity of the disease.
If there is a slight deficiency of platelets in the blood, no further treatment is often required, as this condition is usually normalized again by the body's own processes.
If the reason for the platelet deficiency is a lower formation of new platelets or an increased breakdown of platelets, this cause should be eliminated first. The therapies here are very different depending on the underlying disease. If blood-thinning medication is taken, these are often stopped first so that blood clotting improves somewhat. If no medication is taken or the platelet deficiency is very acute and severe, this blood loss should be compensated for as soon as possible. Blood reserves can be given. The administration of a platelet concentrate can significantly improve the coagulation of the blood again. In the event of an injury, the bleeding can be stopped more quickly and there is less blood loss. An erythrocyte concentrate can also be administered at the same time, as this can improve the coagulation of the blood in the body in addition to the platelet concentrate.
Find out all about the topic here: The blood transfusion.
The duration and forecast
The duration of a platelet deficiency can vary greatly depending on the cause. It is important that the causal factor is eliminated and the formation of new platelets proceeds normally. If the platelet deficiency is only pronounced for a short period of time and is not accompanied by any further clinical symptoms, no consequential damage is to be expected.
If the formation of platelets is still restricted, they should be replaced with platelet concentrates in the event of a severe deficiency, as otherwise there is a risk of life-threatening bleeding.
The course of the disease
The course of the disease in a patient with low platelets can range from clinically normal to life-threatening. If the number of platelets falls, this can be represented by an ever increasing bleeding time. The size of the injuries that lead to bleeding is getting smaller and smaller. Injuries that would otherwise be harmless can lead to insatiable bleeding and large blood loss.
Petechiae, the smallest bleeding in the vessels or spontaneous bleeding can occur. When associated with a large loss of blood, it can be a life-threatening condition.
When does it get dangerous?
For the prognosis of a platelet deficiency it is fundamentally important which symptoms the patient shows. Usually a slight decrease in the values can be tolerated and compensated for by the human body. However, if bleeding times are significantly prolonged or even spontaneous bleeding occurs, it can mean a life-threatening condition for the patient.
Due to the reduced number of platelets, the body's own blood clotting does not work or does not work as well and the bleeding can no longer be properly stopped. A doctor should be consulted, especially in the case of major bleeding, which can also affect internal organs. Symptoms suggestive of internal bleeding could include bloody or black stools and urine.
Also read the article: The gastrointestinal bleeding.
Can that also be cancer?
If a platelet deficiency is diagnosed, leukemia is one of the possible causes. Leukemia is a disease of the blood or blood-building system. In the broader sense, it belongs to the cancer diseases and is popularly referred to as (white) blood cancer. The disease is an increased formation of certain blood cells in the bone marrow. Platelets are also formed in the bone marrow by precursor cells. If there is now an increased formation of other cells, the formation of new platelets often decreases. As a result, the blood levels may be too low.
A tumor that originates from another tissue and presses on the bone marrow could also restrict the formation of new platelets and lead to a reduced number in the blood.
Find out more about Tumor diseases.
Decreased platelet and white blood cell counts
If both the platelet count and the leukocyte count in the blood are low, this can be due to several causes. Since both cells in the bone marrow are made from precursor cells, leukemia (also known as white blood cancer) can be a cause. It is a disease that restricts the function of the bone marrow and thus can lead to impaired formation of the blood components.
Chemotherapy and radiation also damage the bone marrow and can lead to a reduction in both blood components. An increased breakdown of platelets and leukocytes can also be a cause. The reason for this could be, for example, an overactive spleen.
Also read the article: The leukemia.















.jpg)