Cortisone preparations
Synonyms
- chronic inflammatory diseases
- Cortisone tablets
- Cushing threshold dose,
- Dexamethasone
- Low-dose therapy
- Neurodermatitis
- Prednisone
- Prednisolone
- rheumatic diseases
introduction
Cortisone preparations (Glucocorticoids) are among the most important drugs in the treatment of many acute and chronic inflammatory diseases today. They are very effective drugs that are now available in various forms and enable targeted therapy. In the case of chronic inflammatory diseases, cortisone tablets in particular can have a positive effect on the course of the disease and restore the quality of life to those affected.

application areas
Cortisone can be used in many ways. For example, inflammatory skin diseases are available for local therapy Cortisone ointments/ creams available. Applied to the diseased skin area, it effectively combats the inflammation and promotes the healing process. Cortisone can also be administered as a syringe, e.g. in inflammatory joint diseases. In the therapy of asthma Cortisone sprays for inhalation play an important role and have a positive effect on the course of the disease. Cortisone can still be given in tablet form. These are often only used in the case of severe disease processes in which the therapy of the underlying disease and the local administration of Glucocorticoids hardly have any effect. The effect of cortisone consists in the suppression of inflammatory processes as well as exaggerated immune reactions. Inflammations are part of many diseases and, depending on their severity, can severely reduce the quality of life of those affected. Targeted treatment with cortisone effectively combats inflammation and the associated symptoms are reduced. But cortisone does not fix the cause of the disease! However, the healing process can be improved by treating the side effects (Symptoms) can be positively influenced.
Systemic therapy
In the case of some inflammatory diseases with a chronic course, basic therapy and the local application of cortisone are often insufficient. For example, in skin diseases such as neurodermatitis, where deep layers of the skin can also be inflamed, the active ingredient from a cream cannot penetrate deep enough. The use of cortisone tablets can help here. The active ingredient enters the bloodstream via the gastrointestinal tract and is transported from there to diseased areas. One speaks of a systemic effect. Cortisone tablets can be used on the one hand as short-term therapy to treat a disease flare-up. On the other hand, depending on the severity of the disease, regular intake as part of long-term therapy may be necessary in order to prevent a disease flare-up.
Cortisone is also used as a form of therapy for children. For more information, see: Cortisone in the child
Examples: Conditions in which cortisone is given systemically
- severe forms of eczema
- lupus erythematosus
- fast-moving, destructive rheumatoid arthritis
- chronic polyarthritis
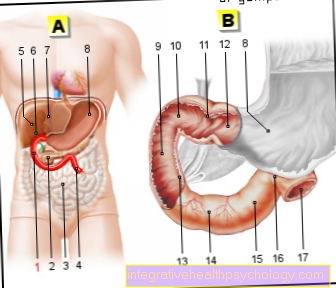
- Ulcerative colitis, Crohn's disease
- Multiple sclerosis flare-up
- Substitution therapy for Addison's disease
Systemic cortisone therapy can also be carried out using infusions. Glucocorticoids are injected directly into the bloodstream. This means that the active ingredient is available even faster.
dosage
Cortisone is an endogenous hormone and regulates many processes in the body (see cortisone). Supplied to the body from the outside as a drug, it intensifies the effect of the body's own cortisone. Inflammatory processes and the overreactivity of the immune system are inhibited and the associated symptoms are reduced. As part of short-term therapy (approx. 2 weeks) to treat a flare-up, a high dose is administered in the first few days, which is reduced further over the course of the treatment days. One also speaks of a gradual dosage. As part of long-term therapy, your doctor will choose the smallest possible but most effective dosage with which your disease can be easily controlled and causes as few side effects as possible (low-dose therapy).
The entire daily dose can either be taken all at once at a certain time of the day, usually in the morning between 6-8 a.m. (circadian rhythm). This is when the body's own cortisone production is at its highest. The daily dose can also be divided into several daily profile-dependent units. Please do not change your dosage yourself or stop the therapy abruptly! This could jeopardize the success of the treatment and cause undesirable side effects. Should you have any questions about the intake or should problems arise, let the doctor treating you advise you!
Side effects
Side effects a cortisone therapy (please refer Cortisone therapy for asthma) usually arise when the dose administered from the outside is for a long time many times higher than the body could provide. A single high dose is harmless. The risk of undesirable side effects occurring is also low with a treatment period of 2 weeks. Glucocorticoids are not fast-acting drugs. Because they control gene regulation, the effect is delayed but all the more lasting. Side effects are closely related to the natural function of the glucocorticoids. A high dose taken over a long period of time has the desired therapeutic effect in particularly serious diseases. Inflammatory processes are inhibited, that immune system prevented from an exaggerated reaction and the patient becomes symptom-free. But other metabolic processes can also be influenced, which can have undesirable consequences.
If the body is supplied with a high dose of glucocorticoids from the outside over a longer period of time, the Adrenal gland downregulates the body's own production. However, this can also impair metabolic processes that are controlled by hormones produced in the kidney. In that context it can be too high blood pressure come. Furthermore, an oversupply of cortisone in the body promotes the breakdown of body reserves for blood sugar. If this cannot be dismantled quickly enough, it happens diabetes. In this context, watch out for an increased feeling of thirst and an increased urge to urinate. Too much cortisone can also have a negative effect on fat metabolism. The result would be weight gain. Therefore have an eye on a balanced one nutrition. In connection with long-term use of cortisone, a osteoporosis arise. The suppressive effect of glucocorticoids on the immune system reduces the resistance to pathogens. Patients treated with cortisone often show an increased susceptibility to infections. Occasionally there are psychological changes such as euphoria or depressions.
In the context of long-term therapy, as it is often carried out in addition to the basic therapy in the case of more serious, chronic illnesses, the benefits and risks must be weighed against each other. Of all cortisone preparations, the intake of cortisone tablets carries a relatively higher risk of undesirable side effects (systemic effects). In the case of many serious illnesses, one has to weigh up whether the possible side effects of cortisone therapy are more serious than the consequences of (untreated) Underlying disease. Often the Cortisone side effects Considered the "lesser evil" compared to the underlying disease, especially because of the Cortisone therapy the course of the disease can be significantly positively influenced.
When do side effects occur?
The so-called Cushing threshold dose is used to measure when therapeutically used glucocorticoids can produce side effects. The name goes back to a disease (Cushing's syndrome). The symptoms of Cushing's syndrome are the result of an excess of cortisone in the body.
Read more on this topic at: Symptoms of Cushing's Syndrome
Just these "typical cortisone“Side effects can also occur with an excessively high dose of cortisone therapy. The Cushing threshold dose indicates the amount of active ingredient taken daily as part of long-term use "typical cortisone“Concomitant symptoms, as they appear in Cushing's syndrome, causes. However, this is only a rough guide. This varies depending on age, gender and the form of the disease.
Further information can be found at: What is the Cushing Threshold?
Active ingredients and preparations
Active ingredient Cushing threshold dose [mg / day] preparations
Betamethasone 1 Celestamine®
Dexamethasone 1.5 Dexa-CT®, Dexamethason GALEN®
Fluocortolone 7.5 Ultralan®-oral
Hydrocortisone 30 Hydrocortisone Hoechst®, Hydrocutan®
Methylprednisolone 6 Urbason®, M-PredniHEXAL®, Metysolon®
Prednisolone 7.5 Decortin®, Dermosolon, PredniHEXAl®
Prednisone 7.5 Decortin®, PrednisolHEXAL®
Triamcinolone 6 Delphicort®, Volon®











.jpg)